3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2021; 18(7):1711-1720. doi:10.7150/ijms.53602 This issue Cite
Research Paper
Development and validation of a comprehensive radiomics nomogram for prognostic prediction of primary hepatic sarcomatoid carcinoma after surgical resection
1. Department of Liver Surgery, Liver Transplantation Center, West China Hospital of Sichuan University, No. 37 GuoXue Alley, Chengdu 610041, China.
2. West China School of Medicine, West China Hospital, Sichuan University, No. 37 GuoXue Alley, Chengdu 610041, China.
3. Department of Biotherapy, West China Hospital and State Key Laboratory of Biotherapy, Sichuan University, No. 37 GuoXue Alley, Chengdu 610041, China.
*These authors contribute equally to this work.
Abstract
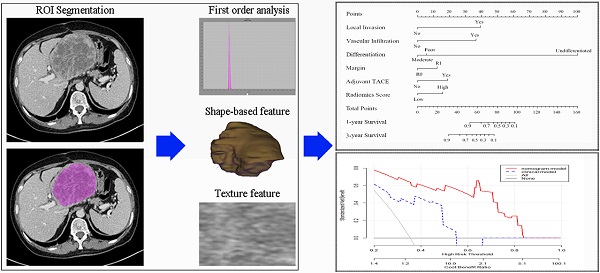
Objective: This study aimed to establish and validate a radiomics nomogram comprised of clinical factors and radiomics signatures to predict prognosis of primary hepatic sarcomatoid carcinoma (PHSC) patients after surgical resection.
Methods: In this retrospective study, 79 patients with pathological confirmation of PHSC and underwent surgical resection were recruited. A radiomics nomogram was developed by radiomics signatures and independent clinical risk factors selecting from multivariate Cox regression. All patients were stratified as high risk and low risk by nomogram. Model performance and clinical usefulness were assessed by C-index, calibration curve, decision curve analysis (DCA) and survival curve.
Results: A total of 79 PHSC were included with 1-year and 3-year overall survival rates of 63.3% and 35.4%, respectively. The least absolute shrinkage and selection operator (LASSO) method selected 3 features. Multivariate Cox analysis found six independent prognostic factors. The radiomics nomogram showed a significant prediction value with overall survival (HR: 7.111, 95%CI: 3.933-12.858, P<0.001). C-index of nomogram was 0.855 and 0.829 in training and validation set, respectively. Decision curve analysis validated the clinical utility of this nomogram. There was a significant difference in the 1-year and 3-year survival rates of stratified high-risk and low-risk patients in the whole cohort (30.6% vs. 90.1% and 5.6% vs. 62.4%, respectively, P < 0.001).
Conclusion: This radiomics nomogram serve as a potential tool for predicting prognosis of PHSC after surgical resection, and help to identify high risk patients who may obtain feeble survival benefit from surgical resection.
Keywords: primary hepatic sarcomatoid carcinoma, prognosis, nomogram, radiomics, clinical decision-making

 Global reach, higher impact
Global reach, higher impact