3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2011; 8(3):216-221. doi:10.7150/ijms.8.216 This issue Cite
Research Paper
Effects of Flurbiprofen on CRP, TNF-α, IL-6, and Postoperative Pain of Thoracotomy
1. Department of Thoracic Surgery, Konya Education and Research Hospital, Konya, Turkey;
2. Microbiology Laboratory, Konya Education and Research Hospital, Konya, Turkey
Received 2011-1-5; Accepted 2011-3-6; Published 2011-3-10
Abstract
Objective: The aims of this study were to evaluate serum levels of acute phase reactants, such as CRP and cytokines (TNF-α and IL-6) in patients who have undergone thoracotomy and to investigate the effects of flurbiprofen on postoperative inflammatory response.
Methods: Forty patients undergoing posterolateral thoracotomy were randomly divided into 2 groups of 20 each. Control group received tramadol (4 x 100 mg) intravenously for four days, and flurbiprofen group received both tramadol (4 x 100 mg) and flurbiprofen (2 x 100 mg). Blood samples were collected before surgery and at the 3th and 168th hours after surgical procedure to measure serum CRP, IL-6, and TNF-α. Pain visual analog scales were recorded daily during the first four postoperative days. Spirometric measurement of forced expiratory volume in the first second (FEV 1) was done before and four days after the operation.
Results: The serum CRP, IL-6, and TNF-α levels in both groups increased significantly at 3th hour after thoracotomy. Serum TNF-α levels did not differ significantly between the groups at postoperative 4th day. However, IL-6 and CRP were significantly lower in flurbiprofen group than in control group at the same day (p<0.05). Visual analog scale was significantly lower in flurbiprofen group at 6th, 12th, 48th, 72th, and 96th hours postoperatively (p<0.05). The patients receiving flurbiprofen had higher FEV 1 values when compared with control group at postoperative 4th day.
Conclusions: Patients undergoing thoracotomy showed reduced postoperative pain, mean additional analgesic consumption, and serum IL-6 and CRP levels, when flurbiprofen was added to systemic analgesic therapy. Analgesia with anti-inflammatory drug may contribute to the attenuation of the postoperative inflammatory response and prevent postoperative pain in patients undergoing thoracotomy.
Keywords: Thoracotomy pain, Inflammatory response, Flurbiprofen
Introduction
Surgical trauma induces an inflammatory state characterized by the release of both proinflammatory and antiinflammatory proteins. Proinflammatory cytokines induce not only a local inflammation at the site of injury, but also systemic responses such as tachycardia, tachypnea, leukocytosis, and pyrexia (1). Increased levels of proinflammatory cytokines are also associated with a higher incidence of postoperative infections and respiratory failure (2-4). Attenuation of the inflammatory response can reduce injury-induced immunosuppression and is linked to functional recovery (5).
Nonsteroidal antiinflammatory drugs (NSAIDs) are useful in pain states, and work by inhibiting the cyclooxygenase enzyme responsible for the release of mediators of inflammation (6). The aims of this study were to evaluate the serum levels of acute phase reactants, such as C-reactive protein (CRP), and cytokines (interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α)) in patients with thoracotomy and to investigate the effects of flurbiprofen on postoperative inflammatory response.
Material and Methods
Eligibility criteria
Forty patients undergoing elective lung resection were included in this double-blind, randomized study. Ethical approval was provided by the ethics committee of Meram Medical School, Selcuk University, Konya, Turkey, and all patients gave their written informed consent to participate in the study. Exclusion criteria of the patients were as follows: history of severe heart disease (New York Heart Association class IV heart failure within the six months before enrollment) or hepatic (Cirrhosis) or renal failure (Chronic kidney disease need for renal replacement therapy) or peptic ulcus, American Society of Anesthesiology class IV or higher, patients undergoing resection of the pleura or chest wall, and patients with hemorrhagic diathesis or medication of anticoagulants, corticosteroids, and acetylsalisilic acid.
The surgical approach in all the patients was a posterolateral thoracotomy through the 5th intercostals space, usually extended from the midscapular to the anterior axillary line for a length ranging between 12 and 15 cm.
Experimental protocol
Two randomized groups of 20 patients each were compared. The baseline pain medication in both groups was tramadol (4 x 100 mg) intravenously for four days. Control group received tramadol (4 x 100 mg) intravenously for four days and flurbiprofen group received both tramadol (4 x 100 mg) and flurbiprofen (2 x 100 mg). Paracetamol 1000 mg was administered as an additional analgesic, if required, for two groups.
