3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2025; 22(8):1916-1923. doi:10.7150/ijms.106953 This issue Cite
Research Paper
Predictors of the Fear of COVID-19 in Individuals with Schizophrenia: a Prospective Study
1. Department of Psychiatry, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan.
2. Department of Psychiatry, School of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan.
3. College of Professional Studies, National Pingtung University of Science and Technology, Pingtung, Taiwan.
4. Department of Child and Adolescent Psychiatry, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Kaohsiung, Taiwan.
5. School of Medicine, Chang Gung University, Taoyuan, Taiwan.
6. Department of Psychiatry, Kaohsiung Medical University Gangshan Hospital, Kaohsiung, Taiwan.
7. Department of Psychiatry, Seattle Children's Hospital, Seattle, WA, USA.
8. Department of Psychiatry and Behavioral Sciences, School of Medicine, University of Washington, Seattle, WA, USA.
*These authors contributed equally to this work.
Received 2024-11-14; Accepted 2025-3-13; Published 2025-3-21
Abstract
Purpose: The fear of COVID-19 can result in psychological distress and mental health problems. Individuals with schizophrenia (IWSs) are especially vulnerable to contracting COVID-19. This study with a 1-year follow-up examined whether individual characteristics (sociodemographic characteristics, schizophrenia symptoms, depression, and self-esteem) or factors related to individual-environmental interaction (self-stigma, loneliness, and perceived social support) predicted the level of fear of COVID-19 (FC) among IWSs.
Patients and methods: In total, 257 IWSs (out of an initial pool of 300 IWSs) were enrolled, and their baseline data were collected. FC was assessed using the Fear of COVID-19 Scale at 1 year after the onset of the study. The associations of baseline factors with FC 1 year later were analyzed using bivariable and multiple linear regression analysis.
Results: Bivariable linear regression results demonstrated that being a woman (p < 0.05), being unemployed (p < 0.05), having depression (p < 0.001), having low self-esteem (p < 0.05), experiencing loneliness (p < 0.01), and having feelings of self-stigma (p < 0.001) significantly predicted FC 1 year later. A multiple linear regression model further indicated that having feelings of self-stigma significantly predicted FC 1 year later (p < 0.01).
Conclusion: Clinicians and policymakers should consider the predictors identified in this study when designing interventions to reduce FC among IWSs.
Keywords: COVID-19, schizophrenia, stigma, fear of COVID-19, psychological well-being
Introduction
Fear is the response to the existence of a threat and generally drives actions toward self-protection [1]. Fear can lead individuals to behave in a dysfunctional manner, resulting in the development of general distress and mental health problems [2, 3]. The fear of respiratory infectious diseases (RIDs), including COVID-19 is an unpleasant emotional state that is elicited by the perception of danger and insecurity feelings in the RIDs epidemics or pandemics [4]. People develop the fear of RIDs because of not only the high transmission rate and severe consequences of contraction but also the control measures such as quarantine for prevention of pathogens spreading [5]. A meta-analysis found that fear of COVID-19 (FC) has moderate associations with mental health problems such as anxiety, depression, and sleep problems [2]. FC also makes an individual less able and motivated to adopt preventive behaviors against COVID-19 [6]. Therefore, health-care professionals must not neglect FC when providing medical services in the aftermath of the COVID-19 pandemic.
Individuals with schizophrenia (IWSs) have higher risks of contracting COVID-19 and hospitalization and mortality due to contracting COVID-19 than individuals in the general population [7-11]. Previous studies have found that FC increases anxiety, loneliness, and depression in individuals with schizophrenia [12, 13]. Multiple COVID-19 related factors contribute to the development of FC, such as perceived vulnerability to and harms of contracting COVID-19, pandemic prevention policies (such as quarantine), a lack of pandemic-related information, and contradictions in the public statements of experts and authorities [14]. However, according to ecological system theory [15], FC result from the interactions between individuals and their environment. Several studies have identified individual factors contributing to FC in IWSs, including gender (women reported greater FC than men) [16] and income (higher income was negatively associated with FC) [17]. Additionally, having psychotic symptoms was significantly associated with FC in IWSs [18].
Whether variables related to the interaction of individual and environmental factors (referred to as individual-environmental factors for brevity) such as self-stigma, loneliness, and perceived social support can predict the level of FC in IWSs has not been thoroughly examined. Self-stigma refers to how individuals perceive, accept, and internalize negative stereotypes from others in their attitude toward themselves [19, 20]. Self-stigma can negatively affect the mood of IWSs and increase the severity of their depression, anxiety, and sense of hopelessness; these, in turn, reduce their willingness to follow medical advice [21-23]. The use of self-stigma as a predictive factor in the development of FC among IWSs has not been thoroughly explored. Loneliness refers to the perceived gap between anticipated and actual levels of social connectivity [24]. Previous cross-sectional studies in IWSs have observed that loneliness was positively associated with FC [13], whereas perceived social support was negatively associated with distress during the COVID-19 pandemic [12]. Whether loneliness and perceived social support can predict the degree of the FC in IWSs requires examination in longitudinal studies. Further, low self-esteem is associated with perceived threats and fear arousal in the general population [25]. Self-esteem refers to acceptance and respect for oneself based on the instinctive need to be valued as human being [26]. One study found that self-esteem protected against anxiety symptoms triggered by FC [27]. However, self-esteem has not been extensively explored as a predictor of FC in IWSs.
