3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2025; 22(5):1176-1183. doi:10.7150/ijms.108261 This issue Cite
Research Paper
The association between aortic stenosis and the risk of consecutive eyelid inflammatory diseases
1. Institute of Medicine, Chung Shan Medical University, Taichung, Taiwan.
2. Division of Cardiology, Department of Internal Medicine, Camillian Saint Mary's Hospital Luodong, Luodong, Yilan, Taiwan.
3. Division of Cardiology, Department of Internal Medicine, Changhua Christian Hospital, Yunlin Branch, Yunlin, Taiwan.
4. Department of Nursing, Hungkuang University, Taichung, Taiwan.
5. Department of Post-Baccalaureate Medicine, College of Medicine, National Chung Hsing University, Taichung, Taiwan.
6. Nobel Eye Institute, Taipei, Taiwan.
7. Department of Medical Research, Chung Shan Medical University Hospital, Taichung, Taiwan.
8. Department of Emergency Medicine, School of Medicine, Chung Shan Medical University, Taichung, Taiwan.
9. Department of Emergency Medicine, Chung Shan Medical University Hospital, Taichung, Taiwan.
10. Department of Food and Beverage Services, Tainan University of Technology, Tainan, Taiwan.
Received 2024-12-5; Accepted 2025-2-6; Published 2025-2-18
Abstract
Aortic stenosis (AS) is a fatal cardiovascular disease characterized by an inflammatory response. Blepharitis and hordeolum are two eyelid conditions that also involve ocular inflammation. The aim of this study is to assess the association between AS and the subsequent development of eyelid inflammatory diseases. This retrospective cohort study included individuals diagnosed with AS, who were matched to a control group of non-AS individuals from the TriNetX database. A total of 431,027 individuals were assigned to both the AS and non-AS groups. The primary outcomes of this study were the incidence rates of eyelid inflammatory diseases, including blepharitis and hordeolum. Cox proportional hazards regression was used for statistical analysis. After the follow-up period, 4,464 cases of blepharitis were recorded in the AS group, compared to 3,139 in the non-AS group. Additionally, there were 2,184 cases of hordeolum in the AS group, compared to 1,724 in the non-AS group. Cox proportional hazards regression analysis revealed that the AS group had a significantly higher risk of developing blepharitis (P < 0.001) and hordeolum (P < 0.001) compared to the non-AS group. The AS group also showed significantly higher cumulative probabilities of both blepharitis and hordeolum than the non-AS group (both P < 0.001). In subgroup analyses, AS patients exhibited a higher risk of developing blepharitis than the non-AS population, except for the Asian population and individuals aged 20-45 years. Similarly, the AS group showed a higher risk of developing hordeolum than the non-AS group, with exceptions in the African and Asian populations and individuals aged 20-45 years. In conclusion, the presence of AS is associated with a higher risk of developing subsequent eyelid inflammatory diseases.
Keywords: aortic stenosis, blepharitis, hordeolum, epidemiology, TriNetX database
Introduction
Aortic stenosis (AS) is a significant cardiovascular disease characterized by fibrosis, calcification, and thickening of the aortic valve structure [1, 2]. In Western countries, the prevalence of AS is estimated to be 5 percent in individuals over the age of 65 [3]. Medical management is typically used for mild cases of AS, while surgery, such as aortic valve replacement, is recommended for more severe cases [4, 5]. Although the survival rate following aortic valve replacement is generally favorable [6, 7], postoperative complications related to AS can lead to mortality [3].
The association between AS and several other diseases has been well-documented [2]. For instance, diabetes mellitus is frequently observed in individuals with AS [8]. Additionally, hypertension is closely linked to the development of AS, and the coexistence of hypertension can impact both the symptoms and severity of AS [9]. In terms of serum lipids, hypercholesterolemia can damage the cardiovascular system, and dyslipidemia has been shown to influence the formation and progression of AS [10]. Beyond these metabolic conditions, elevated inflammatory responses and cytokine levels have also been observed during the development of AS [11].