Postoperative care
Demographic information, visual analog pain scores, pulmonary function tests, and supplementary intravenous analgesia were recorded for each patient. Patients subjectively assessed the level of pain at 1th, 6th, 12th, 24th, 48th, 72th, and 96th hours after surgery by a visual analogue scale (VAS) with scores ranging between 1 (pain free) and 10 (the worst imaginable pain). Pulmonary function parameter including forced expiratory volume in the first second (FEV 1) was performed preoperatively and at postoperative 4th day. Operation time, number of chest tubes, length of hospital stay, and postoperative complications were recorded in all patients.
Measurement of inflammatory mediators
Blood samples were collected before surgery and at 3 and 96 hours after surgical procedure to measure serum CRP, IL-6, and TNF-α levels. Peripheral venous blood samples were collected into the blood collector tubes (Vacuette, Greiner Bio-One GmbH Baden-Württemberg, Germany) and than centrifuged at 4.500 rpm for 10 minutes (Eppendorf Centrifuge 5702, Eppendorf Ag, Hamburg Germany), and sera samples were obtained. All the following laboratory assays were performed by using obtained sera; high sensitive CRP (mg/L), IL-6 (pg/mL) and TNF-α (pg/mL). High sensitive CRP mesurement performed with nephelometric method (reactive: Dade Behring GmbH Marburg, Germany, device: BN II Dade Behring GmbH Marburg, Germany), IL-6 (Invitrogen Corp. CA, USA) and TNF- α (Invitrogen Corp. CA, USA) assays performed by using enzyme linked immuno sorbent assay method (ELISA) (Tecan Minilyser, Tecan Group Ltd. Mannedorf, Switzerland). IL-6 and TNF- α assay mesurements were carried out at 450 nm optical density (OD).
Statistical analysis
All parametric results were expressed as mean ± standard deviation for each group. Statistical analysis was performed with SPSS 15.0 software. Fisher's exact test was used to analyze between-group differences in categorical variables. Student's t-test was used to assess between-group differences in continuous variables. A p-value less than 0.05 was considered to be statistically significant.
Results
Forty patients fulfilled the study criteria and were therefore included in the trial. All patients underwent lung resection either for lung cancer or benign disease. There were no significant differences between groups regarding age, sex, reasons of thoracotomy, preoperative FEV 1, number of chest tubes, operation time, and postoperative blood loss (Table 1).
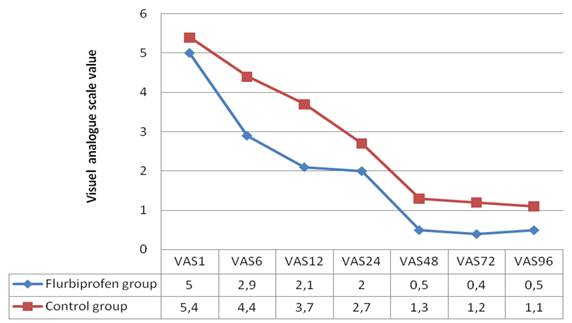
Visual analog scale was significantly lower in flurbiprofen group at 6th, 12th, 48th, 72th, and 96th hours postoperatively (p<0.05) (Figure 1). Mean additional analgesic consumption (paracetamol clorhydrate, 1000 mg infusion solution) in the 96th hour after surgery was 775 mg for control group and 200 mg for flurbiprofen group. There were significant differences between control and flurbiprofen groups (p<0.05).
Patient characteristics, reasons for thoractomy, and surgical information
| Flurbiprofen group | Control group | |
|---|---|---|
| Median age (years) | 55.3 | 50.4 |
| Sex ratio (M/F) | 13/7 | 12/8 |
| Preoperative FEV1(% predict) | 65.6 | 64.6 |
| Number of chest tubes (1/2 tube) | 9/11 | 6/14 |
| Operation time (min) | 150 | 156 |
| Postoperative blood loss (ml) | 266 | 249 |
| Adenocarcinoma (n) | 5 | 4 |
| Squamous carcinoma (n) | 7 | 5 |
| Large cell carcinoma (n) | 1 | 3 |
| Carsinoid tumor (n) | 0 | 1 |
| Bronchiectasis (n) | 4 | 4 |
| Hydatid cyst (n) | 1 | 1 |
| Metastasis (n) | 2 | 2 |
Postoperative pain scores as assessed by Visual Analogue Scale in the study groups.
