3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2025; 22(9):2237-2246. doi:10.7150/ijms.108744 This issue Cite
Research Paper
Risks of cardiovascular disease and cerebrovascular disease following kidney transplantation: A nationwide, population-based cohort study
1. Department of Health Services Administration, China Medical University, Taichung 406040, Taiwan.
2. School of Medicine, Chung Shan Medical University, Taichung 40201, Taiwan.
3. Department of Medical Education, Linkou Chang-Gung Memorial Hospital, Taoyuan City 333, Taiwan.
4. Department of Business Administration, National Taiwan University, Taipei 106, Taiwan.
5. Department of Pharmacy, Chung Shan Medical University Hospital, Taichung 40201, Taiwan.
6. Department of Pharmacology, Chung Shan Medical University, Taichung 40201, Taiwan.
† These authors contributed equally to this work and share the first authorship.
‡ These authors contributed equally to this work and share the correspondence authorship.
Received 2024-12-13; Accepted 2025-3-24; Published 2025-4-13
Abstract
Background: Kidney transplant recipients (KTRs) have an increased risk for cardiovascular disease (CVD) and cerebrovascular disease (CBD). This study investigated the risks of CVD and CBD following kidney transplantation.
Materials and methods: This retrospective cohort study enrolled 3596 KTRs between 2003 and 2017. Propensity Score Matching (PSM) was performed to select patients without a kidney transplant, who were assigned to the control group. Each KTR was matched with five patients without a kidney transplant by sex, age, insured salary, urbanization level, Charlson comorbidity index (CCI), and year of inclusion in the study. A Cox proportional hazards model was employed to investigate the risks of incident CVD and CBD in KTRs after adjusting for relevant variables. Furthermore, we analyzed for CVD and CBD risk 6 months and 1, 3, and 5 years after transplantation.
Results: Among KTRs, the CVD incidence rate per 1,000 person-years was 33.98, which was significantly higher than that among patients without a kidney transplant. After adjusting for confounding variables, KTRs had a significantly higher risk of CVD (adjusted hazard ratio [aHR], 1.74; 95% confidence interval [CI], 1.58-1.93) than did patients without a kidney transplant. Regarding cumulative incidence, the risk of CVD increased over time. Among the four follow-up periods we assessed, the 5-year follow-up period had the highest CVD risk (aHR, 1.35; 95% CI, 1.17-1.56), followed by the 3-year follow-up period (aHR, 1.34; 95% CI, 1.13-1.59). KTRs also had a significantly higher risk of CBD (aHR, 1.43; 95% CI, 1.23-1.68) than did patients without a kidney transplant.
Conclusion: CVD risk is higher among KTRs than among those without a kidney transplant, and this risk increases over time. CBD risk was also higher among KTRs. Large, randomized controlled prospective studies are needed to thoroughly evaluate the relationship between kidney transplantation and the risks of CVD and CBD.
Keywords: cardiovascular disease, cerebrovascular disease, kidney transplant recipient, cohort study, real-world evidence
Introduction
Kidney transplantation is the most effective treatment for patients with irreversible chronic kidney disease [1]. Kidney transplantation yields better outcomes in terms of quality of life and mortality risk compared with dialysis [2]. The most common cause of graft failure is death with a functioning graft. Cardiovascular disease (CVD), infections, and cancer are the leading causes of death in kidney transplant recipients (KTRs) [3].
Observational studies and substantial evidence show that CVD is more prevalent among KTRs than in the general population [4], [5, 6]. Dialysis poses a greater risk of cardiovascular mortality than does kidney transplantation [7, 8]. CVD is the leading cause of morbidity and mortality among KTRs and the primary reason for posttransplant hospitalization [9]. CVD poses a threat to the long-term survival of KTRs [10]. New-onset cerebrovascular disease (CBD) is relatively common among KTRs [11-15]. All forms of CBD are linked to increased mortality risk [14]. Clinicians must understand the risks of CVD and CBD following kidney transplantation to prevent complications. Accordingly, this retrospective cohort study investigated the risks of CVD and CBD following kidney transplantation between 2003 and 2017. Data were obtained from Taiwan's National Health Insurance Research Database (NHIRD).
Materials and methods
Data sources
This study conducted a secondary analysis of the 2002-2022 NHIRD. The NHIRD is managed by Taiwan's Ministry of Health and Welfare. The NHIRD contains data for all beneficiaries covered by the National Health Insurance program, a government-run, single-payer National Health Insurance program established in 1995. This insurance program covers approximately 99% of Taiwan's population. Disease diagnoses within the database are coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) systems. Before 2015, diagnoses were reported using ICD-9-CM, while from 2016 onward, ICD-10-CM has been used. The NHIRD is commonly employed to inform clinical decision-making and health-care policy development [16, 17].
Ethics approval
Data in the NHIRD are anonymized; therefore, this study was exempt from the need to obtain informed consent. The study protocol received ethical approval from the Institutional Review Board of Chung Shan Medical University Hospital, Taiwan (No. CSMUH CS2-21134).
Study participants
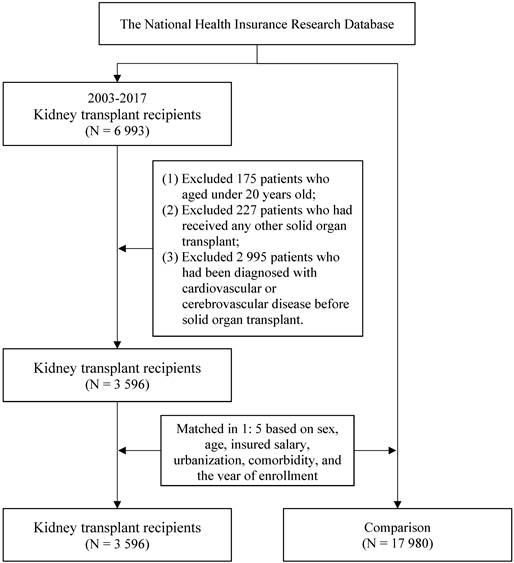
The study enrolled patients aged older than 20 years who received a kidney transplant between 2003 and 2017. Kidney transplantation was identified using ICD-9-CM code V42.0 and ICD-10-CM code Z94.0. In Taiwan, organ transplantation is classified as a major catastrophic illness under the National Health Insurance (NHI) program. Patients who have successfully undergone organ transplantation receive a catastrophic illness certificate. Considering potential factors such as surgical failure or overseas transplantation, this study identified kidney transplant recipients using diagnosis codes from the catastrophic illness registry instead of procedure codes. The index date for kidney transplant patients was defined based on the 'effective start date' recorded in the registry, marking the beginning of the observation period. Patients were excluded if they had received any other solid organ transplant or had a CVD or CBD before receiving a kidney transplant. The control group consisted of individuals who had not undergone organ transplantation during the study period. To reduce potential confounding caused by unbalanced covariates in non-experimental settings, we employed 1:5 propensity score matching for each KTR based on the year of enrollment (i.e., 2003, 2004, 2005, until 2017) to establish a matched cohort. To minimize bias, only individuals without a prior diagnosis of cardiovascular disease (CVD) or cerebrovascular disease (CBD) before the enrollment year were eligible for inclusion in the control group. A propensity score is a probability that is calculated using a logistic regression model. The score is a unit of a certain characteristic assigned to a patient who received a kidney transplant. These scores can help reduce or eliminate selection bias in observational studies by accounting for the characteristics of control individuals. Sex, age, insured salary, urbanization level, and Charlson comorbidity index (CCI) were selected as characteristics for matching. Specifically, an optimized matching approach was used with a caliper width of 0.2 of the pooled standard deviation of the logit of the propensity score. If a control subject had experienced the outcome event prior to matching, they were completely excluded from the analysis. Additionally, subjects that could not be successfully matched were also excluded to ensure the integrity of the comparison. This approach ensured comparability between groups and improved the validity of our findings. After matching, the study comprised 3596 KTRs (KTR group) and 17 980 patients without a kidney transplant (control group). The patient selection process is presented in Figure 1.