Blepharitis is an eyelid inflammatory disease caused by dysfunction of the meibomian glands, which can lead to ocular irritation and subsequently dry eye disorder [12, 13]. Hordeolum, another acute eyelid disorder, is characterized by eyelid swelling, microbial infection, and an inflammatory response [14, 15]. However, there is limited research examining the association between AS and subsequent eyelid disorders. Since AS is commonly associated with systemic inflammation [16], the inflammatory response in AS may extend beyond the cardiovascular system, potentially affecting other organs, including the eyes. As a result, the presence of AS could influence the risk of developing eyelid inflammatory diseases such as blepharitis or hordeolum, necessitating further investigation. Additionally, shared risk factors, along with the effects of AS on blood flow and immune responses, may contribute to the development of eyelid inflammation, highlighting the importance of exploring this potential relationship. Thus, the purpose of this study is to evaluate the potential association between AS and subsequent eyelid inflammatory diseases, including blepharitis and hordeolum. Subgroup analyses based on demographic and laboratory data were also conducted.
Materials and Methods
Data source
TriNetX is a global federated health research network giving access to many electronic medical records (diagnoses, medications, laboratory values, procedures, genomic information) across prominent healthcare organizations. This research was generated using the US Collaborative Network, which involves 67 healthcare institutes. The medical data available in the TriNetX database involve the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes, sex, age, occupation, place of residence, educational level, socioeconomic condition, length of hospitalization if existed, laboratory examination codes, image exam codes, the surgery codes, the procedure codes, and the Anatomical Therapeutic Chemical (ATC) codes for medications. This study was approved by the Institute Review Board of Chung Shan Medical University Hospital (project code: CS2-23180).
Individual selection
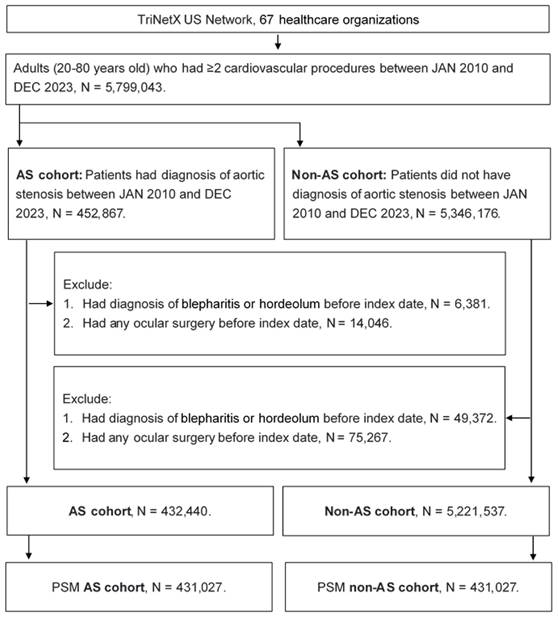
A cohort study was conducted, and individuals with the following characteristics were selected as AS cases: (1) a diagnosis of AS based on the relevant ICD-10 CM codes, (2) the receipt of an echocardiogram, electrocardiogram, chest X-ray, cardiac catheterization, or cardiac computed tomography prior to the AS diagnosis, and (3) the AS diagnosis was confirmed by a cardiologist. The index date in this study was defined as 6 months after the AS diagnosis. Exclusion criteria were applied to enhance the homogeneity of our study population: (1) individuals aged under 20 or over 80 years, (2) those who had undergone ocular surgery prior to the index date, and (3) those who experienced the outcome (described in the following section) before the index date. For the comparison, each individual with AS was matched to an individual without AS using the propensity score matching (PSM) process. The PSM process incorporates demographic information, systemic diseases, and medication use into a specific score and matches individuals based on these scores. After the process, a total of 431,027 and 431,027 individuals were put into the AS and non-AS groups, respectively. The flowchart of selection is revealed in Figure 1.
Main outcome
The main outcomes of this study are the development of blepharitis and hordeolum. The blepharitis development was set as the subsequent conditions: (1) the receipt of blepharitis diagnosis by the related ICD-10 CM codes, (2) the arrangement of slit-lamp biomicroscope exam at the same day of blepharitis diagnosis by the procedure code, and (3) the prescription of antibiotic eyedrop or ointment by the ATC codes. In addition, the hordeolum development was set as the subsequent conditions: (1) the receipt of the hordeolum diagnosis by the related ICD-10 CM codes, (2) the arrangement of slit-lamp biomicroscope exam by the procedure codes, and (3) the application of topical antibiotic eyedrop or ointment by the ATC codes. Only the blepharitis and hordeolum episodes that developed after the index date were regarded as the outcome achievements in this study. All the individuals were followed until the outcome development, individual withdraw from all the available health insurance project or the end of TriNetX database which indicates the December, 31, 2023.
The flowchart of participant selection. AS: aortic stenosis, N: number, PSM: propensity score matching.