The present study followed the IWSs participating in a previous study conducted to determine the experiences of stigma and mental health before the severe outbreak of COVID-19 in Taiwan [28-30] and examined the performance of baseline individual characteristics (sociodemographic characteristics, symptoms of schizophrenia, and self-esteem) and individual-environmental factors (self-stigma, loneliness, and perceived social support) as predictors of FC among IWSs one year later. We hypothesized that, among IWSs, FC is (i) associated with a variety of sociodemographic characteristics and schizophrenia symptoms; (ii) positively associated with greater depressive symptoms, self-stigma, and loneliness; and (iii) negatively associated with greater self-esteem and perceived social support.
Material and methods
Study Participants
The present study followed 300 IWSs participating in a study examining the experiences of stigma and mental health [28-31] and examined the predictive effects of baseline individual and individual-environmental factors on FC one year later. The original study initially collected data on 300 IWSs recruited from two community psychiatric rehabilitation institutes and the psychiatric outpatient clinic of a university hospital over the period from February 2022 to May 2022 [28-31]. Taiwan had a relatively mild outbreak of COVID-19 before February 2022; only 0.077% people in Taiwan had been infected with COVID-19 prior this study [32]. Therefore, the baseline data presented the situation of the vast majority of Taiwanese IWSs before the outbreak of COVID-19. The diagnosis of schizophrenia was made according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [33]. One year later, the same 300 individuals were invited to participate in this follow-up study. Trained research assistants explained the purpose and procedure of the follow-up study to the participants. After providing written informed consent, the participants underwent a face-to-face interview in interview rooms for their level of FC to be assessed.
Ethics statement
This study was approved by the institutional review board of Kaohsiung Medical University Hospital (KMUHIRB-SV(I)-20220063). The participants provided their written informed consent to participate in this study. This questionnaire study did not conduct experiments on humans or human tissue samples. This study conformed to the Declaration of Helsinki and the Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals.
Measures
Predictors at baseline
Participants' sociodemographic characteristics, psychiatric diagnosis and symptoms, self-esteem, self-stigma, loneliness, and perceived social support were assessed at baseline.
Sociodemographic characteristics
The participants' gender (female vs. male), age, total years of education completed, total monthly income, marital status (separated or divorced vs. married or cohabiting), and occupational status (unemployed vs. employed) were collected.
Psychiatric symptoms of schizophrenia
Participants' duration of illness (defined as the total years since the initial diagnosis of schizophrenia) was collected. Psychiatrists assessed participants along five domains of psychiatric symptoms, comprising positive symptoms, negative symptoms, disorganization, excitement, and emotional distress, using the Chinese version of the Positive and Negative Syndrome Scale (C-PANSS) [34-36]. The PANSS is the commonly used tool for assessing psychotic symptoms of patients with schizophrenia [35, 36]. Each item on the C-PANSS for the severity of psychiatric symptoms is rated on a 7-point scale from 1 (absent) to 7 (extreme). A higher mean score for each domain indicates more severe psychiatric symptoms. The raters received standardized training for rating the severity of psychiatric symptoms on the C-PANSS prior to the study; the inter-rater reliability (Cohen's kappa coefficient) of the C-PANSS was 0.85. Cronbach's α for the five modules in our study ranged from 0.65 to 0.80. Emotional distress substantially overlapped with depressive symptoms and thus was not used in any linear regression model to reduce the level of collinearity. Participants reported their frequency of depressive symptoms in the preceding month on the Chinese version of the Center for Epidemiologic Studies—Depression Scale (MC-CES-D) [37, 38]. Each item on the MC-CES-D is rated on a 4-point scale from 0 (rarely or none of the time) to 3 (most or all of the time). A higher total MC-CES-D score indicates more severe depressive symptoms. The MC-CES-D has satisfactory internal consistency (Cronbach's α = 0.90), 1-week test-retest reliability (intraclass correlation reliability = 0.93), congruent validity (area under the receiver operative characteristic curves for major depressive disorder = 0.88-0.90), and construct validity [39, 40]. Cronbach's α in our study was 0.91.
Self-esteem
Participants rated their global self-esteem using the Mandarin Chinese version of the Rosenberg Self-Esteem Scale (M-RSES) [41]. The RSES is one of the commonly used instruments for assessing the level of self-esteem. Each item on the M-RSES is rated on a 4-point scale from 1 (strongly disagree) to 4 (strongly agree). A higher M-RSES total score indicates a higher level of global self-esteem. This scale has high reliability and construct validity [41]. Cronbach's alpha in this study was 0.84.