Flowchart of the patient selection process
Study design
This retrospective cohort study investigated the risk of CVD and CBD by using data from Taiwan's NHIRD. The CVDs investigated comprised acute myocardial infarction (ICD-9-CM 410; ICD-10-CM I21-I22), atrial fibrillation (ICD-9-CM 427.31; ICD-10-CM I48.0, II48.1, I48.2, I48.91), ischemic heart disease (ICD-9-CM 410-414; ICD-10-CM I20-I25), heart failure (ICD-9-CM 428; ICD-10-CM I50), and peripheral artery disease (ICD-9-CM 443.9; ICD-10-CM I73.9). CBD comprised ischemic stroke (ICD-9-CM 443-435, 437; ICD-10-CM G45, G46, I63, I65-I67, I69) and hemorrhagic stroke (ICD-9-CM 430-432; ICD-10-CM I60-I62). The definitions of CVD and CBD were based on diagnostic criteria requiring at least three occurrences as a principal diagnosis in outpatient records or at least one occurrence as any listed diagnosis during hospitalization within the follow-up period. The incident date of CVD or CBD was defined as the date of the first recorded diagnosis. The approval date of KTR was defined as the start of the observation period. For the matched comparison group, the same date was assigned as the start of the observation period. All patients were followed up from the observation start date until death, diagnosis of CVD, CBD, or the end date of 2022.
The control variables included sex, age, insured salary, urbanization level, CCI, and related comorbidities. Age was categorized as ≤40, 41-50, 51-60, and ≥61 years. Insured salary was categorized into four groups: ≤ 19,200, 19,201-22,800, 22,801-42,000, and ≥ 42,001 New Taiwan Dollars (NTD). For urbanization level, we classified the insured regions of study subjects into seven levels based on previous research definitions, with level 1 being the highest and level 7 the lowest [18]. CCI was categorized as 0, 1, 2, and ≥ 3. The comorbidities included in our analysis were hypertension (ICD-9-CM 401-405; ICD-10-CM I10-I13, I15), hyperlipidemia (ICD-9-CM 272; ICD-10-CM E78), diabetes mellitus (ICD-9-CM 250; ICD-10-CM E10-E14), chronic kidney disease (ICD-9-CM 585; ICD-10-CM N18), hyperuricemia (ICD-9-CM 790.6; ICD-10-CM E79.0), anxiety (ICD-9-CM 300.0; ICD-10-CM F40-F41), depression (ICD-9-CM 296.2-296.3; ICD-10-CM F32-F33), and sleep disturbance (ICD-9-CM 780; ICD-10-CM G47.9).
Statistical analysis
All statistical analyses were conducted using SAS software version 9.4 (SAS Institute, Cary, NC, USA). Statistical significance was indicated by p < .05. Chi-square tests were used to compare the distributions of baseline characteristics between KTRs and patients without a kidney transplant. Since the number and proportion of deaths during the follow-up period were lower than those of CVD events, we treated death as a censoring event rather than a competing event. A Cox proportional hazards model was employed to investigate the risk of incident CVD and CBD in KTRs after adjustment for all relevant variables. Results are presented as hazard ratios (HRs) with 95% confidence intervals (CIs). The risks of incident CVD and CBD following kidney transplantation may change over time; therefore, we conducted a sensitivity analysis to estimate the risks of CVD and CBD over several follow-up periods, namely 6 months and 1, 3, and 5 years.
Results
The baseline characteristics of the participants are given in Table 1. In total, 49.25% of the KTRs were men, and the mean age of KTRs was 45.69 ± 11.30 years. Furthermore, 32.81%, 31.65%, 26.28%, and 9.26% of KTRs were aged ≤40, 41-50, 51-60, and ≥61 years, respectively. After propensity score matching, no significant differences in sex, age, insured salary, urbanization, and CCI between the groups were observed (p > 0.05). Among KTRs, 54.06% had hypertension, 6.03% had hyperlipidemia, 14.40% had diabetes mellitus, 66.60% had chronic kidney disease, and 1.06% had depression. The distribution of the aforementioned comorbidities in the KTR group significantly differed from that in the control group (p < .001).
Distribution of baseline characteristics of kidney transplant recipients and the comparison.