Confounder adjustment
To better verify the association between AS and later eyelid inflammatory diseases, the effect of these confounders were adjusted in the multivariable analysis: age, urbanization, sex, income level, hypertension, hyperlipidemia, diabetes, ischemic heart disease, cerebrovascular disease, chronic kidney disease, chronic lower respiratory diseases, peripheral vascular disease, estimated glomerular filtration rate (eGFR), LDL, HDL, and Troponin I. The presence of above covariates is based on the related demographic, ICD-10 CM and laboratory codes. To confirm the durations of systemic morbidities are long enough to influence the possibility of eyelid inflammatory diseases, only the morbidities that persisted for longer than two years were chosen into the statistical analysis of this study.
Statistical analysis
The SAS version 9.4 (SAS Institute Inc, Cary, NC, USA) was exploited in the statistical analyses in this study. The descriptive analysis was exploited to show the basic features of the AS group and the non-AS group, and the standard mean difference (SMD) was exploited to evaluate the difference of each index between the two groups. A SMD more than 0.1 was defied as significant difference in this study. Then the Cox proportional hazard regression was exploited to compare the incidences of blepharitis and hordeolum between the AS and non-AS groups, and the adjusted hazard ratio (aHR) with 95% confidence interval (CI) for the incidences of eyelid inflammatory diseases were produced. The Kaplan-Meier curve was pictured and the cumulative incidences of eyelid inflammatory diseases episodes between the two groups were calculated by the log-rank test. In the subgroup analysis, the patients were categorized into different subgroup based on age, sex, HDL, LDL and eGFR. Then the Cox proportional hazard regression was exploited again to analyze the risk of eyelid inflammatory diseases in different subgroups. Statistical significance was set as P < 0.05 and the P value beneath 0.001 was described as P < 0.001 in this study.
Results
The initial features of the study population is illustrated in the Table 1. The mean age was 65.1±11.7 and 65.6±11.3 years old in the AS and non-AS groups, respectively. The difference of mean age between groups did not reach significant difference. The distributions of sex and urbanization were also similar between the two groups (both SMD < 0.1). About the systemic conditions, the rate of systemic diseases and laboratory data did not achieve significant difference between the AS and non-AS groups (all SMD < 0.1) (Table 1).
Baseline characteristics among aortic stenosis cohort and control cohort
| Characteristics | AS cohort | Control cohort | SMD |
|---|---|---|---|
| N | 431027 | 431027 | |
| Age at Index | 65.1±11.7 | 65.6±11.3 | 0.0385 |
| Sex | |||
