3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2012; 9(8):725-729. doi:10.7150/ijms.4726 This issue Cite
Research Paper
Clinical Effect of Acute Complete Acromioclavicular Joint Dislocation Treated with Micro-Movable and Anatomical Acromioclavicular Plate
Department of Orthopaedic Surgery, the Affiliated Southeast Hospital of Xiamen University, Orthopaedic Trauma Center of PLA, Zhangzhou, 363000, PR China.
Received 2012-6-11; Accepted 2012-9-17; Published 2012-10-14
Abstract
Objectives: We evaluated the long-term clinical results of acute complete acromioclavicular dislocations treated with micro-movable and anatomical acromioclavicular plate.
Methods: Open reduction and internal fixation was performed using the MAAP in 16 patients (10 males, 6 females; mean age 36 years; range16 to 63 years) with acute complete acromioclavicular joint dislocation. Radiographic evaluations were routinely conducted every 3 weeks until 3 months postoperatively. The MAAP were removed under local anesthesia after 3 months postoperatively. We evaluated the functional results by using the constant scoring system and radiological results in the last follow-up time. The mean follow up was 26 months (range 16 to 38 months).
Results: The mean Constant score was 94 (range, 78 to 100). The results were excellent in 12 patients (75.0%), good in 3 patients (18.8%) and satisfactory in 1patient (6.2%). Three patients with scores of 80 to 90 had mild pain during activity, but have not affected the shoulder range of motion. One patient has both some pain and limited range of motion of shoulder joint. All patients but one have returned to their preoperative work without any limitations. Compared to the contralateral side, radiography showed anatomical reposition in the vertical plane in 14 cases, slight loss of reduction in 2 older patients.
Conclusion: We recommend the MAAP fixation for surgical treatment of acute complete acromioclavicular joint dislocation as it could provide satisfactory shoulder functions and clinical results, with lower complication rate. However, it is necessary to continue to observe the clinical effects of this fixation technique.
Keywords: Acromioclavicular joint, Dislocation, Micro-movable fixation
INTRODUCTION
Acromioclavicular joint dislocation is prone to occur through a direct or an indirect injury mechanism, which has been divided into three grades by Tossy in the 1960s according to the extent of displacement of the clavicle end in relation to the acromion[1]. Radiographs of Tossy grade III show the acromioclavicular joint is displaced greater than one half its normal depth,which indicates that acromioclavicular and coracoclavicular ligaments have been completely torn.
A number of different procedures, including nonoperative and operative, have been described for acute complete acromioclavicular joint dislocation, but there is no consensus over the most appropriate treatment method so far. The purpose of this study is to discuss our treatment of 16 patients with acute complete acromioclavicular joint dislocation using micro-movable and anatomical acromioclavicular plate (MAAP) fixation and to evaluate the long-term clinical results.
MATERIALS AND METHODS
In collaboration with Xiamen Double Engine Medical Material Co Ltd, we have designed a MAAP, for which we have obtained the national invention patent (patent number: 200620009587.3). This plate is made of titanium alloy and was designed in accordance with the surface anatomy of the clavicle and acromion, which is composed by three parts, such as clavicle lateral anatomical plate, acromion medial anatomical plate and micro-movable connecting rods. The plate has 4 screw holes on the acromion side, and clavicle side of 5,7,or 9 screw holes can be used (Fig. 1).
From February 2007 to August 2009, 16 patients (10 males, 6 females; mean age 36 years; range 16 to 63 years) seen at the 175th Hospital of People 's Liberation Army, for acute complete acromioclavicular joint dislocation were included in this study. According to the typical history of shoulder injuries, stress radiographs examination results and Tossy classification[1], all of the patients can be confirmed this clinical diagnosis which belongs to Tossy grade III. Table 1 shows demographics, follow-up time and mechanism of injury of each patient.
Surgical methods
A length of 5-6 cm longitudinal skin incision was made centred on the acromioclavicular joint. Soft tissue and muscle were separated to expose the superior surface of dislocated acromioclavicular joint and the lateral end of the clavicle. The intra-articular meniscus was removed, if damaged. MAAP was then applied onto the acromion medial side and fracture ends. A four-hole acromion medial plate was used and fixed with cancellous screw to increase the plate holding force and clavicle lateral anatomical plate was fixed with cortical screws or cancellous screw according to the bone condition. The acromioclavicular ligament and capsule were neither dissected nor repaired. The anterior portion of the deltoid was finally repaired back to its origin using absorbable suture.