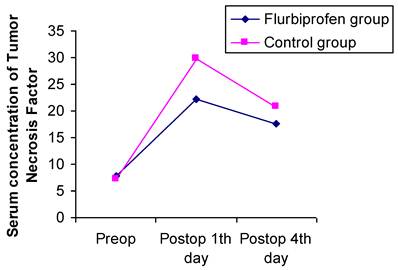
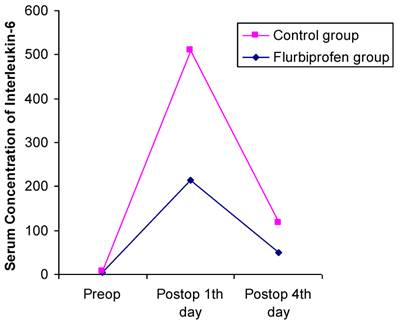
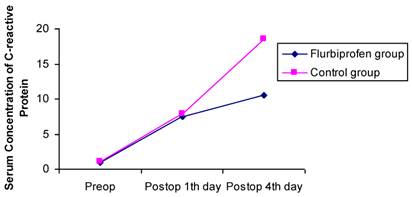
Postoperative increases in serum CRP, IL-6, and TNF-α concentrations were observed in both groups. The CRP value peaked on the postoperative 4th day in the control group whereas IL-6 and TNF-α values peaked on the postoperative 1th day in both groups. Serum CRP, IL-6, and TNF-α levels did not differ significantly between the groups at preoperative and postoperative first day. Serum TNF-α levels were not significantly different between the groups at postoperative 4th day. However, IL-6 and CRP were significantly lower in flurbiprofen group than in control group at postoperative 4th day (Figure 2,3,4).
Mean postoperative length of hospital stay was 8.0±2.2 days in control group and 6.8±1.9 days in flurbiprofen group. There were no significant differences between the both groups (p=0.077). Mean postoperative (%) FEV 1 was 49.7±7.2 in control group and 55.6±6.7 in flurbiprofen group. There were significant differences between the both groups (p<0.05). No major complication occurred in any groups. Prolonged chest tube drainage occurred in one patient in the flurbiprofen group. Atelectasis occurred in one patient belonging to the control group and it was recovered by respiratory rehabilitation and bronchoscopic aspiration. Gastrointestinal side effects, mostly nausea and vomiting, were determined as the most common events in both groups. No patients in both groups discontinued the study because of severe side effects (Table 2).
Changes in serum concentration of TNF-α before and after thoracotomy in the study groups.
Changes in serum concentration of IL-6 before and after thoracotomy in the study groups.
Changes in serum concentration of CRP before and after thoracotomy in the study groups.
Side effects and complications in the postoperative period.
| Side effects | Flurbiprofen group (n, %) | Control group (n, %) |
|---|---|---|
| Prolonged chest tube drainage | 1(5) | - |
| Atelectasis | - | 1 (5) |
| Nausea/vomiting | 9 (45) | 7 (35) |
| Constipation | 2 (10) | 3 (15) |
Discussion
Thoracotomy for lung resection represents a major surgical stress, and is associated with a significant increase in the postoperative circulating levels of plasma inflammatory markers (7). Our results showed that the levels of serum CRP, IL-6, and TNF-α were high in all patients after surgery, and that CRP and IL-6 elevations were significantly less pronounced in the group using anti-inflammatory drug than control group. In addition, patients in the flurbiprofen group experienced less severe postoperative pain, whereas those in the control group reported higher VAS scores and additional analgesic consumption. These findings may be related to the antiinflammatory effects of flurbiprofen.
VAS scoring is a simple and often used method for evaluating variations in pain intensity. Subjects are instructed to indicate the intensity of the pain by marking a 100-mm line anchored with terms describing the extremes of pain intensity. VAS scoring was a valid measure of pain in the early postoperative period (8). VAS scoring was used for evaluating acut postthoracotomy pain in different studies (9-12).