| Female | 181869 (42.2%) | 179975 (41.8%) | 0.0089 |
| Male | 236436 (54.9%) | 236865 (55.0%) | 0.0020 |
| Race | |||
| White | 320968 (74.5%) | 325208 (75.5%) | 0.0227 |
| Black or African American | 46247 (10.7%) | 43532 (10.1%) | 0.0206 |
| Asian | 12340 (2.9%) | 11174 (2.6%) | 0.0166 |
| Comorbidities | |||
| Hypertensive diseases | 287680 (66.7%) | 291080 (67.5%) | 0.0168 |
| Dyslipidemia | 214894 (49.9%) | 216622 (50.3%) | 0.0080 |
| Ischemic heart diseases | 174353 (40.5%) | 173865 (40.3%) | 0.0023 |
| Diabetes mellitus | 120962 (28.1%) | 119623 (27.8%) | 0.0069 |
| Chronic kidney disease | 106658 (24.7%) | 102937 (23.9%) | 0.0201 |
| Peripheral vascular disease | 98052 (22.7%) | 94618 (22.0%) | 0.0191 |
| Chronic lower respiratory diseases | 80255 (18.6%) | 77223 (17.9%) | 0.0182 |
| Cerebrovascular diseases | 68052 (15.8%) | 65215 (15.1%) | 0.0182 |
| Diseases of liver | 35786 (8.3%) | 31642 (7.3%) | 0.0358 |
| Cerebrovascular disease | 486 (0.1%) | 805 (0.2%) | 0.0191 |
| Lab data | |||
| eGFR | 67.4±30.6 | 66.9±29.7 | 0.0176 |
| HDL | 46.4±18.5 | 46.4±18.6 | 0.0047 |
| LDL | 92.6±39.9 | 96.4±40.7 | 0.0941 |
| Troponin | 1.3±10.5 | 1.6±12.7 | 0.0249 |
AS: aortic stenosis, eGFR: estimated glomerular filtration rate, N: number, SMD: standard mean difference
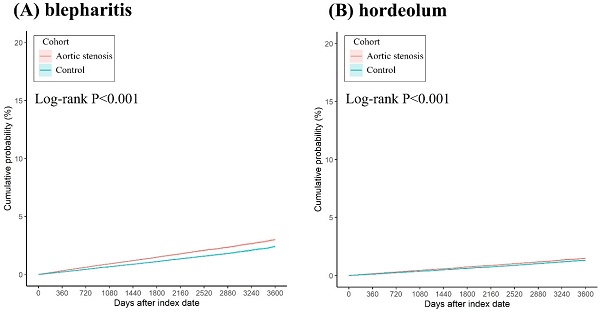
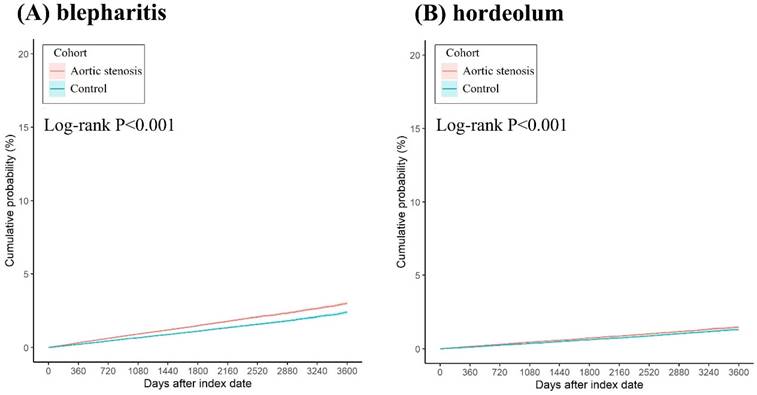
After the follow up interval, a total of 6,165 and 4,546 eyelid inflammatory diseases were found in the AS and non-AS group. There were 4,464 and 3,139 blepharitis events in the AS and non-AS groups, respectively. In addition, there was 2,184 and 1,724 hordeolum events in the AS and non-AS groups, respectively. According to the Cox proportional hazard regression, the AS group revealed a significantly higher risk of blepharitis development (aHR: 1.331, 95% CI: 1.271-1.393, P < 0.001) than the non-AS groups (Table 2). Also, the risk of hordeolum was significantly higher in the AS group (aHR: 1.183, 95% CI: 1.111-1.260, P < 0.001) than the non-AS group (Table 2). The cumulative probabilities of blepharitis and hordeolum between groups are displayed in Figures 2A-2B. The AS group revealed a significantly higher cumulative probabilities of blepharitis and hordeolum than the non-AS group (all P < 0.001) (Figures 2A-2B).
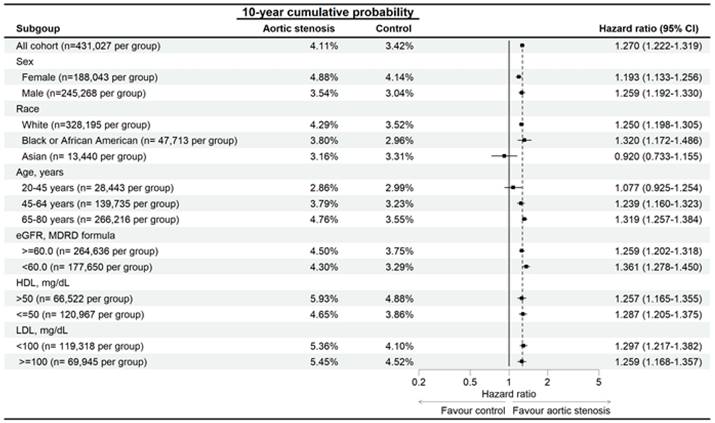
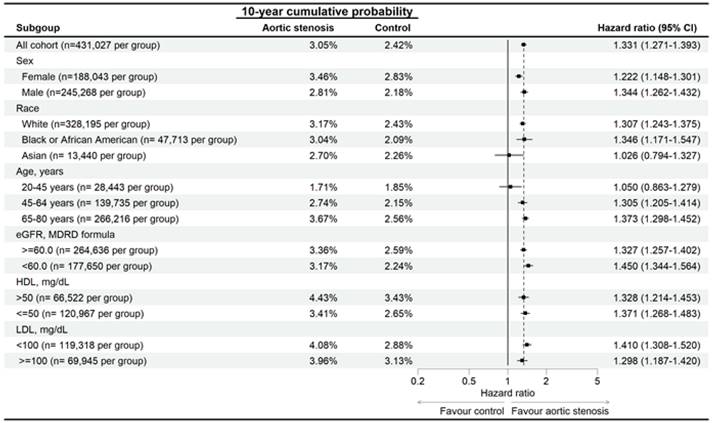
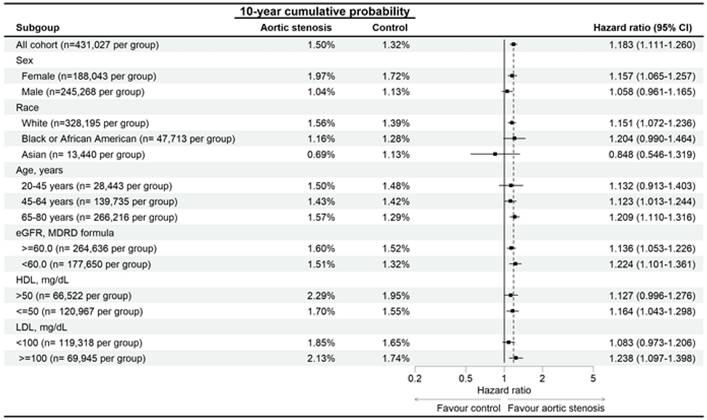
In the subgroup analysis, the AS patients with different characteristics demonstrated higher risk of developing eyelid inflammatory diseases than the non-AS population with same characteristics except the Asian population and those aged from 20-45 years (Figure 3). In addition, the AS patients also demonstrated higher risk of developing blepharitis than the non-AS population except for the Asian population and those aged from 20-45 years (Figure 4). On the other side, the AS subgroups revealed higher risk of hordeolum than the non-AS subgroup except for the African population, Asian population and those aged from 20-45 years (Figure 5).
