3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2025; 22(2):409-416. doi:10.7150/ijms.102667 This issue Cite
Research Paper
Short-term outcomes after robot-assisted versus open radical cystectomy for bladder cancer in patients with diabetes mellitus: an analysis of the United States Nationwide Inpatient Sample of 2005-2018
1. Department of Urology, Taipei Municipal Wan Fang Hospital, Taipei, Taiwan.
2. Doctor of medicine., Taipei Medical University, Taipei, Taiwan.
3. Department of Urology, Taipei Veterans General Hospital, Taipei, Taiwan.
4. Department of Physiology, School of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan.
5. Department of Urology, College of Medicine, and Shu-Tien Urological Science Research Center, National Yang Ming Chiao Tung University, Taipei, Taiwan.
6. Department of Urology, Shuang Ho Hospital, Taipei Medical University, Taipei, Taiwan.
7. Doctor of medicine, Taipei Medical University, Taipei, Taiwan.
Received 2024-8-22; Accepted 2024-11-1; Published 2025-1-1
Abstract
Introduction: Diabetes mellitus (DM) is associated with worse surgical outcomes, and is a risk factor for bladder cancer and subsequent oncological outcomes. This study evaluated outcomes robot-assisted radical cystectomy (RARC) compared to open radical cystectomy (ORC) in patients with DM.
Materials and Methods: Data of adults ≥ 18 years old with DM who underwent radical cystectomy were extracted from the United States National Inpatient Sample database 2005-2018. The outcomes were in-hospital mortality, prolonged length of stay (LOS), and postoperative complications.
Results: Data of 2,765 patients were analyzed. Patients who received RARC had a significantly lower odds of prolonged LOS (adjusted odd ratio (aOR) = 0.56, 95% CI: 0.45, 0.71), unfavorable discharge (aOR = 0.74, 95% CI: 0.56, 0.97), urinary complications (aOR = 0.75, 95% CI: 0.57, 0.98) and wound and device-related complications (aOR = 0.59, 95% CI: 0.41, 0.86) than ORC. Of patients < 70 years old, RARC was significantly associated with decreased odds for urinary complications (aOR = 0.59, 95% CI: 0.41, 0.84) and wound and device-related complications (aOR = 0.55, 95% CI: 0.32, 0.94) compared to ORC. In patients with a Charlson Comorbidity Index score of 0-1, RARC was associated with a lower risk of urinary complications (aOR = 0.74, 95% CI: 0.56, 0.98) and wound and device-related complications (aOR = 0.63, 95% CI: 0.43, 0.93) compared to ORC.
Conclusions: In patients with DM and bladder cancer, RARC appears to be associated with better short-term outcomes in terms of reduced risks of prolonged LOS, unfavorable discharge, urinary complications, and wound and device-related complications compared to ORC.
Keywords: bladder cancer, diabetes mellitus (DM), laparoscopic, nationwide inpatient sample (NIS), open radical cystectomy (ORC), robot-assisted radical cystectomy (RARC)
Introduction
Bladder cancer is the most common malignancy of the urinary tract [1]. In 2020, according to the Global Cancer Statistics Report approximately 575,000 individuals worldwide were diagnosed with bladder cancer, comprising 3% of all malignancies [2]. Radical cystectomy, which can be done through open surgery or minimal invasive surgery, is the standard surgical treatment for non-metastatic muscle-invasive bladder cancer [3]. It has been recognized that minimal invasive surgery is associated with lower risk of various short-term complications and mortality than open radical cystectomy (ORC) for bladder cancer [4].
Diabetes mellitus (DM) is a serious, long-term condition with a major impact on the lives and well-being of individuals, families, and societies worldwide [5]. It is also a rising epidemic, and one of the leading causes of death worldwide [6]. Patients DM may represent a unique population within the context of various health conditions, including greater risks for cardiovascular disease and a variety of cancers [7, 8]. It has been documented that DM is associated with an increased risk for bladder cancer [9, 10]. Further, previous studies have shown that DM is linked to worse survival rates across various cancers, including bladder cancer [11, 12]. Moreover, DM is considered a comorbidity in patients undergoing surgery, and can complicate surgical procedures and have negative impact on postoperative outcomes [13].