Self-stigma
Participants rated their level of self-stigma from having the diagnosis of schizophrenia on the Taiwanese version of the Self-Stigma Scale-Short (T-SSS-S) [42]. The T-SSS-S is the first instrument for assessing the level of self-stigma in individuals with mental illnesses [50]. Each item on the T-SSS-S is rated on a 4-point scale ranging from 1 (strongly disagree) to 4 (strongly agree). A higher total T-SSS-S score indicates a higher level of self-stigma toward having schizophrenia. The original version and Taiwanese version of the Self-Stigma Scale-Short were found to have acceptable internal consistency (Cronbach's alpha = 0.81-0.84 and 0.87, respectively) and satisfactory construct validity (comparative fit index = 0.97 and 0.99, respectively) in a confirmatory factor analysis model [42, 43]. Cronbach's alpha in this study was 0.88.
Loneliness
Participants rated their degree of loneliness on the Chinese version of the University of California Los Angeles Loneliness Scale—Version 3 (C-UCLA-LS3) [44, 45]. Each item on the C-UCLA-LS3 is rated on a 4-point scale from 1 (never) to 4 (always). A higher total C-UCLA-LS3 score indicates a higher level of loneliness. In previous research, the Chinese versions of the UCLA Loneliness Scale (Version 3) exhibited favorable psychometric properties among individuals with schizophrenia or schizoaffective disorder [44]. Cronbach's α in our study was 0.90.
Perceived social support from families and friends
Participants rated the level of perceived social support from family members and friends on the Chinese version of the Adaptability, Partnership, Growth, Affection, and Resolve (C-APGAR) Index [46, 47]. Each item on the C-APGAR is rated on a 4-point scale from 1 (never) to 4 (always). Higher total scores of the family and friend C-APGAR items indicate higher levels of perceived support from families and friends, respectively. Cronbach's alpha for the family and friend C-APGAR in this study was 0.94 and 0.93, respectively.
Outcome variable: FC
Participants rated their level of FC on the Fear of COVID-19 Scale (FCV-19S) [48]. The FCV-19S is the instrument that have been used to assess FC of people across various countries, genders, age, and backgrounds (e.g., the general population, healthcare worker, and college students) in the COVID-19 pandemic [49]. A review study examining the studies from 21 countries with 16 language versions of FCV-19S confirmed that the FCV-19S is a valid instrument for assessing fear across different languages [50]. Ratings are given on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). An analysis of several studies has independently validated the psychometric properties of FCV-19S obtained in samples of a generally reasonable size in diverse populations [51]. The Taiwanese version of the FCV-19S has a single-factor structure with satisfactory fit indices; the fear of COVID-19 measured by the FCV-19S was significantly associated with psychological distress measured by Depression Anxiety Stress Scale-21 among individuals in Taiwan [6]. Cronbach's alpha coefficient (α) of the FCV-19S in this study was 0.90.
Statistical analysis
We conducted statistical analyses using IBM SPSS Statistics version 24.0 (International Business Machines Corporation, Armonk, NY, USA). Continuous variables are presented in terms of their mean and standard deviation; their distributions were tested for skewness and kurtosis [52]. Categorical variables are presented in terms of their frequency and percentage. The present study used bivariable linear regression to examine the associations of factors at baseline with the reported FC at follow-up. Baseline factors significantly associated with FC at follow-up in bivariable models were utilized in a multivariable regression model. The potential multicollinearity was examined using variance inflation factors (VIF); a VIF value greater than 5 is considered indicative of significant multicollinearity [53]. A p value lower than 0.05 indicated statistical significance.
Results
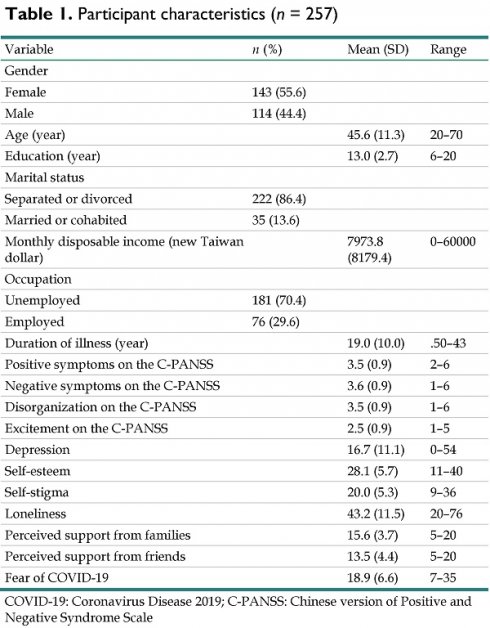
In total, 257 IWSs (85.7% of the initial 300), of whom 55.6% were women, participated in the follow-up study; of the remaining initial IWSs, 13 (4.3%) refused to participate, and 30 (10%) were lost to follow-up. No significant differences in gender (p = 0.093), age (p = 0.389), or years of education (p = 0.459) were observed between those who participated in the follow-up study and those who did not. Table 1 presents the variables at baseline and FC at follow-up for the 257 participants.