Discussion
In this study, the AS population demonstrated a significantly higher risk of blepharitis and hordeolum developments compared to the non-AS group after considering multiple demographic and disease factors. Moreover, the probability of developing eyelid inflammatory diseases in the AS groups was positively associated with disease interval. On the other hand, the correlation between AS and following eyelid inflammatory diseases are prominent in different populations except for the Asian population and individuals aged from 20-45 years.
The AS can associate with multiple diseases throughout the human body [17]. The metabolic syndromes which referred to hypertension, glucose intolerance, and the dyslipidemia presented positive correlation to the existence of AS [18]. Both the hypertension and hyperlipidemia would develop more common in the individuals with AS [9, 10]. Moreover, the incidence of diabetes would elevate in the individuals diagnosed with AS, and the diabetes individuals with AS illustrated an advanced aortic valve calcification than the non-diabetes people [8]. In addition to the metabolic syndromes, the malignancy like prostate cancer was found more frequently in the individuals with AS [19]. Besides, the inflammatory reaction is an important factor for the formation of AS in which the inflammation and lipid deposition are two major mechanisms of the initial phase in the AS formation [20, 21]. There are some inflammatory biomarkers that could increase under the condition of AS [22]. The expression of both tumor growth factor beta and interleukin-6 would increase in the individuals with AS [23], and the nuclear factor-kappa B and bone morphogenic protein routes were significantly enhanced in the process of AS development [20]. About the eyelid inflammatory diseases, the blepharitis resulted from the dysfunction and inflammation of meibomian gland [12], and the pro-inflammatory protein HMGB1 could elevated in the individuals diagnosed with blepharitis [24]. On the other hand, the hordeolum also owns inflammatory nature in which the inflammatory response of the eyelid margin was observed in the individuals with hordeolum [25]. Since both the AS and eyelid inflammatory diseases including blepharitis and hordeolum associate with the inflammatory reaction [12, 15, 25], the higher baseline inflammatory status in the individuals with AS may increase the rate of subsequent eyelid inflammatory diseases. This speculation was supported by the findings of this study at least to some extents.
The Kaplan-Meier curve and cumulative incidence of (A) blepharitis events, and (B) hordeolum events between groups.