| Variables | Total | Comparison | Kidney transplant recipients | p-value | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Total | 21,576 | 100.00 | 17,980 | 100.00 | 3,596 | 100.00 | |
| Sex 1 | 0.995 | ||||||
| Female | 10,951 | 50.76 | 9,126 | 50.76 | 1,825 | 50.75 | |
| Male | 10,625 | 49.24 | 8,854 | 49.24 | 1,771 | 49.25 | |
| Age (year) 1 | 1.000 | ||||||
| ≤40 | 7,096 | 32.89 | 5,916 | 32.90 | 1,180 | 32.81 | |
| 41-50 | 6,816 | 31.59 | 5,678 | 31.58 | 1,138 | 31.65 | |
| 51-60 | 5,671 | 26.28 | 4,726 | 26.28 | 945 | 26.28 | |
| ≥61 | 1,993 | 9.24 | 1,660 | 9.23 | 333 | 9.26 | |
| Mean ± SD | 45.36 ± 14.27 | 45.30 ± 14.80 | 45.69 ± 11.30 | ||||
| Insured salary (NTD.) 1 | 0.999 | ||||||
| ≤19,200 | 7,105 | 32.93 | 5,922 | 32.94 | 1,183 | 32.90 | |
| 19,201-22,800 | 4,435 | 20.56 | 3,694 | 20.55 | 741 | 20.61 | |
| 22,801-42,000 | 5,439 | 25.21 | 4,535 | 25.22 | 904 | 25.14 | |
| ≥42,001 | 4,597 | 21.31 | 3,829 | 21.30 | 768 | 21.36 | |
| Urbanization 1 | 1.000 | ||||||
| Level 1 | 7,111 | 32.96 | 5,921 | 32.93 | 1,190 | 33.09 | |
| Level 2 | 7,313 | 33.89 | 6,095 | 33.90 | 1,218 | 33.87 | |
| Level 3 | 3,279 | 15.20 | 2,731 | 15.19 | 548 | 15.24 | |
| Level 4 | 2,548 | 11.81 | 2,125 | 11.82 | 423 | 11.76 | |
| Level 5 | 303 | 1.40 | 253 | 1.41 | 50 | 1.39 | |
| Level 6 | 480 | 2.22 | 402 | 2.24 | 78 | 2.17 | |
| Level 7 | 542 | 2.51 | 453 | 2.52 | 89 | 2.47 | |
| CCI score 1 | 1.000 | ||||||
| 0 | 2,083 | 9.65 | 1,735 | 9.65 | 348 | 9.68 | |
| 1 | 875 | 4.06 | 730 | 4.06 | 145 | 4.03 | |
| 2 | 9,189 | 42.59 | 7,657 | 42.59 | 1,532 | 42.60 | |
| ≥3 | 9,429 | 43.70 | 7,858 | 43.70 | 1,571 | 43.69 | |
| Enrolled year 1 | 1.000 | ||||||
| 2003 | 2,376 | 11.01 | 1,980 | 11.01 | 396 | 11.01 | |
| 2004 | 2,064 | 9.57 | 1,720 | 9.57 | 344 | 9.57 | |
| 2005 | 1,938 | 8.98 | 1,615 | 8.98 | 323 | 8.98 | |
| 2006 | 1,800 | 8.34 | 1,500 | 8.34 | 300 | 8.34 | |
| 2007 | 1,530 | 7.09 | 1,275 | 7.09 | 255 | 7.09 | |
| 2008 | 1,458 | 6.76 | 1,215 | 6.76 | 243 | 6.76 | |
| 2009 | 1,320 | 6.12 | 1,100 | 6.12 | 220 | 6.12 | |
| 2010 | 1,290 | 5.98 | 1,075 | 5.98 | 215 | 5.98 | |
| 2011 | 1,260 | 5.84 | 1,050 | 5.84 | 210 | 5.84 | |
| 2012 | 1,116 | 5.17 | 930 | 5.17 | 186 | 5.17 | |
| 2013 | 1,026 | 4.76 | 855 | 4.76 | 171 | 4.76 | |
| 2014 | 1,140 | 5.28 | 950 | 5.28 | 190 | 5.28 | |
| 2015 | 1,140 | 5.28 | 950 | 5.28 | 190 | 5.28 | |
| 2016 | 978 | 4.53 | 815 | 4.53 | 163 | 4.53 | |
| 2017 | 1,140 | 5.28 | 950 | 5.28 | 190 | 5.28 | |
| Comorbidities | |||||||
| Hypertension | <0.001 | ||||||
| No | 16,346 | 75.76 | 14,694 | 81.72 | 1,652 | 45.94 | |
| Yes | 5,230 | 24.24 | 3,286 | 18.28 | 1,944 | 54.06 | |
| Hyperlipidemia | 0.005 | ||||||
| No | 20,037 | 92.87 | 16,658 | 92.65 | 3,379 | 93.97 | |
| Yes | 1,539 | 7.13 | 1,322 | 7.35 | 217 | 6.03 | |
| Diabetes mellitus | <0.001 | ||||||
| No | 17,081 | 79.17 | 14,003 | 77.88 | 3,078 | 85.60 | |
| Yes | 4,495 | 20.83 | 3,977 | 22.12 | 518 | 14.40 | |
| Chronic kidney disease | <0.001 | ||||||
| No | 18,308 | 84.85 | 17,107 | 95.14 | 1,201 | 33.40 | |
| Yes | 3,268 | 15.15 | 873 | 4.86 | 2,395 | 66.60 | |
| Hyperuricemia | <0.001 | ||||||
| No | 21,399 | 99.18 | 17,898 | 99.54 | 3,501 | 97.36 | |
| Yes | 177 | 0.82 | 82 | 0.46 | 95 | 2.64 | |
| Anxiety | <0.001 | ||||||
| No | 20,787 | 96.34 | 17,251 | 95.95 | 3,536 | 98.33 | |
| Yes | 789 | 3.66 | 729 | 4.05 | 60 | 1.67 | |
| Depression | <0.001 | ||||||
| No | 21,148 | 98.02 | 17,590 | 97.83 | 3,558 | 98.94 | |
| Yes | 428 | 1.98 | 390 | 2.17 | 38 | 1.06 | |
| Sleep disturbance | 0.002 | ||||||
| No | 18,327 | 84.94 | 15,334 | 85.28 | 2,993 | 83.23 | |
| Yes | 3,249 | 15.06 | 2,646 | 14.72 | 603 | 16.77 | |
1 Variables for propensity score matching.
CVD incidence rates are shown in Table 2. The average follow-up duration was 10.02 ± 5.58 years. In total, 4424 patients (20.50%) developed CVD, and the CVD incidence rate per 1,000 person-years was 19.58. Among KTRs, the CVD incidence rate per 1,000 person-years was 33.98, which was significantly higher than that in the control group (p < .001). CVD incidence increased with age. Hypertension, hyperlipidemia, diabetes mellitus, or chronic kidney disease increased the risk of CVD.
Findings on CVD risk are shown in Table 3. After confounding variables were adjusted for, the risk of CVD was found to be significantly higher in the KTR group (adjusted HR [aHR], 1.74; 95% CI, 1.58-1.93) than in the control group. The risk of CVD was higher among men (aHR, 1.18; 95% CI, 1.12-1.26) than among women. The risk of CVD was increased by the following comorbidities: hypertension (aHR, 1.18; 95% CI, 1.10-1.26), hyperuricemia (aHR, 1.19; 95% CI, 1.07-1.33), diabetes mellitus (aHR, 1.28; 95% CI, 1.19-1.38), and chronic kidney disease (aHR, 1.16; 95% CI, 1.04-1.29).