Participant characteristics (n = 257)
| Variable | n (%) | Mean (SD) | Range |
|---|---|---|---|
| Gender | |||
| Female | 143 (55.6) | ||
| Male | 114 (44.4) | ||
| Age (year) | 45.6 (11.3) | 20-70 | |
| Education (year) | 13.0 (2.7) | 6-20 | |
| Marital status | |||
| Separated or divorced | 222 (86.4) | ||
| Married or cohabited | 35 (13.6) | ||
| Monthly disposable income (new Taiwan dollar) | 7973.8 (8179.4) | 0-60000 | |
| Occupation | |||
| Unemployed | 181 (70.4) | ||
| Employed | 76 (29.6) | ||
| Duration of illness (year) | 19.0 (10.0) | .50-43 | |
| Positive symptoms on the C-PANSS | 3.5 (0.9) | 2-6 | |
| Negative symptoms on the C-PANSS | 3.6 (0.9) | 1-6 | |
| Disorganization on the C-PANSS | 3.5 (0.9) | 1-6 | |
| Excitement on the C-PANSS | 2.5 (0.9) | 1-5 | |
| Depression | 16.7 (11.1) | 0-54 | |
| Self-esteem | 28.1 (5.7) | 11-40 | |
| Self-stigma | 20.0 (5.3) | 9-36 | |
| Loneliness | 43.2 (11.5) | 20-76 | |
| Perceived support from families | 15.6 (3.7) | 5-20 | |
| Perceived support from friends | 13.5 (4.4) | 5-20 | |
| Fear of COVID-19 | 18.9 (6.6) | 7-35 |
COVID-19: Coronavirus Disease 2019; C-PANSS: Chinese version of Positive and Negative Syndrome Scale
Table 2 presents the results on the associations of factors at baseline with FC 1 year later. The unadjusted regression models demonstrated that female participants had greater FC than male participants (p < 0.05). Additionally, unemployed participants had greater FC than employed participants (p < 0.05). Moreover, higher levels of depression (p < 0.001), self-stigma (p < 0.001), and loneliness (p < 0.01) at baseline were significantly associated with greater FC 1 year later. By contrast, higher self-esteem at baseline was significantly associated with less FC one year later (p < 0.05).
Baseline factors significantly associated with FC were entered into a multivariable linear regression model, which indicated that greater self-stigma (p < 0.01) at baseline was significantly associated with greater FC 1 year later. All VIF values were less than 5, indicating no significant multicollinearity.
Associations of individual, environmental, and individual-environmental interaction factors with the fear of COVID-19 in linear regression analysis
| Unadjusted model | Adjusted model | ||
|---|---|---|---|
| B (se) | B (se) | VIF | |
| Gendera | -1.740 (0.824)* | -1.554 (0.808) | 1.030 |
| Age | 0.034 (0.036) | - | |
| Education | -0.193 (0.156) | - | |
| Monthly disposable incomeb | -0.028 (0.051) | - | |
| Marital statusc | 0.876 (1.203) | - | |
| Occupationd | -1.817 (0.898)* | -1.105 (0.887) | 1.047 |
| Duration of illness | 0.028 (0.041) | - | |
| Positive symptoms on the C-PANSS | 0.028 (0.463) | - | |
| Negative symptoms on the C-PANSS | 0.575 (0.437) | - | |
| Disorganization on the C-PANSS | 0.419 (0.474) | - | |
| Excitement on the C-PANSS | -0.001 (0.055) | - | |
| Depression | 0.137 (0.036)*** | 0.079 (0.060) | 2.829 |
| Self-esteem | -0.165 (0.071)* | 0.152 (0.106) | 2.349 |
| Self-stigma | 0.331 (0.075)*** | 0.272 (0.104)** | 1.947 |
| Loneliness | 0.093 (0.035)** | 0.021 (0.050) | 2.154 |
| Perceived support from families | 0.018 (0.113) | - | |
| Perceived support from friends | -0.138 (0.093) | - | |
Reference criteria: a female, b 1000 new Taiwan dollars per unit, c separated or divorced, d unemployed.
*p < .05; **p < .01; ***p < .001.
COVID-19: Coronavirus Disease 2019; C-PANSS: Chinese version of Positive and Negative Syndrome Scale; VIF: Variance Inflation Factor
Discussion
The adjusted regression model revealed that greater self-stigma at baseline was positively associated with FC in IWSs at follow-up 1 year later. The unadjusted regression models in this study also indicated that being female, being unemployed, having higher levels of depression, self-stigma, and loneliness, and having lower self-esteem at baseline were significantly associated with greater FC; however, the associations of these baseline variables with FC at follow-up became non-significant, indicating that there might be confounding effects among these variables.