Many studies have investigated and compared the effectiveness between robot-assisted radical cystectomy (RARC) and ORC for bladder cancer with respect to oncological and functional outcomes [4, 14-16]. However, there has been limited research has focused specifically on patients with DM. Considering the significance of comprehending the surgical results among high-risk patients such as those with DM to facilitate clinical decision-making and enhance patient care, our study aims to assess the in-hospital outcomes following RARC as compared to ORC. To accomplish this, we utilized a nationally representative cohort from the United States (US).
Methods
Data source
This population-based, retrospective observational study extracted data from the United Stated (US) National Inpatient Sample (NIS) database. The NIS is the largest all-payer, continuous inpatient care database in the United States, and includes about 8 million hospital stays each year [17]. The database is administered by the Healthcare Cost and Utilization Project (HCUP) of the US National Institutes of Health (NIH). The patient data consist of primary and secondary diagnoses, primary and secondary procedures, admission and discharge status, patient demographic information, projected payment source, hospital stay duration, and hospital characteristics (i.e., bed size/location/teaching status/hospital area).
Initial consideration is given to all hospitalized patients for inclusion. The continuously updated, annual NIS database contains patient information from around 1,050 hospitals in 44 states, representing a stratified sample of 20% of US community hospitals, as defined by the American Hospital Association.
Study population
Hospitalized adults ≥ 18 years old with DM who underwent radical cystectomy between 2005 and 2018 were identified through the International Classification of Diseases, Ninth Revision and Tenth Revision, Clinical Modification (ICD-9-CM and ICD-10-CM) codes. Exclusion criteria were patients with incomplete data on main outcomes of interest, sex, and weight values of the dataset. Patients who underwent pure laparoscopic (i.e., without robot assistance) procedures alone were also excluded. Patients who received RARC and ORC were also identified through ICD-9 and ICD-10 procedure codes.
Study outcomes
Outcomes were in-hospital mortality, prolonged length of hospital stay (LOS), postoperative complications, and unfavorable discharge (defined as discharge to a long-term care facility). In-hospital mortality information was identified from the discharge disposition. LOS of stay was calculated by subtracting the admission date from the discharge date. Postoperative complications included infection, urinary complications, acute kidney injury (AKI), and wound and device-related complication (i.e., complications or acute reaction that occur as a result of using surgical instruments or medical devices during procedures), and were identified through ICD codes.
Covariates
Demographic data including age, sex, race, and family income-to-poverty ratio were extracted from the NIS database. Hospital-related characteristics (bed size and location/teaching status) were extracted from the database as part of the comprehensive data available for all participants, in accordance with other NIS studies in the medical literature.
Statistical analysis
Since the NIS database covers a 20% sample of the annual US inpatient admissions, weighted samples (TRENDWT before 2011; DISCWT after 2012), stratum (NIS_STRATUM), and clusters (HOSPID) were used to generate national estimates for all the analyses. SAS software provides an analysis of sample survey data using the SURVEY procedure. Descriptive statistics of the included patients were presented as number (n) and weighted percentage (%), or mean and standard error (SE). Categorical data were analyzed by the PROC SURVEYFREQ method, and continuous data were analyzed by the PROC SURVEYREG method.
The patients included in the study were matched by age and sex using the propensity score matching (PSM) method, to reach a ratio of cases:controls = 1:4. Logistic regression analyses were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for dichotomized outcomes. Variables with significant differences between the 2 comparison groups were entered into multivariable regression models for adjustments. All analyses were 2-sided, and a value of p < 0.05 was considered to indicate a statistically significant difference. All statistical analyses were performed using the statistical software package SAS version 9.4 (SAS Institute Inc., Cary, NC, US).