Findings on CVD risk stratified by follow-up duration are shown in Table 4. The KTR group had a higher risk of CVD than did the control group during 3-year (aHR, 1.34; 95% CI, 1.13-1.59) and 5-year (aHR, 1.35; 95% CI, 1.17-1.56) follow-up windows.
CBD risk is shown in Table 5. After confounding variables were adjusted for, the risk of CBD was found to be significantly higher in the KTR group (aHR, 1.43; 95% CI, 1.23-1.68) than in the control group. The KTR group had a lower risk of CBD than did the control group within a 6-month follow-up window (aHR, 0.53; 95% CI, 0.28-0.99) and a higher risk of CBD in a 5-year follow-up window (aHR, 1.26; 95% CI, 1.01-1.57).
Discussion
This large-scale retrospective observational study provides real-world findings regarding the risk of CVD following kidney transplantation. The study demonstrated that CVD risk was higher in the KTR group than in the control group and that KTRs with comorbid hypertension, hyperlipidemia, diabetes mellitus, chronic kidney disease, and depression were at further risk. Male sex and older age were risk factors for CVD, and this risk increased over time following transplantation. CBD risk was also higher in the KTR group than in the control group.
Incidence rate of cardiovascular disease.
| Variables | Cardiovascular disease | |||
|---|---|---|---|---|
| Events | % | IR 1 | p-value | |
| Total | 4,424 | 20.50 | 19.58 | |
| Patients | <0.001 | |||
| Comparison | 3,292 | 18.31 | 17.09 | |
| Kidney transplant recipients | 1,132 | 31.48 | 33.98 | |
| Sex | 0.007 | |||
| Female | 2,166 | 19.78 | 18.19 | |
| Male | 2,258 | 21.25 | 21.12 | |
| Age (year) | <0.001 | |||
| ≤40 | 1,026 | 14.46 | 12.31 | |
| 41-50 | 1,637 | 24.02 | 22.28 | |
| 51-60 | 1,388 | 24.48 | 25.56 | |
| ≥61 | 373 | 18.72 | 25.09 | |
| Insured salary (NTD.) | <0.001 | |||
| ≤19,200 | 1,594 | 22.43 | 20.29 | |
| 19,201-22,800 | 772 | 17.41 | 18.05 | |
| 22,801-42,000 | 1,132 | 20.81 | 19.55 | |
| ≥42,001 | 926 | 20.14 | 19.80 | |
| Urbanization | 0.036 | |||
| Level 1 | 1,499 | 21.08 | 19.93 | |
| Level 2 | 1,535 | 20.99 | 19.95 | |
| Level 3 | 605 | 18.45 | 18.01 | |
| Level 4 | 505 | 19.82 | 19.00 | |
| Level 5 | 59 | 19.47 | 19.10 | |
| Level 6 | 98 | 20.42 | 20.67 | |
| Level 7 | 123 | 22.69 | 21.07 | |
| CCI score | <0.001 | |||
| 0 | 339 | 16.27 | 12.70 | |
| 1 | 185 | 21.14 | 17.60 | |
| 2 | 2,003 | 21.80 | 20.22 | |
| ≥3 | 1,897 | 20.12 | 21.15 | |
| Comorbidities | ||||
| Hypertension | <0.001 | |||
| No | 3,038 | 18.59 | 17.01 | |
| Yes | 1,386 | 26.50 | 29.25 | |
| Hyperlipidemia | <0.001 | |||
| No | 4,031 | 20.12 | 19.10 | |
| Yes | 393 | 25.54 | 26.42 | |
| Diabetes mellitus | <0.001 | |||
| No | 3,321 | 19.44 | 17.98 | |
| Yes | 1,103 | 24.54 | 27 | |
| Chronic kidney disease | <0.001 | |||
| No | 3,463 | 18.92 | 17.54 | |
| Yes | 961 | 29.41 | 33.63 | |
| Hyperuricemia | <0.001 | |||
| No | 4,367 | 20.41 | 19.46 | |
| Yes | 57 | 32.20 | 36.23 | |
| Anxiety | 0.803 | |||
| No | 4,265 | 20.52 | 19.57 | |
| Yes | 159 | 20.15 | 19.70 | |
| Depression | 0.216 | |||
| No | 4,326 | 20.46 | 19.49 | |
| Yes | 98 | 22.90 | 24.78 | |
| Sleep disturbance | 0.002 | |||
| No | 3,692 | 20.15 | 19.11 | |
| Yes | 732 | 22.53 | 22.34 | |
1 Incidence rate per 1,000 person-year.
Risk estimated for incident cardiovascular disease using the Cox proportional hazards model.
| Variables | Cardiovascular disease | ||||
|---|---|---|---|---|---|
| Adjusted HR | 95% CI | p-value | |||
| Patients | |||||
| Comparison (ref.) | 1 | ||||
| Kidney transplant recipients | 1.74 | 1.58 | - | 1.93 | <0.001 |
| Sex | |||||
| Female (ref.) | 1 | ||||
| Male | 1.18 | 1.12 | - | 1.26 | <0.001 |
| Age (year) | |||||
| ≤40 (ref.) | 1 | ||||
| 41-50 | 1.78 | 1.64 | - | 1.92 | <0.001 |
| 51-60 | 1.97 | 1.81 | - | 2.14 | <0.001 |
| ≥61 | 1.82 | 1.61 | - | 2.05 | <0.001 |
| Insured salary (NTD) | |||||
| ≤19,200 (ref.) | 1 | ||||
| 19,201-22,800 | 0.86 | 0.79 | - | 0.94 | 0.001 |
| 22,801-42,000 | 0.93 | 0.87 | - | 1.01 | 0.084 |
| ≥42,001 | 0.86 | 0.79 | - | 0.93 | 0.000 |
| Urbanization | |||||
| Level 1 (ref.) | 1 | ||||
| Level 2 | 0.98 | 0.91 | - | 1.05 | 0.560 |
| Level 3 | 0.89 | 0.81 | - | 0.98 | 0.021 |
| Level 4 | 0.96 | 0.87 | - | 1.07 | 0.486 |
| Level 5 | 0.92 | 0.71 | - | 1.19 | 0.519 |
| Level 6 | 0.94 | 0.77 | - | 1.16 | 0.569 |
| Level 7 | 1.06 | 0.88 | - | 1.27 | 0.559 |
| CCI score | |||||
| 0 (ref.) | 1 | ||||
| 1 | 1.24 | 1.04 | - | 1.49 | 0.019 |
| 2 | 1.44 | 1.28 | - | 1.63 | <0.001 |
| ≥3 | 1.35 | 1.20 | - | 1.53 | <0.001 |
| Comorbidities (Yes vs No [ref.]) | |||||
| Hypertension | 1.18 | 1.10 | - | 1.26 | <0.001 |
| Hyperlipidemia | 1.19 | 1.07 | - | 1.33 | 0.001 |
| Diabetes mellitus | 1.28 | 1.19 | - | 1.38 | <0.001 |
| Chronic kidney disease | 1.16 | 1.04 | - | 1.29 | 0.007 |
| Hyperuricemia | 1.25 | 0.96 | - | 1.63 | 0.098 |
| Anxiety | 0.98 | 0.84 | - | 1.15 | 0.820 |
| Depression | 1.25 | 1.02 | - | 1.53 | 0.030 |
| Sleep disturbance | 1.06 | 0.98 | - | 1.15 | 0.145 |
Analysis for cardiovascular disease risk at different follow-up times.