Risk of eyelid inflammatory diseases in patients with aortic stenosis stratified by age, sex, race, HDL, and LDL levels. N: number
Risk of blepharitis in patients with aortic stenosis stratified by age, sex, race, HDL, and LDL levels. N: number
Risk of hordeolum in patients with aortic stenosis stratified by age, sex, race, HDL, and LDL levels. N: number
Main outcomes between the two groups
| Study event | N | Cumulative probability | Hazard ratio (95% CI) | P | |||
|---|---|---|---|---|---|---|---|
| 1-year | 3-years | 5-years | 10-years | ||||
| All events | |||||||
| AS | 6,165 | 0.44% | 1.27% | 2.07% | 4.05% | 1.270 (1.222-1.319) | <0.001* |
| Control | 4,546 | 0.31% | 0.98% | 1.61% | 3.38% | Reference | |
| Blepharitis | |||||||
| AS | 4,464 | 0.32% | 0.91% | 1.49% | 2.99% | 1.331 (1.271-1.393) | <0.001* |
| Control | 3,139 | 0.21% | 0.66% | 1.11% | 2.38% | Reference | |
| Hordeolum | |||||||
| AS | 2,184 | 0.15% | 0.45% | 0.73% | 1.47% | 1.183 (1.111-1.260) | <0.001* |
| Control | 1,724 | 0.11% | 0.37% | 0.61% | 1.31% | Reference | |
aHR: adjusted hazard ratio, AS: aortic stenosis, CI: confidence interval, N: number
* denotes significant difference between groups
The existence of AS correlated to higher incidence of blepharitis and hordeolum in this study. About the correlation between eyelid diseases and systemic diseases, the presence of coronary heart disease was significantly related to the higher incidence of subsequent blepharitis [26]. In addition, the recurrent hordeolum was found in patient with nephrotic syndrome [27]. Still, the association between AS and eyelid inflammatory diseases had not been fully surveyed. To our knowledge, our results may be a preliminary finding that the presence of AS significantly associated with the risk of succeeding blepharitis and hordeolum development. Moreover, the blepharitis and hordeolum episodes before the index date was excluded, this the time sequence between the AS and succeeding blepharitis and hordeolum may be established. Furthermore, we adjusted several confounders of blepharitis and hordeolum including the age, metabolic syndromes and the LDL/HDL concentration in the multivariable analysis. Consequently, the existence of AS may be the independent risk factor for the development of subsequent eyelid inflammatory diseases. In addition to the inflammation, the dysfunction of lipid also play a crucial role in the formation of blepharitis, hordeolum and AS [13, 16, 28], thus the higher serum lipid level in the AS may also trigger the development of succeeding blepharitis and hordeolum. About the cumulative incidences of eyelid diseases, both blepharitis and hordeolum showed a higher cumulative incidence in the AS group compared to the non-AS group. In the later years, the risk of eyelid inflammatory diseases gain 50% in the AS group compared to the similar values between groups within one year after the index date. These results may indicate the elevated risk of eyelid inflammatory diseases would be much higher in the individuals with prolonged AS than the non-AS population, which may influence the eyelid health to a higher degree.
Concerning the subgroup analysis, both the incidences of blepharitis and hordeolum were significantly higher in all the subgroups with AS except the Asian population and the individuals aged from 20-45 years. There was rare research to report such correlation. The young age was not a significant protective factor for the development of blepharitis in previous study [12], and the young adult also demonstrated average risk of developing hordeolum [25]. On the other hand, the Asian population did not present with lower risk of blepharitis or hordeolum in previous articles [25, 29], and the rate of meibomian gland dysfunction was even higher in the Asian population. The possible explanation for the relative lower risk of eyelid inflammatory diseases in this study may due to the small case numbers in the Asian population and the young age group. Both subgroups account for less than 10 percent of cases in the whole study population, thus the small case numbers may contribute to the statistical bias. On the other hand, the risk of hordeolum in the African group with AS was also similar to the African group without AS. Because the total numbers of hordeolum episodes were relative fewer compared to the total numbers of blepharitis events (only about half), the low outcome numbers of hordeolum may also cause insignificant results in the population with relative low patient numbers. The AS correlated with higher incidence of eyelid inflammatory diseases in all the other subgroups compared to the non-AS population. These results may indicate the universal influence of AS on the development of eyelid inflammatory diseases.
Regarding the epidemiology, the AS is a common cardiovascular disorder in the world and the incidence of AS is near 3 percent in individuals older than 75 years in the North America are and the health of about 4.43 percent of US population was influenced by the AS [4, 30]. Besides, the AS incidence in Chinese people aged older than 75 was more than 20 percent [31]. The aortic valve replacement had been consumed in the majority of individuals for the AS in developed countries which is a large medical cost [32]. For the surgical intervention, the operative mortality of aortic valve transplantation was more than 1 percent despite the survival time may elevate after early postoperative period [4, 11]. The blepharitis is also a prevalent disease in which about 30 percent of individuals in ophthalmic department were diagnosed with blepharitis and many of them was suffered from dry eye [12]. Also, the hordeolum may be one of the most common ocular diseases although the exact prevalence and incidence of hordeolum need further evaluation [25]. Although the medical managements are adequate for most of hordeolum, the severe hordeolum may cause periorbital cellulitis which can influence the visual acuity [14]. Since the AS, blepharitis and hordeolum influence a large portion of people and can contribute to huge socioeconomical burden, any association among them should be revealed.