The effect of self-stigma on FC in IWSs may stem from several mechanisms. First, self-stigma has substantial negative effects on the mental health of IWSs and increases the risks of depression, anxiety, hopelessness, and suicidality [21-23, 29]. Mental health problems contribute to these individuals' automatic thoughts [54] and catastrophic beliefs [55], which are detrimental to rational appraisals of risk and timely responses to the urgent threat of COVID-19, potentially increasing FC in these individuals. Second, self-stigma and related mental health problems may compromise the self-efficacy of IWSs [56]; this weakened self-efficacy may have increased the difficulty they experienced in confidently dealing with the problems encountered during the COVID-19 pandemic, exacerbating their FC. Third, self-stigma can worsen individuals' social functioning [57]. A lack of connection with others may have limited information and psychological and material support available to IWSs during the COVID-19 pandemic, further exacerbating their FC. Fourth, self-stigma may decrease individuals' willingness to seek medical assistance from health-care professionals [57]. Consequently, many IWSs experienced great FC during the pandemic due to a lack of reliable information and resources from medical professionals. The results of this study indicate that intervention programs for reducing self-stigma in IWSs are beneficial to the health of IWSs during normal times and can reduce fear during an outbreak of infectious diseases.
The unadjusted regression models in the present study demonstrated that loneliness but not perceived social support at baseline were positively associated with FC 1 year later in IWSs. Humans are innately social beings and have a neurobiological need to “belong to a certain group” [58, 59]. Loneliness is the negative subjective feeling that arises when individuals are isolated, misunderstood, or rejected or when individuals are not satisfied with their social relationships [60]. Loneliness is also an emotional consequence of the cognitive evaluation of social interactions. When expectations of the quality and quantity of social interactions and networks are unmet, individuals experience negative emotional reactions [61]. According to social information processing models [62, 63], individuals with prominent loneliness are hypervigilant to socially threatening stimuli, expect to experience negative social interactions, reflexively make negative appraisals of self and others, remember more past negative messages than positive ones, and have future goals focused on preventing painful feelings rather than creating positive experiences [62-64]. Therefore, during the pandemic, individuals who experienced considerable loneliness may have experienced great FC when faced with drastic changes to their routines and social interactions. Further, studies have found a positive association between loneliness and stigmatizing experiences in IWSs [65, 66]. The association of loneliness and FC might be confounded by self-stigma in this study. Based on the results of this study, it is necessary to enhance social support for IWSs and help them adjust the perception of interpersonal interactions to reduce perceived loneliness.
The unadjusted regression models of the present study found that being a woman, being unemployed, feeling depressed, and having low self-esteem at baseline predicted FC 1 year later. Biological variables (e.g., hormones) and social factors (e.g., social expectations of gender roles) may account for the observed difference along gender lines in FC in IWSs [16]. Employment provides a regular income, which reduced the negative influences of the COVID-19 pandemic on daily life and thus may have mitigated FC in employed IWSs [17]. Depression can compromise cognitive function and skills that are essential to the adoption of protective behaviors against COVID-19, and may thus have increased FC in IWSs with depression. By contrast, IWSs with high self-esteem were likely to be more confident that they could manage the difficulties of COVID-19 and thus felt less threatened by the pandemic. Further, studies have found that both depressive symptoms and low self-esteem were associated with higher self-stigma in individuals with severe mental illnesses [23]. Therefore, the associations of depressive symptoms and self-esteem with FC in IWSs might be confounded by self-stigma.
The present study demonstrated that self-stigma can predict FC among IWSs. Eliminating public stigma toward schizophrenia is essential to preventing the development of self-stigma. Therefore, government authorities and health-care professionals must educate the public on the etiology of schizophrenia and mitigate overt and subtle discrimination toward IWSs. For IWSs, psychoeducation and cognitive behavioral therapy effectively reduce self-stigma [67, 68]. These intervention programs integrate elements of education about schizophrenia, cognitive techniques for dealing with public attitudes toward and beliefs in schizophrenia, and psychodynamic approach for dealing with emotional reactions associated with schizophrenia and stigma [67, 68]. Several online intervention programs have been developed to improve the stigma in IWSs and should be feasible during a pandemic [69, 70]. Community-based stigma reduction strategies, such as contact interventions, educational interventions, and family psychoeducation programs should be also established to reduce public stigma toward schizophrenia [71]. Furthermore, although the predictive effects of individual factors (gender, employment status, depression, loneliness, and self-esteem) for FC did not reach significance in this study's multivariable regression model, health-care professionals must consider these variables when developing intervention programs to help IWSs cope with the changes caused by the COVID-19 pandemic.
This study has several limitations. First, the study collected self-reported data from IWSs and may be affected by informant bias. Second, the participants were invited from community psychiatric rehabilitation institutes and psychiatric outpatient clinics and were invested in participating in this follow-up assessment. Thus, the study may be affected by sampling bias. Third, this study did not examine the predictive effect of baseline physical health status and COVID-19-related variables such as participants' and family members' history of contracting COVID-19 and related hospitalization, receipt of COVID vaccination, COVID-related burden, and fear of COVID-19; these may be confounders affecting the study's results.
Conclusion
Self-stigma significantly predicted the severity of FC 1 year later among IWSs. Gender, employment status, depression, loneliness, and self-esteem also had predictive effects on FC in bivariable linear regression models. The identified predictors should be considered in the design of interventions against FC among IWSs.