| Variables | Cardiovascular disease | ||||||
|---|---|---|---|---|---|---|---|
| Events | % | Adjusted HR | 95% CI | p-value | |||
| In 6 months | |||||||
| Patients | |||||||
| Comparison (ref.) | 300 | 1.67 | 1 | ||||
| Kidney transplant recipients | 79 | 2.20 | 1.23 | 0.86 | - | 1.75 | 0.253 |
| In 1 year | |||||||
| Patients | |||||||
| Comparison (ref.) | 512 | 2.85 | 1 | ||||
| Kidney transplant recipients | 138 | 3.84 | 1.10 | 0.84 | - | 1.44 | 0.479 |
| In 3 years | |||||||
| Patients | |||||||
| Comparison (ref.) | 1,081 | 6.01 | 1 | ||||
| Kidney transplant recipients | 355 | 9.87 | 1.34 | 1.13 | - | 1.59 | <0.001 |
| In 5 years | |||||||
| Patients | |||||||
| Comparison (ref.) | 1,589 | 8.84 | 1 | ||||
| Kidney transplant recipients | 506 | 14.07 | 1.35 | 1.17 | - | 1.56 | <0.001 |
Risk estimated for incident cerebrovascular disease using the Cox proportional hazards model.
| Variables | Cerebrovascular Disease | ||||
|---|---|---|---|---|---|
| Adjusted HR | 95% CI | p-value | |||
| Patients | |||||
| Comparison (ref.) | 1 | ||||
| Kidney transplant recipients | 1.43 | 1.23 | - | 1.68 | <0.001 |
| At different follow-up time | |||||
| In 6 months | |||||
| Comparison (ref.) | 1 | ||||
| Kidney transplant recipients | 0.53 | 0.28 | - | 0.99 | 0.049 |
| In 1 year | |||||
| Comparison (ref.) | 1 | ||||
| Kidney transplant recipients | 0.82 | 0.52 | - | 1.30 | 0.394 |
| In 3 years | |||||
| Comparison (ref.) | 1 | ||||
| Kidney transplant recipients | 1.07 | 0.81 | - | 1.41 | 0.658 |
| In 5 years | |||||
| Comparison (ref.) | 1 | ||||
| Kidney transplant recipients | 1.26 | 1.01 | - | 1.57 | 0.048 |
The risks of CVD and mortality are lower among KTRs than among patients receiving dialysis. Nevertheless, these risks are higher among KTRs than in the general population [19]. KTRs have double the risk of cardiovascular mortality compared with the general population [20, 21]. The high incidence of CVD after kidney transplantation is primarily due to the presence and accumulation of traditional risk factors both before and after the transplant [22].
Male and older-adult KTRs, especially those aged 51-60 years, have a higher risk of CVD. The incidence of CV remains high after transplantation. A study using survival model analysis identified the following as key predictors of cardiovascular events in KTRs: male sex, older age, previous CVD, pretransplant smoking, and posttransplant diabetes mellitus [23]. These factors increase the risk of cardiovascular events [23]. Age and sex are risk factors for vascular disease [24]. CVD accounts for one-third of all deaths following transplantation, with individuals aged 50 years or older facing a significantly higher risk than the general population [9].
KTRs with comorbid hypertension, hyperlipidemia, diabetes mellitus, chronic kidney disease, and depression had a higher risk of CVD than did KTRs without these comorbidities. Traditional cardiovascular risk factors, such as hyperlipidemia, hypertension, and diabetes mellitus, are common in KTRs, partly due to the effects of immunosuppressive drugs. These factors contribute to adverse outcomes and increase the burden of CVD after transplantation [14, 25]. Hypertension is a major risk factor for atherosclerotic CVD, which is the leading cause of premature death and a major factor in graft failure among transplant recipients [26]. Although hypertension is a significant risk factor for renal graft survival, controlling hypertension alone does not seem to improve outcomes. Graft survival is more affected by the severity of graft dysfunction at the start of observation, regardless of blood pressure control [27]. Dyslipidemia is common among KTRs, even when renal function remains normal or nearly normal [28]. Dyslipidemia is an important risk factor for CVD [29]. The prevalence of hyperlipidemia among KTRs has been estimated to reach up to 80% [30]. Abnormal glucose metabolism significantly increases the risk of fatal and nonfatal cardiovascular events [31], with a threefold higher risk of cardiac death or nonfatal acute myocardial infarction compared with patients without diabetes [32]. Patients with pretransplant diabetes mellitus (PreDM) had an increased risk of mortality from cardiovascular diseases compared to those without diabetes [33, 34]. Another study also indicted that PreDM patients have the highest incidence of major adverse cardiovascular events and cardiac-related mortality following transplantation [35]. Patients with PreDM experienced significantly lower survival rates, with up to a 50% higher risk of death while on the transplant waiting list and a 70% increased risk of CVD and all-cause mortality [36, 37]. Chronic kidney disease increases the risk of death among KTRs, and KTRs with chronic kidney disease are more likely to require dialysis than are KTRs without chronic kidney disease [38]. CVD is a significant cause of morbidity and mortality among patients with chronic kidney disease [21]. Progressive renal dysfunction increases the risk of cardiovascular complications following transplantation [4]. Chronic kidney disease increases the risk of adverse outcomes, with CVD being the leading cause of death in this population [39]. Cardiovascular mortality increases as kidney function declines, even after adjusting for traditional risk factors, indicating that chronic kidney disease is an independent risk factor for CVD [40]. In advanced chronic kidney disease stages (3b-4), 40%-45% of patients die from CVD rather than progressing to end-stage kidney disease requiring transplantation or dialysis [41]. Depression and anxiety are consistently identified as the most prevalent psychiatric disorders among organ donors following donation [42]. Anxiety and depression are associated with higher morbidity following kidney transplantation [43]. A meta-analysis associated depression but not anxiety with an increased risk of posttransplant mortality [44]. Despite progress in renal transplantation, depression is still a common and problematic comorbidity that remains largely overlooked. In this context, depression is associated with poorer outcomes, including reduced graft survival [45].