There are several limitations in this study. Firstly, the TriNetX database is a claimed dataset which preserves the medical codes for the patients. Consequently, multiple important data including the site of AS, the severity of AS, the image result of AS, the surgical details of aortic valve replacement if arranged, the postoperative condition of individuals with AS if arranged, the recurrence of AS if existed, the appearance of eyelid inflammatory diseases, the meibomian gland condition of eyelid inflammatory diseases, the microorganism culture results of eyelid inflammatory diseases if arranged, the treatment outcomes of eyelid inflammatory diseases and the recurrence of eyelid inflammatory diseases if existed cannot be investigated. Secondly, there could be some individuals that had eyelid inflammatory diseases before the AS diagnosis but did not search medical assistance due to the light disease severity, thus the time sequence between AS and subsequent eyelid inflammatory diseases is not fully confirmed.
In conclusion, the existence of AS associates with higher incidence of succeeding eyelid inflammatory diseases including blepharitis and hordeolum after adjusting multiple confounders. Furthermore, the risk of developing eyelid inflammatory diseases in the AS population positively relates to the disease period of AS. Consequently, the routine ophthalmic referral may be suggested for the individuals with persistent AS. Further large-scale prospective study to evaluate the association between AS and therapeutic outcomes of eyelid inflammatory diseases is mandatory.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Phillips D. Aortic stenosis: A review. Aana j. 2006;74:309-15
2. Moncla LM, Briend M, Bossé Y, Mathieu P. Calcific aortic valve disease: mechanisms, prevention and treatment. Nat Rev Cardiol. 2023;20:546-59
3. Sawaya F, Liff D, Stewart J, Lerakis S, Babaliaros V. Aortic stenosis: a contemporary review. Am J Med Sci. 2012;343:490-6
4. Thaden JJ, Nkomo VT, Enriquez-Sarano M. The global burden of aortic stenosis. Prog Cardiovasc Dis. 2014;56:565-71
5. Kanwar A, Thaden JJ, Nkomo VT. Management of Patients With Aortic Valve Stenosis. Mayo Clin Proc. 2018;93:488-508
6. Boskovski MT, Gleason TG. Current Therapeutic Options in Aortic Stenosis. Circ Res. 2021;128:1398-417
7. Carabello BA, Paulus WJ. Aortic stenosis. Lancet. 2009;373:956-66
8. Kopytek M, Mazur P, Ząbczyk M, Undas A, Natorska J. Diabetes concomitant to aortic stenosis is associated with increased expression of NF-κB and more pronounced valve calcification. Diabetologia. 2021;64:2562-74
9. Rassa A, Zahr F. Hypertension and Aortic Stenosis: A Review. Curr Hypertens Rev. 2018;14:6-14
10. Mata P, Alonso R, Pérez de Isla L, Badimón L. Dyslipidemia and aortic valve disease. Curr Opin Lipidol. 2021;32:349-54
11. Grimard BH, Safford RE, Burns EL. Aortic Stenosis: Diagnosis and Treatment. Am Fam Physician. 2016;93:371-8
12. Amescua G, Akpek EK, Farid M, Garcia-Ferrer FJ, Lin A, Rhee MK. et al. Blepharitis Preferred Practice Pattern®. Ophthalmology. 2019;126:P56-p93
13. Bernardes TF, Bonfioli AA. Blepharitis. Semin Ophthalmol. 2010;25:79-83
14. Deibel JP, Cowling K. Ocular inflammation and infection. Emerg Med Clin North Am. 2013;31:387-97
15. Lindsley K, Nichols JJ, Dickersin K. Non-surgical interventions for acute internal hordeolum. Cochrane Database Syst Rev. 2017;1:Cd007742
16. Akahori H, Tsujino T, Masuyama T, Ishihara M. Mechanisms of aortic stenosis. J Cardiol. 2018;71:215-20