Systemic cytokine response induced by surgical damage has been reported and is thought to have an important effect on the immune system. IL-6 and TNF-α are major mediators of the acute-phase protein response to tissue damage caused by surgical intervention (13-15). CRP is an acute phase reactant; it is a marker of inflammation and produced in the liver on stimulation by monocyte related cytokines, such as IL-6 and TNF-α. (16,17). Among the human body responses to surgery, the serum IL-6 level is reported to be a sensitive indicator of the degree of surgical stress (13-15). Furthermore, it has been reported that postoperative IL-6 levels correlate with postoperative complications and mortality (18). Many reports confirm our finding that IL-6 concentration in the control group on postoperative first day after pulmonary resection over 100 pg/ml (2,19,20).
While IL-6 level reached to the peak level at the postoperative first day in the both group, it was found statistically lower at flurbiprofen administrated group comparing with control group on postoperative 4th day. While the IL-6 levels determined at reference value in flurbiprofen group, it was remained over reference range in control group at postoperative 4th day. While TNF-α measurement reached to the peak level in both group on postoperative 4th day, levels of TNF- α were determined relatively lower at flurbiprofen group comparing with control group. In addition to this, there was no significant difference between two groups. Serum CRP level was significantly lower in flurbiprofen group than in control group at postoperative 4th day.
Pain control is a significant concern in hospitalized patients, with many clinicians now considering pain to be the fifth vital sign (21). Colacchio et al. (22) reported that ketorolac may be an effective agent for restoring perioperative immune competence, whereas the use of continuous morphine might have significant deleterious effects. Torres et al. (23) reported that postoperative pain after abdominal surgery in which dipyrone administered via patient controlled analgesia pumps had the same analgesic efficacy with less adverse effects than buprenorphine and morphine. Although in most cases NSAIDs can control postoperative pain after ambulatory surgery, NSAIDs alone are usually insufficient during the early postoperative period in hospitalized patients undergoing major surgical procedures (24). NSAIDs are associated with inhibition of platelet aggregation, gastrointestinal bleeding, and renal toxicity, limiting their usefulness in clinical practice. The incidence of these side effects are rare, however, patients with preexisting peptic ulcer disease and renal impairment are at greater risk. Careful patient selection, therefore, would seem to be the prudent course of action when choosing these agents perioperatively.
Lung volumes after thoracic surgery may be reduced by up to 50%, and aggressive analgesic therapy leads to improvements in pulmonary function not observed with standard therapy (25-27). The pain relief in the flurbiprofen group resulted in better function with higher postoperative FEV1. When comparing preoperative and postoperative measured FEV 1 values, 24 % and 16 % decreases determined at control and flurbiprofen groups, respectively.
In conclusion, we observed that patients undergoing thoracotomy showed reduced postoperative pain, mean additional analgesic consumption, and serum IL-6 and CRP levels, when flurbiprofen added to the systemic analgesic therapy. Analgesia with antiinflammatory drug may contribute to the attenuation of the postoperative inflammatory response and prevent postoperative pain in patients undergoing thoracotomy.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Andres BM, Taub DD, Gurkan I. et al. Postoperative fever after total knee arthroplasty: the role of cytokines. Clin Orthop Relat Res. 2003;415:221-31
2. Yamada T, Hisanaga M, Nakajima Y. et al. Serum interleukin-6, interleukin-8, hepatocyte growth factor, and nitric oxide changes during thoracic surgery. World J Surg. 1998;22:783-90
3. Katsuta T, Saito T, Shigemitsu Y. et al. Relation between tumor necrosis factor alpha and interleukin 1 beta producing capacity of peripheral monocytes and pulmonary complications following oesophagectomy. Br J Surg. 1998;85:548-53