CVD risk increased over time following kidney transplantation. Among the four follow-up periods we assessed, the 5-year follow-up period had the highest CVD risk, followed by the 3-year follow-up period. CVD has become a major contributor to graft loss, especially after the first year following transplantation [4]. We applied competing risk methodology and found that the cumulative incidence of cardiovascular events was 5.0% at 1 year after transplantation, 8.1% at 5 years, and 11.9% at 10 years [23]. The cumulative incidence of posttransplant myocardial infarction was 4.3% following transplantation, 4.1%-4.5% at 6 months, 5.6% at 12 months, and 11.1% at 36 months [46]. The cumulative incidence of coronary heart disease following transplantation was 3.1% at 1 year, 5.2% at 3 years, and 7.6% at 5 years [47].
Our study indicates that the risk of CBD was higher in KTRs compared to non-transplant patients during the 5-year follow-up period. In contrast, the 6-month follow-up period was associated with a lower CBD risk (aHR 0.53, 95% CI: 0.28-0.99). However, the lower limit of the confidence interval is close to negligible. The incidence of posttransplantation stroke in KTRs varies from 1.1% to 8.0% [11-15]. Single-center studies have demonstrated the adverse mortality implications of posttransplantation cerebrovascular disease events in KTRs [13, 48]. The cumulative 3-year incidence of new-onset cerebrovascular events after kidney transplantation was 6.8%. Among patients on the waiting list, this incidence was 11.8%, and among those with graft loss, this was 11.2% [14]. Transplantation reduced the risk of cerebrovascular events by 34% compared with remaining on the waiting list, and the risk of cerebrovascular events increased by more than 150% after graft failure [14]. Cerebrovascular events are associated with negative implications for mortality [14]. Kidney function within the first year after transplantation has consistently been recognized as an important factor that affects longer-term graft survival [49, 50]. KTRs experience a gradual decline in glomerular filtration rate over time, which is strongly associated with donor age and aortic stiffness after the first year following transplantation [51]. A study has shown evidence of the involvement of kidney disease in both the early and later phases of cerebrovascular atherosclerosis and cerebral small vessel disease [52]. Kidney dysfunction was linked to an increased risk of stroke, regardless of the etiological subtype [53]. The incidence of stroke in KTRs was 5% in the first year following transplantation and 9.4% in the second year [15]. This study revealed that the incidence of stroke was relatively lower in the early stages after transplantation but increased in the later stages. Our research shows that the risk of CBD was higher in KTRs than in non-transplant patients over the 5-year follow-up period. On the other hand, the 6-month follow-up period was linked to a lower risk of CBD. This may be associated with initial improvement in kidney function in the early post-transplant period, followed by a gradual decline over time. However, further well-designed controlled prospective studies are needed to confirm whether CBD risk continues to increase over time following kidney transplantation.
CVD risk was higher in the KTR group than in the control group, and this risk increased over time. CBD risk was also higher in the KTR group. Clinicians must comprehensively understand the risks of CVD and CBD following kidney transplantation to minimize complications.
The present study has several strengths. First, it used a nationwide, population-based sample, selecting patients from the entire Taiwanese population and following them over a long period. This approach provided a large, representative sample with high statistical value and minimized selection bias. Second, we investigated the risks of CVD and CBD in KTRs at different time points after transplantation (i.e., 6 months and 1, 3, and 5 years).
This study has some limitations. First, selective reporting bias and data errors may have resulted from the study's retrospective cohort design. Second, the study used the NHIRD, which is a secondary database. Because the NHIRD lacks laboratory details and medical examination data, we were unable to evaluate diagnostic criteria. Third, the NHIRD lacks data on smoking habits, alcohol consumption, body mass index, personal medical history, physical activity, and dietary habits, all of which are linked to CVD and CBD risk. Fourth, all diagnoses in this study were based on ICD-9-CM or ICD-10-CM classifications. Taiwan's Bureau of National Health Insurance enhances diagnostic accuracy by randomly reviewing charts and conducting patient interviews, ensuring that analyses using NHIRD data are valid and accurate. Nonetheless, we acknowledge that some confounding variables may not have been controlled for in this study. Last, some comorbidities, such as metabolic syndrome, obesity, and obstructive sleep apnea, are associated with the occurrence of CVD and CBD. However, due to the limited number of patients with these conditions, their inclusion could lead to overdispersion in the regression analyses. Therefore, they were not incorporated into this study. This study focused on the incidence of CVD and CBD after kidney transplantation, without further analysis of the underlying reasons for transplantation. While end-stage renal disease (ESRD) is the most common indication, other conditions, such as congenital anomalies, genetic disorders, or rare kidney diseases, may also lead to kidney transplantation. Different transplantation indications could potentially influence post-transplant CVD and CBD risk. Future studies should consider incorporating the causes of transplantation to better understand their impact on cardiovascular and cerebrovascular outcomes.
Acknowledgements
We are grateful to China Medical University Taiwan, Chung Shan Medical University Taiwan, and Chung Shan Medical University Hospital Taiwan for providing administrative, technical, and funding support that has contributed to the completion of this study. This study is based, in part, on data released by the Health and Welfare Data Science Center, Ministry of Health and Welfare Taiwan. The interpretation and conclusions contained herein do not represent those of the Ministry of Health and Welfare Taiwan.
Funding
This research was supported by the Chung Shan Medical University Hospital Taiwan (CSH-2015-C-012), China Medical University Taiwan (CMU113-MF-120 and CMU113-S-42), and the National Science and Technology Council Taiwan (NSTC 113-2410-H-040-001).
Author contributions
Conceptualization: Tung-Han Tsai, Kuang-Hua Huang, Min-Ling Tsai, Chien-Ying Lee; Formal analysis: Hsin Chen, Shuo-Yan Gau, Kun-Yu Su; Methodology: Tung-Han Tsai, Kuang-Hua Huang, Hsin Chen, Min-Ling Tsai, Chien-Ying Lee; Validation: Min-Ling Tsai and Chien-Ying Lee; Writing - original draft: Tung-Han Tsai, Kuang-Hua Huang, Min-Ling Tsai, Chien-Ying Lee; Writing - review & editing: Tung-Han Tsai, Kuang-Hua Huang, Hsin Chen, Shuo-Yan Gau, Kun-Yu Su, Min-Ling Tsai, Chien-Ying Lee.