17. Yu Chen H, Dina C, Small AM, Shaffer CM, Levinson RT, Helgadóttir A. et al. Dyslipidemia, inflammation, calcification, and adiposity in aortic stenosis: a genome-wide study. Eur Heart J. 2023;44:1927-39
18. Lindman BR, Clavel MA, Mathieu P, Iung B, Lancellotti P, Otto CM. et al. Calcific aortic stenosis. Nat Rev Dis Primers. 2016;2:16006
19. Frattini S, Troise G, Fucci C, Pressman GS, Faggiano P. Aortic valve stenosis and cancer: a common and complex association. Expert Rev Cardiovasc Ther. 2021;19:289-99
20. Zheng KH, Tzolos E, Dweck MR. Pathophysiology of Aortic Stenosis and Future Perspectives for Medical Therapy. Cardiol Clin. 2020;38:1-12
21. Joseph J, Naqvi SY, Giri J, Goldberg S. Aortic Stenosis: Pathophysiology, Diagnosis, and Therapy. Am J Med. 2017;130:253-63
22. Sarkar A, Chowdhury S, Kumar A, Khan B, Chowdhury S, Gupta R. et al. Biomarkers as Prognostic Markers for Aortic Stenosis: A Review. Am J Cardiol. 2023;206:53-9
23. Goody PR, Hosen MR, Christmann D, Niepmann ST, Zietzer A, Adam M. et al. Aortic Valve Stenosis: From Basic Mechanisms to Novel Therapeutic Targets. Arterioscler Thromb Vasc Biol. 2020;40:885-900
24. Cavone L, Muzzi M, Mencucci R, Sparatore B, Pedrazzi M, Moroni F. et al. 18β-glycyrrhetic acid inhibits immune activation triggered by HMGB1, a pro-inflammatory protein found in the tear fluid during conjunctivitis and blepharitis. Ocul Immunol Inflamm. 2011;19:180-5
25. Willmann D, Guier CP, Patel BC, Melanson SW. Hordeolum (Stye). StatPearls. Treasure Island (FL) ineligible companies. Disclosure: Christian Guier declares no relevant financial relationships with ineligible companies. Disclosure: Bhupendra Patel declares no relevant financial relationships with ineligible companies. Disclosure: Scott Melanson declares no relevant financial relationships with ineligible companies.: StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC. 2024
26. Lee CY, Yang SF, Chang YL, Huang JY, Chang CK. The Degrees of Coronary Heart Disease and the Degrees of New-Onset Blepharitis: A Nationwide Cohort Study. Diagnostics (Basel). 2024;14:1349
27. Hayasaka Y, Hayasaka S, Matsukura H. Ocular findings in Japanese children with nephrotic syndrome receiving prolonged corticosteroid therapy. Ophthalmologica. 2006;220:181-5
28. Gordon AA, Danek DJ, Phelps PO. Common inflammatory and infectious conditions of the eyelid. Dis Mon. 2020;66:101042
29. Rhee MK, Yeu E, Barnett M, Rapuano CJ, Dhaliwal DK, Nichols KK. et al. Demodex Blepharitis: A Comprehensive Review of the Disease, Current Management, and Emerging Therapies. Eye Contact Lens. 2023;49:311-8
30. Peters AS, Duggan JP, Trachiotis GD, Antevil JL. Epidemiology of Valvular Heart Disease. Surg Clin North Am. 2022;102:517-28
31. Chen J, Lyu L, Shen J, Pan Y, Jing J, Wang YJ. et al. Epidemiological study of calcified aortic valve stenosis in a Chinese community population. Postgrad Med J. 2023;99:868-74
32. Harris AW, Pibarot P, Otto CM. Aortic Stenosis: Guidelines and Evidence Gaps. Cardiol Clin. 2020;38:55-63
Author contact
![]() Corresponding authors: Chia-Jui Weng, PhD, or Shun-Fa Yang, Ph.D. Institute of Medicine, Chung Shan Medical University, Taichung 402, Taiwan; Tel.: +886-4-24739595 ext. 34253; Fax: +886-4-24723229; E-mail: t10044tut.edu.tw (Chia-Jui Weng); ysfedu.tw (Shun-Fa Yang).
Corresponding authors: Chia-Jui Weng, PhD, or Shun-Fa Yang, Ph.D. Institute of Medicine, Chung Shan Medical University, Taichung 402, Taiwan; Tel.: +886-4-24739595 ext. 34253; Fax: +886-4-24723229; E-mail: t10044tut.edu.tw (Chia-Jui Weng); ysfedu.tw (Shun-Fa Yang).

 Global reach, higher impact
Global reach, higher impact