4. Takeda S, Takeda S, Kim C. et al. Preoperative administration of methylprednisolone attenuates cytokine-induced respiratory failure after esophageal resection. J Nippon Med Sch. 2003;70:16-20
5. Hall GM, Peerbhoy D, Shenkin A. et al. Relationship of the functional recovery after hip arthroplasty to the neuroendocrine and inflammatory responses. Br J Anaesth. 2001;87:537-42
6. Soto RG, Fu ES. Acute Pain Management for Patients Undergoing Thoracotomy. Ann Thorac Surg. 2003;75:1349-57
7. Avdagic SS, Krdzalic G, Avdagic H. et al. Effects of postoperative analgesia on acute phase response in thoracic surgery. Med Arh. 2010;64:113-5
8. DeLoach LJ, Higgins MS, Caplan AB. et al. The visual analog scale in the immediate postoperative period: intrasubject variability and correlation with a numeric scale. Anesth Analg. 1998;86:102-6
9. D'Andrilli A, Ibrahim M, Ciccone AM. et al. Intrapleural intercostal nerve block associated with mini-thoracotomy improves pain control after major lung resection. Eur J Cardiothorac Surg. 2006;29:790-4
10. Dabir S, Parsa T, Radpay B. et al. Interpleural morphine vs bupivacaine for postthoracotomy pain relief. Asian Cardiovasc Thorac Ann. 2008;16:370-4
11. Allen MS, Halgren L, Nichols FC. et al. A randomized controlled trial of bupivacaine through intracostal catheters for pain management after thoracotomy. Ann Thorac Surg. 2009;88:903-10
12. Tetik O, Islamoglu F, Ayan E. et al. Intermittent infusion of 0.25% bupivacaine through an intrapleural catheter for post-thoracotomy pain relief. Ann Thorac Surg. 2004;77:284-8
13. Yamauchi H, Kobayashi E, Yoshida T. et al. Changes in immune-endocrine response after surgery. Cytokine. 1998;10:549-54
14. Cruickshank AM, Fraser WD, Burns HJ. et al. Response of serum interleukin-6 in patients undergoing elective surgery of varying severity. Clin Sci. 1990;79:161-5
15. Toda H, Murata A, Tanaka N. et al. Changes in serum granulocyte colonystimulating factor (G-CSF) and interleukin 6 (IL-6) after surgical intervention. Res Commun Mol Pathol Pharmacol. 1995;87:275-86
16. Rosalki SB. C-reactive protein. Int J Clin Pract. 2001;55:269-70
17. Bataille R, Klein B. C-reactive protein levels as a direct indicator of interleukin-6 levels in humans in vivo. Arthritis Rheum. 1992;35:982-4
18. Hauser GJ, Ben-Ari J, Colvin MP. et al. Interleukin-6 levels in serum and lung lavage fluid of children undergoing open heart surgery correlate with postoperative morbidity. Intens Care Med. 1998;24:481-6
19. Craig SR, Leaver HA, Yap PL. et al. Acute phase responses following minimal access and conventional thoracic surgery. Eur J Cardiothorac Surg. 2001;20:455-63
20. Yim AP, Wan S, Lee TW. et al. VATS lobectomy reduces cytokine responses compared with conventional surgery. Ann Thorac Surg. 2000;70:243-7
21. Lanser P, Gesell S. Pain management: the fifth vital sign. Healthcare Benchmarks. 2001;8:68-70
22. Colacchio T, Yeager M, Hildebrandt L. Perioperative immunomodulation in cancer surgery. Am J Surg. 1994;167:174-9
23. Torres LM, Collado F, Almarcha JM. et al. Treatment of postoperative pain with intravenous PCA system. Comparison with morphine, metamizole, and buprenorphine. Rev Esp Anestesiol Reanim. 1993;40:181-4
24. Torres LM, Rodríguez MJ, Montero A. et al. Efficacy and safety of dipyrone versus tramadol in the management of pain after hysterectomy: A randomized, double-blind, multicenter study. Reg Anesth Pain Med. 2001;26(2):118-24
25. Sabanathan S, Eng J, Mearns AJ. Alterations in respiratory mechanics following thoracotomy. J R Coll Surg Edinb. 1990;35:144-50
26. Shulman M, Sandler AN, Bradley JW. et al. Postthoracotomy pain and pulmonary function following epidural and systemic morphine. Anesthesiology. 1984;61:569-75
27. Sabanathan S. Has postoperative pain been eradicated? Ann R Coll Surg Engl. 1995;77:202-9
Author contact
![]() Corresponding author: Recep Kesli, MD., Konya Education and Research Hospital, Microbiology Laboratory, Meram Yeni Yol, 42090/ Konya /Turkey. E-mail: recepkeslicom; Phone: +90 332 324 21 60; Fax: +90 332 324 21 60.
Corresponding author: Recep Kesli, MD., Konya Education and Research Hospital, Microbiology Laboratory, Meram Yeni Yol, 42090/ Konya /Turkey. E-mail: recepkeslicom; Phone: +90 332 324 21 60; Fax: +90 332 324 21 60.

 Global reach, higher impact
Global reach, higher impact