Postoperative treatment
Postoperatively, all patients wear a sling immobilization for 4 weeks, with active and passive activities allowed in the neighboring joints such as the elbow and the wrist. After this period, we encourage patients to strengthen the shoulder joint functional exercises, including passive pendulum exercises and active “crawling up the wall” exercises, to avoid joint stiffness and heterotopic ossification. The MAAP removal was performed after about 3 months in the hospital under local anesthesia.
Follow-up
All patients received clinical follow-up, which were assessed by clinical results and radiographic follow-ups. Functional results were evaluated in the last follow-up time by using the constant scoring system[2]. Constant score combines patient's subjective symptom scores (35%) which assess pain and vocational activities and objective scores (65%) which measures shoulder range of motion and shoulder strength[2]. Score range from 0 to 100, with higher scores indicating better shoulder function.
Radiographic evaluations were routinely conducted every 3 weeks until 3 months postoperatively. We use the method which has been described by Pavlik by evaluating the vertical distance between the inferior border of the acromion and the clavicle in comparison with the contralateral side and measured the differences in millimeters (less than 2 mm, anatomical reposition; 2-4 mm, slight loss of reduction; 4-8 mm, partial loss of reduction; greater than 8 mm, total loss of reduction)[3]. Degenerative changes of the acromioclavicular joint was also reviewed and recorded.
The appearance of micro-movable and anatomical acromioclavicular plate (MAAP).

RESULTS
The patients were followed up for a mean time of 26 months (range, 16 to 38 months). In the final stages of follow-up, the average Constant score was 94 (range, 78 to 100). In these patients, twelve scored above 90, three scored between 80 and 90,only one patient scored 78 (Table 1). Mild pain during activity was the main confusion in these three patients with scores of 80 to 90 which started after operation without any other trauma and can change with the weather changes, but have not affected the shoulder range of motion (cases 7, 8, and 10; Constant scores,83, 87,86, respectively). In one patient with the score 78 who has both some pain and limited range of motion of shoulder joint (case 12). It can be obtained satisfactory results by Intra-articular steroid injection therapy to relieve pain of shoulder. No patients showed decreasing of muscle strength.
Postoperative radiograph follow-ups showed two older patients had screw loosening with degenerative changes and slight loss of reduction of the acromioclavicular joint (cases 7 and 10). No patient had a MAAP broken and complete dislocation of the acromioclavicular joint during follow-up (Fig. 2). There were no signs of redislocation of joint. Apart from a few patients ' pain symptoms, no other complications were observed. In addition to a patient because of frequent shoulder pain and limited range of motion of shoulder joint, all patients have returned to their preoperative work without any limitations.
Detailed data of 16 patients treated with the (MAAP)
| Case | Age (years) | Mechanism of injury | Time to Removal (weeks) | Duration of follow-up (months) | Complication | Constant score | Functional results | Radiological results |
|---|---|---|---|---|---|---|---|---|
| 1 | 16 | Fall in playing football | 10 | 16 | None | 100 | Excellent | Normal |
| 2 | 23 | Fall in playing basketball | 10 | 24 | None | 94 | Excellent | Normal |
| 3 | 32 | Traffic accident | 11 | 19 | None | 96 | Excellent | Normal |
| 4 | 19 | Fall in playing football | 10 | 24 | None | 100 | Excellent | Normal |
| 5 | 43 | Fall from motorcycle | 11 | 18 | None | 96 | Excellent | Normal |
| 6 | 43 | Traffic accident | 12 | 21 | None | 100 | Excellent | Normal |
| 7 | 63 | Fall from bike | 12 | 21 | Acromioclavicular arthritis | 83 | Good | Screw loosing, slight loss of reduction |
| 8 | 36 | Fall down the stairs | 12 | 38 | Acromioclavicular arthritis | 87 | Good | Normal |
| 9 | 48 | Traffic accident | 12 | 28 | None | 94 | Excellent | Normal |
| 10 | 62 | Fall from bike | 12 | 30 | Acromioclavicular arthritis | 86 | Good | Screw loosing, slight loss of reduction |
| 11 | 23 | Traffic accident | 12 | 32 | None | 100 | Excellent | Normal |
| 12 | 28 | Traffic accident | 12 | 28 | Limited range of motion, acromioclavicular arthritis | 78 | Satisfactory | Normal |
| 13 | 34 | Fall down the stairs | 12 | 36 | None | 100 | Excellent | Normal |
| 14 | 40 | Fall from motorcycle | 12 | 27 | None | 92 | Excellent | Normal |
| 15 | 34 | Traffic accident | 12 | 30 | None | 98 | Excellent | Normal |
| 16 | 32 | Fall from motorcycle | 12 | 24 | None | 100 | Excellent | Normal |
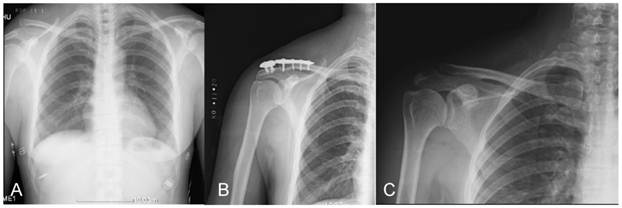
A 43-year-old man fell from motorcycle. (A) A preoperative radiograph of his chest showed acute complete acromioclavicular joint dislocation. (B) A postoperative radiograph of the same patient showed the ideal reduction of acromioclavicular joint and correct position of the MAAP. (C) Three months after open reduction and internal fixation. The MAAP was removed without any complication.