Abbreviations
IWSs: Individuals with schizophrenia; COVID-19: Coronavirus Disease 2019; FC: fear of COVID-19; C-PANSS: Chinese version of the Positive and Negative Syndrome Scale; MC-CES-D: Chinese version of the Center for Epidemiologic Studies—Depression Scale; M-RSES: Mandarin Chinese version of the Rosenberg Self-Esteem Scale; T-SSS-S: Taiwanese version of the Self-Stigma Scale-Short; C-UCLA-LS3: Chinese version of the University of California Los Angeles Loneliness Scale—Version 3; C-APGAR: Chinese version of the Adaptability, Partnership, Growth, Affection, and Resolve Index; FCV-19S: Fear of COVID-19 Scale.
Acknowledgements
Funding
This study was supported by research grants from Kaohsiung Medical University Hospital (grant KMUH111-1M52) and the National Science and Technology Council of Taiwan (grant 112-2314-B-037-041). The funding agency did not have a role in this study.
Availability of data and materials
The data will be available upon reasonable request to the corresponding authors
Competing Interests
The author(s) report no conflicts of interest in this work.
References
1. Hooley JM, Butcher JN, Nock M, Mineka S. Abnormal Psychology. 17 edition. Boston: Pearson. 2017
2. Alimoradi Z, Ohayon MM, Griffiths MD, Lin CY, Pakpour AH. Fear of COVID-19 and its association with mental health-related factors: systematic review and meta-analysis. BJPsych Open. 2022;8:e73
3. Cikrikci O, Cikrikci N, Griffiths M. Fear of COVID-19, stress and depression: A meta-analytic test of the mediating role of anxiety. Psychol Psychother. 2022;95:853-74
4. Pakpour AH, Griffiths MD, Lin CY. Assessing psychological response to the COVID-19: The Fear of COVID-19 Scale and the COVID Stress Scales. Int J Ment Health Addict. 2021;19:2407-10
5. Masuyama A, Shinkawa H, Kubo T. Validation and psychometric properties of the Japanese Version of the Fear of COVID-19 Scale among adolescents. Int J Ment Health Addict. 2022;20:387-97
6. Chang KC, Hou WL, Pakpour AH, Lin CY, Griffiths MD. Psychometric testing of three COVID-19-related scales among people with mental illness. Int J Ment Health Addict. 2022;20:324-36
7. Wang Q, Xu R, Volkow ND. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20:124-30
8. Nemani K, Li C, Olfson M, Blessing EM, Razavian N, Chen J. et al. Association of psychiatric disorders With mortality among patients with COVID-19. JAMA Psychiatry. 2021;78:380-6
9. Toubasi AA, AbuAnzeh RB, Tawileh HBA, Aldebei RH, Alryalat SAS. A meta-analysis: The mortality and severity of COVID-19 among patients with mental disorders. Psychiatry Res. 2021;299:113856
10. Tzur Bitan D, Kridin K, Cohen AD, Weinstein O. COVID-19 hospitalisation, mortality, vaccination, and postvaccination trends among people with schizophrenia in Israel: a longitudinal cohort study. Lancet Psychiatry. 2021;8:901-8
11. Vai B, Mazza MG, Delli Colli C, Foiselle M, Allen B, Benedetti F. et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry. 2021;8:797-812
12. Brosch K, Meller T, Pfarr JK, Stein F, Schmitt S, Ringwald KG. et al. Which traits predict elevated distress during the Covid-19 pandemic? Results from a large, longitudinal cohort study with psychiatric patients and healthy controls. J Affect Disord. 2022;297:18-25
13. Lee YR, Chung YC, Kim JJ, Kang SH, Lee BJ, Lee SH. et al. Effects of COVID-19-related stress and fear on depression in schizophrenia patients and the general population. Schizophrenia (Heidelb). 2022;8:15
14. Heiat M, Heiat F, Halaji M, Ranjbar R, Tavangar Marvasti Z, Yaali-Jahromi E. et al. Phobia and fear of COVID-19: origins, complications and management, a narrative review. Ann Ig. 2021;33:360-70
15. Bronfenbrenner U. The Ecology of Human Development Experiments by Nature and Design. Harvard University Press. 1979
16. Metin A, Erbiçer ES, Şen S, Çetinkaya A. Gender and COVID-19 related fear and anxiety: A meta-analysis. J Affect Disord. 2022;310:384-95
17. Morgado-Toscano C, Gómez-Salgado J, Fagundo-Rivera J, Navarro-Abal Y, Rodríguez-Jiménez L, Climent-Rodríguez JA. et al. Anxiety and fear of COVID-19 in the UK general population: A cross-sectional study. Medicine (Baltimore). 2023;102:e33045
18. Bitar Z, Haddad C, Obeid S, Hallit S. The association between fear of COVID-19 and depression, anxiety, and psychosis among Lebanese chronic patients with schizophrenia: any moderating effect of spirituality? Croat Med J. 2022;63:412-22
19. Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: Implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25:875-84
20. Watson AC, Corrigan P, Larson JE, Sells M. Self-stigma in people with mental illness. Schizophr Bull. 2007;33:1312-8