Data availability statement
The database used to support the findings of this study was provided by the Health and Welfare Data Science Center, Ministry of Health and Welfare (HWDC, MOHW) under license and so cannot be made freely available. Requests for access to these data should be made to HWDC (https://dep.mohw.gov.tw/dos/cp-5119-59201-113.html).
Competing Interests
The authors have declared that no competing interest exists.
References
1. Chaudhry D, Chaudhry A, Peracha J, Sharif A. Survival for waitlisted kidney failure patients receiving transplantation versus remaining on waiting list: systematic review and meta-analysis. BMJ. 2022;376:e068769
2. Ojo AO, Port FK, Wolfe RA, Mauger EA, Williams L, Berling DP. Comparative mortality risks of chronic dialysis and cadaveric transplantation in black end-stage renal disease patients. Am J Kidney Dis. 1994;24:59-64
3. El-Zoghby ZM, Stegall MD, Lager DJ, Kremers WK, Amer H, Gloor JM. et al. Identifying specific causes of kidney allograft loss. Am J Transplant. 2009;9:527-35
4. Montanaro D, Gropuzzo M, Tulissi P, Boscutti G, Risaliti A, Baccarani U. et al. [Cardiovascular disease after renal transplantation]. G Ital Nefrol. 2004;21(Suppl 26):S53-66
5. Pita-Fernandez S, Pertega-Diaz S, Valdes-Canedo F, Seijo-Bestilleiro R, Seoane-Pillado T, Fernandez-Rivera C. et al. Incidence of cardiovascular events after kidney transplantation and cardiovascular risk scores: study protocol. BMC Cardiovasc Disord. 2011;11:2
6. Carpenter MA, Weir MR, Adey DB, House AA, Bostom AG, Kusek JW. Inadequacy of cardiovascular risk factor management in chronic kidney transplantation - evidence from the FAVORIT study. Clin Transplant. 2012;26:E438-46
7. Lee RA, Gabardi S. Current trends in immunosuppressive therapies for renal transplant recipients. Am J Health Syst Pharm. 2012;69:1961-75
8. Neale J, Smith AC. Cardiovascular risk factors following renal transplant. World J Transplant. 2015;5:183-95
9. Birdwell KA, Park M. Post-Transplant Cardiovascular Disease. Clin J Am Soc Nephrol. 2021;16:1878-89
10. Young JB, Neumayer HH, Gordon RD. Pretransplant cardiovascular evaluation and posttransplant cardiovascular risk. Kidney Int Suppl. 2010(118):S1-7
11. Huang ST, Yu TM, Chuang YW, Chung MC, Wang CY, Fu PK. et al. The Risk of Stroke in Kidney Transplant Recipients with End-Stage Kidney Disease. Int J Environ Res Public Health. 2019;16:326
12. Aull-Watschinger S, Konstantin H, Demetriou D, Schillinger M, Habicht A, Horl WH. et al. Pre-transplant predictors of cerebrovascular events after kidney transplantation. Nephrol Dial Transplant. 2008;23:1429-35
13. Oliveras A, Roquer J, Puig JM, Rodriguez A, Mir M, Orfila MA. et al. Stroke in renal transplant recipients: epidemiology, predictive risk factors and outcome. Clin Transplant. 2003;17:1-8
14. Lentine KL, Rocca Rey LA, Kolli S, Bacchi G, Schnitzler MA, Abbott KC. et al. Variations in the risk for cerebrovascular events after kidney transplant compared with experience on the waiting list and after graft failure. Clin J Am Soc Nephrol. 2008;3:1090-101
15. Saran R, Robinson B, Abbott KC, Agodoa LYC, Bhave N, Bragg-Gresham J. et al. US Renal Data System 2017 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis. 2018;71:A7
16. Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH. et al. Taiwan's National Health Insurance Research Database: past and future. Clin Epidemiol. 2019;11:349-58
17. Lai SW, Liao KF, Lin CL, Lin CC, Lin CH. Longitudinal data of multimorbidity and polypharmacy in older adults in Taiwan from 2000 to 2013. Biomedicine (Taipei). 2020;10:1-4
18. Liu C-Y, Hung Y-T, Chuang Y-L, Chen Y-J, Weng W-S, Liu J-S. et al. Incorporating Development Stratification of Taiwan Townships into Sampling Design of Large Scale Health Interview Survey [in Tradionnal Chinese]. Journal of Health Management. 2006;4:1-22
19. Parajuli S, Mandelbrot DA, Aziz F, Garg N, Muth B, Mohamed M. et al. Characteristics and Outcomes of Kidney Transplant Recipients with a Functioning Graft for More than 25 Years. Kidney Dis (Basel). 2018;4:255-61
20. Foley RN, Parfrey PS, Sarnak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis. 1998;32:S112-9
21. Sarnak MJ, Levey AS. Cardiovascular disease and chronic renal disease: a new paradigm. Am J Kidney Dis. 2000;35:S117-31
22. Fazelzadeh A, Mehdizadeh A, Ostovan MA, Raiss-Jalali GA. Incidence of cardiovascular risk factors and complications before and after kidney transplantation. Transplant Proc. 2006;38:506-8
23. Seoane-Pillado MT, Pita-Fernandez S, Valdes-Canedo F, Seijo-Bestilleiro R, Pertega-Diaz S, Fernandez-Rivera C. et al. Incidence of cardiovascular events and associated risk factors in kidney transplant patients: a competing risks survival analysis. BMC Cardiovasc Disord. 2017;17:72
24. Kasiske BL, Guijarro C, Massy ZA, Wiederkehr MR, Ma JZ. Cardiovascular disease after renal transplantation. J Am Soc Nephrol. 1996;7:158-65
25. Jardine AG, Gaston RS, Fellstrom BC, Holdaas H. Prevention of cardiovascular disease in adult recipients of kidney transplants. Lancet. 2011;378:1419-27
26. Mangray M, Vella JP. Hypertension after kidney transplant. Am J Kidney Dis. 2011;57:331-41
27. Cheigh JS, Haschemeyer RH, Wang JC, Riggio RR, Tapia L, Stenzel KH. et al. Hypertension in kidney transplant recipients. Effect on long-term renal allograft survival. Am J Hypertens. 1989;2:341-8
28. Kasiske B, Cosio FG, Beto J, Bolton K, Chavers BM, Grimm R Jr. et al. Clinical practice guidelines for managing dyslipidemias in kidney transplant patients: a report from the Managing Dyslipidemias in Chronic Kidney Disease Work Group of the National Kidney Foundation Kidney Disease Outcomes Quality Initiative. Am J Transplant. 2004;4(Suppl 7):13-53