DISCUSSION
The purpose of this study is to demonstrate that acute complete acromioclavicular joint dislocation can be treated by means of a MAAP and evaluate the results of this surgical fixation methods through clinical follow-ups.
Patients with complete acromioclavicular joint dislocation are often associated with complete tear of the conoid and the trapezoid ligaments, which are usually recommended surgical treatment to stabilize the acromioclavicular joint and promote the restoration of ligaments[1]. Surgical techniques mainly include directly through the metal fixation of acromioclavicular joint and indirect suture ligament to stabilize the acromioclavicular joint. There are many metallic implants available to treat these cases. One of the popular methods is pin fixation using either smooth or threaded Kirschner wires after a closed or open reduction. However, given that Sethi[4] and Norrell et al.[5] reported the rare but catastrophic complications due to migration of the pins, this surgical method has been abandoned. The clavicle hook plate is a convenient device which was commonly used in Europe. Although it has been successful in treating acromioclavicular joint dislocations and distal clavicle fractures with good clinical results, there are still several complications such as infection, clavicular stress fracture, acromion fracture, and hook or screw cutout[6-8]. Screws and in combination with ligament reconstruction were recommended in treatment of acute complete acromioclavicular joint dislocation, and potential complications of this technique include suture cutout[9-11]. Other surgical techniques to stabilize the lateral clavicle and acromioclavicular joint include reconstruction of the coracoclavicular ligament by using a variety of suture materials or using autograft or allograft tissues[12]. The use of native coracoacromial ligament to reestablish acromioclavicular joint stability was first described in 1972 by Weaver[13]. Then, Morrison et al.[14] passed through drill holes in the base of the coracoid and the lateral clavicle using synthetic loop augmentation to stabilize acromioclavicular joint and obtained good and excellent results. Baumgarten et al.[15] used an arthroscopcally assisted technique with a semitendinosus allograft to reconstruct the acromioclavicular joint, which required only 3-cm incision over the distal clavicle. However, these surgical techniques restricted rotational movement between the clavicle and the scapula during motion of the humerus, especially abduction and forward flexion of the shoulder, because it connects the clavicle and acromion so firmly[16].
The range of movement at the acromioclavicular joint has been investigated for many years. In the early cadaveric study, Moseley et al[17] reported that the acromioclavicular joint had a certain degree of rotation. Recently, three-dimensional studies of the acromioclavicular joint using open MR imaging showed that the acromioclavicular joint has approximately 15-20°of rotation, which support the view that the acromioclavicular joint has some degree of rotational movements[18]. To this end, we designed this MAAP which can both effectively fix the acromioclavicular joint and retain its micro-movable features. Moreover, the MAAP is a limited contact plate, which can minimize the impact of the blood supply to the periosteum and cortex.
The use of MAAP described here is a novel technique that can provide a simple and effective internal fixation for the acromioclavicular joint dislocation. In this series of 16 patients, 12 had excellent clinical results, 3 had good results and only one had a satisfactory result. According to our experience, it is very important to consider at least three points to reduce the incidence of complications. First, the fixing screw should not be too long beyond the lower edge of the acromion, which should be made at the posterior medial side of the acromion and at least three screws are needed to fix the acromial side. If the screws are located at relatively anterior side of the acromion, activities of the humerus will be prone to increase the risk of screws cut-out and plate migration. Second, it is best to conventionally remove the MAAP later than 3 months after surgery. Long-term MAAP retention will increase the considerable risk of complications, such as plate breakage, screws cut-out, acromion fracture, and rotator cuff damage. Third, to prevent excessive acromioclavicular joint activities, patients should be asked to avoid adduction and outreach greater than 90° as possible until the MAAP is removed. To our delights, no infection was observed in our series.