21. Rüsch N, Zlati A, Black G, Thornicroft G. Does the stigma of mental illness contribute to suicidality? Br J Psychiatry. 2014;205:257-9
22. Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71:2150-61
23. Dubreucq J, Plasse J, Franck N. Self-stigma in serious Mental Illness: A Systematic Review of Frequency, Correlates, and Consequences. Schizophr Bull. 2021;47:1261-87
24. de Jong Gierveld J, van Tilburg T, Dykstra PA. Loneliness and social isolation. In: Vangelisti AL, Perlman D, editors. The Cambridge Handbook of Personal Relationships. Cambridge: Cambridge University Press. 2006 p. 485-500
25. Lin HC, Chen CC. Disease prevention behavior during the COVID-19 pandemic and the role of self-esteem: An extended parallel process model. Psychol Res Behav Manag. 2021;14:123-35
26. Gullotta T, Adams GR, Ramos JM. Handbook of Adolescent Behavioral Problems: Evidence-based Approaches to Prevention and Treatment. New York, NY: Springer. 2005
27. Rossi A, Panzeri A, Pietrabissa G, Manzoni GM, Castelnuovo G, Mannarini S. The anxiety-buffer hypothesis in the time of COVID-19: When self-esteem protects from the impact of loneliness and fear on anxiety and depression. Front Psychol. 2020;11:2177
28. Chen YL, Jian CR, Chang YP, Chao SR, Yen CF. Association of loneliness with suicide risk and depression in individuals with schizophrenia: moderating effects of self-esteem and perceived support from families and friends. Schizophrenia (Heidelb). 2023;9:41
29. Jian CR, Wang PW, Lin HC, Huang MF, Yeh YC, Liu TL. et al. Association between self-stigma and suicide risk in individuals with schizophrenia: Moderating effects of self-esteem and perceived support from friends. Int J Environ Res Public Health. 2022;19:15071
30. Jian C-R, Chang Y-P, Lin C-Y. Assessing perceived emotional social support in individuals with schizophrenia or schizoaffective disorder: The multisource emotional support inventory. Taiwanese Journal of Psychiatry. 2023;37:127
31. Lin CW, Chang YP, Yen CF. Predictors of motivation to receive a COVID-19 vaccination and the number of COVID-19 vaccine doses received in patients with schizophrenia. Vaccines (Basel). 2023;11:1781
32. National Center for High-performance Computering. Taiwan county and city area daily new confirmed diagnosis chart. Available from:https://covid-19.nchc.org.tw/2023_city_confirmed.php; 4 March. 2024
33. American Psychiatric aAssociation. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, US: American Psychiatric Publishing, Inc. 2013
34. Cheng JJ. Positive and Negative Syndrome Scale (PANSS): establishment and reliability study of a Mandarin Chinese language version. Chin Psychiatry. 1996;10:251-8
35. Kay SR. Positive and Negative Syndromes in Schizophrenia: Assessment and Research. Psychology Press. 1991
36. van der Gaag M, Hoffman T, Remijsen M, Hijman R, de Haan L, van Meijel B. et al. The five-factor model of the Positive and Negative Syndrome Scale II: a ten-fold cross-validation of a revised model. Schizophr Res. 2006;85:280-7
37. Chien CP, Cheng TA. Depression in Taiwan: Epidemiological survey utilizing CES-D. Seishin Shinkeigaku Zasshi. 1985;87:335-8
38. Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385-401
39. Yang HJ, Soong WT, Kuo PH, Chang HL, Chen WJ. Using the CES-D in a two-phase survey for depressive disorders among nonreferred adolescents in Taipei: a stratum-specific likelihood ratio analysis. J Affect Disord. 2004;82:419-30
40. Cheng CP, Yen CF, Ko CH, Yen JY. Factor structure of the Center for Epidemiologic Studies Depression Scale in Taiwanese adolescents. Compr Psychiatry. 2012;53:299-307
41. Rosenberg M. The Measurement of Self-esteem, Society and the Adolescent Self-image. Princeton: Princeton University Press. 1965
42. Mak WW, Cheung RY. Self-stigma among concealable minorities in Hong Kong: conceptualization and unified measurement. Am J Orthopsychiatry. 2010;80:267-81
43. Wu TH, Chang CC, Chen CY, Wang JD, Lin CY. Further psychometric evaluation of the self-stigma scale-short: measurement invariance across mental illness and gender. PLoS One. 2015;10:e0117592
44. Lin CY, Tsai CS, Jian CR, Chao SR, Wang PW, Lin HC. et al. Comparing the psychometric properties among three versions of the UCLA Loneliness Scale in individuals with schizophrenia or schizoaffective disorder. Int J Environ Res Public Health. 2022;19:8443
45. Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20-40
46. Chen. Y-C, HSU. C-C, Hsu. S-H, Lin. C-C. A preliminary study of family APGAR index. Acta Paediatrica Sinica. 1980;21:210-7