Results
Study population
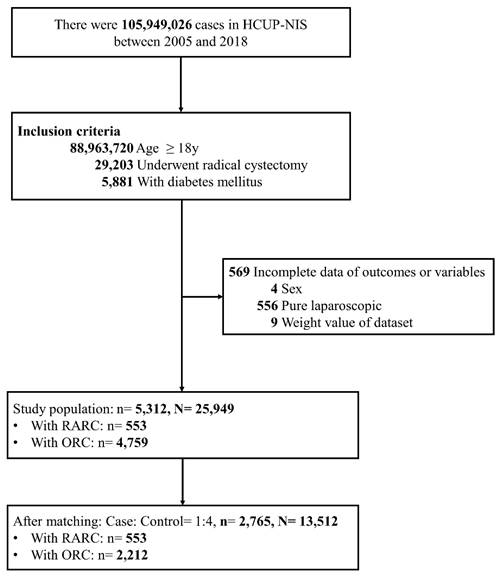
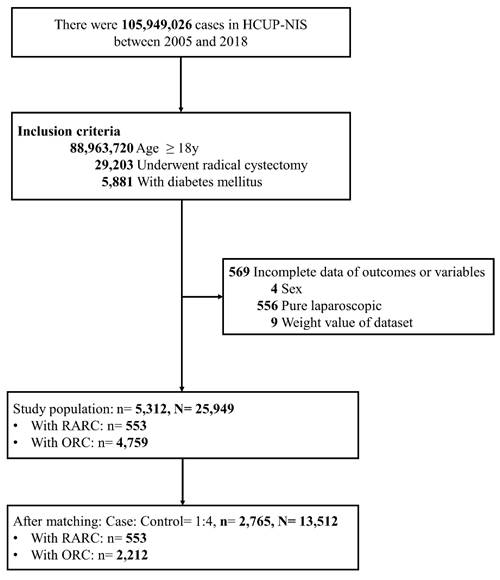
A flow diagram of patient selection and inclusion is shown in Figure 1. A total of 5,881 patients with DM who received a radical cystectomy between 2005 and 2018 were identified in the NIS database. Patients who received a pure laparoscopic radical cystectomy laparoscopic (n = 556) and those with missing information on study outcomes or variables (n = 13) were excluded. Finally, 5,312 patients were included as the study cohort. After PSM, 2,765 patients remained and were included in the analysis. This sample represented 13,512 US adults. Amongst, 553 (20.0%) patients underwent RARC and 2,212 (80.0%) underwent ORC.
Characteristics of the study population after matching
Patient characteristics are summarized in Table 1. The mean age of the patients was 69 years, and 86% were males. Household income, lymph node invasion or metastatic disease, smoking, emergency admission, weekend admission, hospital bed size, and hospital location/ teaching status were significantly different between the 2 groups (all, p < 0.05).
In-hospital outcomes after matching
In-hospital outcomes are summarized in Table 2. Patients who received RARC had lower percentages of urinary, wound, and device-related complications, prolonged LOS, and unfavorable discharge than patients who received ORC (all, p < 0.05).
Flow diagram of patient selection and inclusion.
Associations between RARC and ORC and in-hospital outcomes
The relations between RACR and ORC and in-hospital outcomes are summarized in Table 3. After adjustment, patients who received RARC had a significantly lower risk of prolonged LOS (adjusted odd ratio (aOR) = 0.56, 95% CI: 0.45, 0.71), unfavorable discharge (aOR = 0.74, 95% CI: 0.56, 0.97), urinary complications (aOR = 0.75, 95% CI: 0.57, 0.98) and wound and device-related complications (aOR = 0.59, 95% CI: 0.41, 0.86) than patients who received ORC. Full analytic models are shown in Supplementary Tables S3-S4.