29. Hosseini MS, Rostami Z, Einollahi B. Dyslipidemia after kidney transplantation and correlation with cyclosporine level. Nephrourol Mon. 2013;5:831-4
30. Gonyea JE, Anderson CF. Weight change and serum lipoproteins in recipients of renal allografts. Mayo Clin Proc. 1992;67:653-7
31. Cosio FG, Kudva Y, van der Velde M, Larson TS, Textor SC, Griffin MD. et al. New onset hyperglycemia and diabetes are associated with increased cardiovascular risk after kidney transplantation. Kidney Int. 2005;67:2415-21
32. Hjelmesaeth J, Hartmann A, Leivestad T, Holdaas H, Sagedal S, Olstad M. et al. The impact of early-diagnosed new-onset post-transplantation diabetes mellitus on survival and major cardiac events. Kidney Int. 2006;69:588-95
33. Dos Santos Q, Hornum M, Terrones-Campos C, Crone CG, Wareham NE, Soeborg A. et al. Posttransplantation Diabetes Mellitus Among Solid Organ Recipients in a Danish Cohort. Transpl Int. 2022;35:10352
34. Yeh H, Lin C, Li YR, Yen CL, Lee CC, Chen JS. et al. Temporal trends of incident diabetes mellitus and subsequent outcomes in patients receiving kidney transplantation: a national cohort study in Taiwan. Diabetol Metab Syndr. 2020;12:34
35. Lim WH, Lok CE, Kim SJ, Knoll G, Shah BR, Naylor K. et al. Impact of Pretransplant and New-Onset Diabetes After Transplantation on the Risk of Major Adverse Cardiovascular Events in Kidney Transplant Recipients: A Population-based Cohort Study. Transplantation. 2021;105:2470-81
36. Lim WH, Wong G, Pilmore HL, McDonald SP, Chadban SJ. Long-term outcomes of kidney transplantation in people with type 2 diabetes: a population cohort study. Lancet Diabetes Endocrinol. 2017;5:26-33
37. Lee S, Yoo KD, An JN, Oh YK, Lim CS, Kim YS. et al. Factors affecting mortality during the waiting time for kidney transplantation: A nationwide population-based cohort study using the Korean Network for Organ Sharing (KONOS) database. PLoS One. 2019;14:e0212748
38. Carminatti M, Tedesco-Silva H, Silva Fernandes NM, Sanders-Pinheiro H. Chronic kidney disease progression in kidney transplant recipients: A focus on traditional risk factors. Nephrology (Carlton). 2019;24:141-7
39. Matsushita K, Ballew SH, Wang AY, Kalyesubula R, Schaeffner E, Agarwal R. Epidemiology and risk of cardiovascular disease in populations with chronic kidney disease. Nat Rev Nephrol. 2022;18:696-707
40. Matsushita K, Coresh J, Sang Y, Chalmers J, Fox C, Guallar E. et al. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol. 2015;3:514-25
41. Thompson S, James M, Wiebe N, Hemmelgarn B, Manns B, Klarenbach S. et al. Cause of Death in Patients with Reduced Kidney Function. J Am Soc Nephrol. 2015;26:2504-11
42. Heinrich TW, Marcangelo M. Psychiatric issues in solid organ transplantation. Harv Rev Psychiatry. 2009;17:398-406
43. Noohi S, Khaghani-Zadeh M, Javadipour M, Assari S, Najafi M, Ebrahiminia M. et al. Anxiety and depression are correlated with higher morbidity after kidney transplantation. Transplant Proc. 2007;39:1074-8
44. Dew MA, Rosenberger EM, Myaskovsky L, DiMartini AF, DeVito Dabbs AJ, Posluszny DM. et al. Depression and Anxiety as Risk Factors for Morbidity and Mortality After Organ Transplantation: A Systematic Review and Meta-Analysis. Transplantation. 2015;100:988-1003
45. Chilcot J, Spencer BW, Maple H, Mamode N. Depression and kidney transplantation. Transplantation. 2014;97:717-21
46. Lentine KL, Brennan DC, Schnitzler MA. Incidence and predictors of myocardial infarction after kidney transplantation. J Am Soc Nephrol. 2005;16:496-506
47. Israni AK, Snyder JJ, Skeans MA, Peng Y, Maclean JR, Weinhandl ED. et al. Predicting coronary heart disease after kidney transplantation: Patient Outcomes in Renal Transplantation (PORT) Study. Am J Transplant. 2010;10:338-53
48. de Mattos AM, Prather J, Olyaei AJ, Shibagaki Y, Keith DS, Mori M. et al. Cardiovascular events following renal transplantation: role of traditional and transplant-specific risk factors. Kidney Int. 2006;70:757-64
49. Hariharan S, McBride MA, Cherikh WS, Tolleris CB, Bresnahan BA, Johnson CP. Post-transplant renal function in the first year predicts long-term kidney transplant survival. Kidney Int. 2002;62:311-8
50. Schold JD, Nordyke RJ, Wu Z, Corvino F, Wang W, Mohan S. Clinical Events and Renal Function in the First Year Predict Long-Term Kidney Transplant Survival. Kidney360. 2022;3:714-27
51. Bahous SA, Khairallah M, Al Danaf J, Halaby R, Korjian S, Daaboul Y. et al. Renal function decline in recipients and donors of kidney grafts: role of aortic stiffness. Am J Nephrol. 2015;41:57-65
52. van der Velde M, Matsushita K, Coresh J, Astor BC, Woodward M, Levey A. et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int. 2011;79:1341-52
53. Marini S, Georgakis MK, Anderson CD. Interactions Between Kidney Function and Cerebrovascular Disease: Vessel Pathology That Fires Together Wires Together. Front Neurol. 2021;12:785273
Author contact
![]() Corresponding author: Chien-Ying Lee, PhD, Department of Pharmacology, Chung Shan Medical University, No.110, Sec.1, Jianguo N. Rd., Taichung City 40201, Taiwan. Tel: 886-4-24730022 #11664 E-mail: cshd015edu.tw.
Corresponding author: Chien-Ying Lee, PhD, Department of Pharmacology, Chung Shan Medical University, No.110, Sec.1, Jianguo N. Rd., Taichung City 40201, Taiwan. Tel: 886-4-24730022 #11664 E-mail: cshd015edu.tw.

 Global reach, higher impact
Global reach, higher impact