47. Smilkstein G. The Family APGAR: A proposal for family function test and its use by physicians. J Fam Pract. 1978;6:1231-9
48. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and initial validation. Int J Ment Health Addict. 2022;20:1537-45
49. Luo F, Ghanei Gheshlagh R, Dalvand S, Saedmoucheshi S, Li Q. Systematic review and meta-analysis of fear of COVID-19. Front Psychol. 2021;12:661078
50. Alimoradi Z, Lin CY, Ullah I, Griffiths MD, Pakpour AH. Item response theory analysis of the Fear of COVID-19 Scale (FCV-19S): A systematic eeview. Psychol Res Behav Manag. 2022;15:581-96
51. Blázquez-Rincón D, Aguayo-Estremera R, Alimoradi Z, Jafari E, Pakpour AH. The Fear of COVID-19 Scale: A meta-analytic structural equation modeling approach. Psychol Assess. 2023;35:1030-40
52. Lin CY, Luh WM, Cheng CP, Yang AL, Su CT, Ma HI. Measurement equivalence across child self-reports and parent-proxy reports in the Chinese version of the pediatric quality of life inventory version 4.0. Child Psychiatry Hum Dev. 2013;44:583-90
53. O'brien RM. A caution regarding rules of thumb for variance inflation factors. Qual Quant. 2007;41:673-90
54. Hiçdurmaz D, İnci F, Karahan S. Predictors of mental health symptoms, automatic thoughts, and self-esteem among university students. Psychol Rep. 2017;120:650-69
55. Gellatly R, Beck AT. Catastrophic thinking: A transdiagnostic process across psychiatric disorders. Cognit Ther Res. 2016;40:441-52
56. Drapalski AL, Lucksted A, Brown CH, Fang LJ. Outcomes of ending self-stigma, a group intervention to reduce internalized stigma, among individuals with serious mental illness. Psychiatr Serv. 2021;72:136-42
57. Ociskova M, Prasko J, Holubova M, Latalova K, Sollar T, Zatkova M. et al. Self-stigma in patients with schizophrenia: Impact and management. Neuro Endocrinol Lett. 2023;44:368-83
58. Baumeister RF, Leary MR. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117:497-529
59. Insel TR, Young LJ. The neurobiology of attachment. Nat Rev Neurosci. 2001;2:129-36
60. Andersson L. Loneliness research and interventions: A review of the literature. Aging Ment Health. 1998;2:264-74
61. Peplau LA, Perlman D. Loneliness: A Sourcebook of Current Theory, Research, and Therapy. New York: Wiley. 1982
62. Spithoven AWM, Bijttebier P, Goossens L. It is all in their mind: A review on information processing bias in lonely individuals. Clin Psychol Rev. 2017;58:97-114
63. Eglit GML, Palmer BW, Martin AS, Tu X, Jeste DV. Loneliness in schizophrenia: Construct clarification, measurement, and clinical relevance. PLoS One. 2018;13:e0194021
64. Liao H-Y, Lee Y, Hsu S-T, Yen C-F. Loneliness in patients with schizophrenia. Taiwanese Journal of Psychiatry. 2021;35:59-63
65. Suman A, Nehra R, Sahoo S, Grover S. Prevalence of loneliness and its correlates among patients with schizophrenia. Int J Soc Psychiatry. 2023;69:906-15
66. Yildirim T, Kavak Budak F. The relationship between internalized stigma and loneliness in patients with schizophrenia. Perspect Psychiatr Care. 2020;56:168-74
67. Ivezić S, Sesar MA, Mužinić L. Effects of a group psychoeducation program on self-stigma, empowerment and perceived discrimination of persons with Sschizophrenia. Psychiatr Danub. 2017;29:66-73
68. Shih CA, Huang JH, Yang MH. Anti-stigma psychosocial intervention effects on reducing mental illness self-stigma and increasing self-esteem among patients with schizophrenia in Taiwan: A quasi-experiment. Asian J Psychiatr. 2022;73:103171
69. Randhawa A, Kühn S, Schöttle D, Moritz S, Gallinat J, Ascone L. The effects of assessing character strengths vs. psychopathology on mood, hope, perceived stigma and cognitive performance in individuals with psychosis. PLoS One. 2023;18:e0289872
70. Fernandez DK, Deane FP, Vella SA. Effects of online continuum and categorical belief manipulations on schizophrenia stigma, help-seeking, and help-provision. Psychiatry Res. 2022;307:114293
71. Morgan AJ, Reavley NJ, Ross A, Too LS, Jorm AF. Interventions to reduce stigma towards people with severe mental illness: Systematic review and meta-analysis. J Psychiatr Res. 2018;103:120-33
Author contact
![]() Corresponding author: Peng-Wei Wang, Department of Psychiatry, Kaohsiung Medical University Hospital, 100 Tzyou 1st Road, Kaohsiung 80703, Taiwan. Tel. (optional): 886-7-3124941; Fax (optional); 886-7-3134761; Email: wistar.huangcom.
Corresponding author: Peng-Wei Wang, Department of Psychiatry, Kaohsiung Medical University Hospital, 100 Tzyou 1st Road, Kaohsiung 80703, Taiwan. Tel. (optional): 886-7-3124941; Fax (optional); 886-7-3134761; Email: wistar.huangcom.

 Global reach, higher impact
Global reach, higher impact