The limitation of our study is that we could not give clear evidence by magnetic resonance imaging (MRI) examination that the healing of the coracoclavicular ligament was attributed to the use of MAAP maintained the stability of acromioclavicular joint, as it was extremely difficult to convince the patient after removal of MAAP to do the expensive MRI examination. In addition, one drawback of fixation technique is the need for a second surgical procedure for MAAP removal, otherwise, complications such as frequent shoulder pain, screws breakage et al are prone to occur.
In conclusion, all patients were able to return to their daily activities without any noticeable complication. We believe that fixation with MAAP in the surgical treatment of acute complete acromioclavicular joint dislocations is an effective method in achieving satisfactory shoulder functions, with lower complication rate. However, it is necessary to continue to observe the clinical effects of this fixation technique.
Acknowledgements
This work was supported by ”Eleventh Five-Year” scientific research Project of Nanjing Military Region; contract grant number: 06NA100.
Conflict of Interest
The authors declare that they have no conflict of interest related to the publication of this manuscript.
References
1. Tossy JD, Mead NC, Sigmond HM. Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res. 1963;28:111-9
2. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160-4
3. Pavlik A, Csepai D, Hidas P. Surgical treatment of chronic acromioclavicular joint dislocation by modified Weaver-Dunn procedure. Knee Surg Sports Traumatol Arthrosc. 2001;9(5):307-12
4. Sethi GK, Scott SM. Subclavian artery laceration due to migration of a Hagie pin. Surgery. 1976;80(5):644-6
5. NORRELL H Jr, LLEWELLYN RC. Migration of a Threaded Steinmann Pin from an Acromioclavicular Joint into the Spinal Canal:A CASE REPORT. J Bone Joint Surg Am. 1965;47(5):1024-6
6. Charity RM, Haidar SG, Ghosh S, Tillu AB. Fixation failure of the clavicular hook plate: a report of three cases. J Orthop Surg (Hong Kong). 2006;14(3):333-5
7. Chaudry SN, Waseem M. Clavicular hook plate: complications of retaining the implant. Injury. 2006;37(7):665
8. Sim E, Schwarz N, Hocker K, Berzlanovich A. Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Clin Orthop Relat Res. 1995;314:134-42
9. Esenyel CZ, Ozturk K, Bulbul M, Ayanoglu S, Ceylan HH. Coracoclavicular ligament repair and screw fixation in acromioclavicular dislocations. Acta Orthop Traumatol Turc. 2010;44(3):194-8
10. Assaghir YM. Outcome of exact anatomic repair and coracoclavicular cortical lag screw in acute acromioclavicular dislocations. J Trauma. 2011;71(3):E50-4
11. Simovitch R, Sanders B, Ozbaydar M, Lavery K, Warner JJ. Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg. 2009;17(4):207-19
12. El SMT, El AH. Suture repair using loop technique in cases of acute complete acromioclavicular joint dislocation. J Orthop Traumatol. 2011;12(1):29-35
13. Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54(6):1187-94
14. Morrison DS, Lemos MJ. Acromioclavicular separation. Reconstruction using synthetic loop augmentation. Am J Sports Med. 1995;23(1):105-10
15. Baumgarten KM, Altchek DW, Cordasco FA. Arthroscopically assisted acromioclavicular joint reconstruction. Arthroscopy. 2006;22(2):228.e1-228.e6
16. Duan X, Zhang H, Zhang H, Wang Z. Treatment of coracoid process fractures associated with acromioclavicular dislocation using clavicular hook plate and coracoid screws. J Shoulder Elbow Surg. 2010;19(2):e22-5
17. Moseley HF. The clavicle: its anatomy and function. Clin Orthop Relat Res. 1968;58:17-27
18. Sahara W, Sugamoto K, Murai M, Yoshikawa H. Three-dimensional clavicular and acromioclavicular rotations during arm abduction using vertically open MRI. J Orthop Res. 2007;25(9):1243-9
Author contact
![]() Corresponding author: Jianyun Miao, 268 Zhang-Hua Road, Zhangzhou, 363000, Fujian Province, China. Tel & Fax: +86-596-2931538; E-mail: miaojianyuncom
Corresponding author: Jianyun Miao, 268 Zhang-Hua Road, Zhangzhou, 363000, Fujian Province, China. Tel & Fax: +86-596-2931538; E-mail: miaojianyuncom

 Global reach, higher impact
Global reach, higher impact