Characteristics of the study population after matching
| Total (N = 2,765) | RARC (n = 553) | ORC (n = 2,212) | p-value | |
|---|---|---|---|---|
| Age, years | 69.4 ± 0.2 | 69.5 ± 0.3 | 69.4 ± 0.2 | 0.853 |
| 18-59 | 335 (12.1) | 67 (12.2) | 268 (12.1) | 0.999 |
| 60-69 | 1040 (37.6) | 208 (37.4) | 832 (37.7) | |
| 70-79 | 1060 (38.4) | 212 (38.4) | 848 (38.4) | |
| 80+ | 330 (11.9) | 66 (12.0) | 264 (11.9) | |
| Sex | 0.984 | |||
| Male | 2385 (86.3) | 477 (86.3) | 1908 (86.3) | |
| Female | 380 (13.7) | 76 (13.7) | 304 (13.7) | |
| Insurance status | 0.193 | |||
| Medicare/Medicaid | 1986 (71.9) | 382 (69.3) | 1604 (72.6) | |
| Private including HMO | 704 (25.5) | 152 (27.5) | 552 (25.0) | |
| Self-pay/no-charge/other | 71 (2.6) | 18 (3.2) | 53 (2.4) | |
| Missing | 4 | 1 | 3 | |
| Household income | 0.032 | |||
| Q1 | 639 (23.5) | 113 (21.0) | 526 (24.2) | |
| Q2 | 701 (25.8) | 125 (23.0) | 576 (26.5) | |
| Q3 | 739 (27.2) | 163 (30.3) | 576 (26.5) | |
| Q4 | 635 (23.5) | 140 (25.8) | 495 (22.9) | |
| Missing | 51 | 12 | 39 | |
| Lymph node invasion or metastatic disease | 0.036 | |||
| Yes | 592 (21.3) | 100 (18.0) | 492 (22.2) | |
| No | 2173 (78.7) | 453 (82.0) | 1720 (77.8) | |
| Smoking | <0.001 | |||
| Yes | 1167 (42.4) | 272 (49.3) | 895 (40.6) | |
| No | 1598 (57.6) | 281 (50.7) | 1317 (59.4) | |
| DM with end organ damage | 0.485 | |||
| Yes | 352 (12.8) | 66 (11.9) | 286 (13.0) | |
| No | 2413 (87.2) | 487 (88.1) | 1926 (87.0) | |
| CCI | 0.785 | |||
| 0-1 | 1965 (71.0) | 389 (70.4) | 1576 (71.1) | |
| 2-3 | 686 (24.8) | 144 (26.0) | 542 (24.5) | |
| 4-5 | 104 (3.8) | 18 (3.3) | 86 (4.0) | |
| 6+ | 10 (0.4) | 2 (0.4) | 8 (0.4) | |
| Emergent admission | <0.001 | |||
| Yes | 277 (10.0) | 23 (4.2) | 254 (11.5) | |
| No | 2482 (90.0) | 530 (95.8) | 1952 (88.5) | |
| Missing | 6 | 0 | 6 | |
| Weekend admission | 0.025 | |||
| Yes | 140 (5.0) | 17 (3.1) | 123 (5.5) | |
| No | 2625 (95.0) | 536 (96.9) | 2089 (94.5) | |
| Hospital bed size | <0.001 | |||
| Small | 301 (10.6) | 98 (17.6) | 203 (8.9) | |
| Medium | 498 (18.3) | 78 (14.3) | 420 (19.3) | |
| Large | 1956 (71.1) | 376 (68.0) | 1580 (71.8) | |
| Missing | 10 | 1 | 9 | |
| Hospital location/ teaching status | <0.001 | |||
| Rural | 50 (1.7) | 3 (0.5) | 47 (2.1) | |
| Urban nonteaching | 444 (16.1) | 54 (9.9) | 390 (17.6) | |
| Urban teaching | 2261 (82.2) | 495 (89.6) | 1766 (80.3) | |
| Missing | 10 | 1 | 9 |
Abbreviation: HMO, Health Maintenance Organization; RARC, robotic-assisted radical cystectomy; ORC, open radical cystectomy; DM, diabetes mellitus; and CCI, Charlson Comorbidity Index; Q, quartile.
Continuous variables are presented as mean ± SE; categorical variables are presented as unweighted counts (weighted percentage).
p-value < 0.05 shown in bold.
In-hospital outcomes after matching
| Total (N = 2,765) | RARC (n = 553) | ORC (n = 2,212) | p-value | |
|---|---|---|---|---|
| In-hospital mortality | 46 (1.6) | 11 (2.0) | 35 (1.6) | 0.459 |
| Complication, any | 1673 (60.5) | 312 (56.2) | 1361 (61.6) | 0.017 |
| AMI and cardiac complications | 201 (7.3) | 38 (6.8) | 163 (7.4) | 0.647 |
| CVA and nervous system complications | 65 (2.4) | 12 (2.2) | 53 (2.4) | 0.721 |
| VTE | 94 (3.4) | 13 (2.3) | 81 (3.7) | 0.105 |
| Respiratory complications and pneumonia | 370 (13.4) | 68 (12.3) | 302 (13.7) | 0.381 |
| Digestive system complications | 531 (19.3) | 95 (17.1) | 436 (19.9) | 0.155 |
| Urinary complications | 409 (14.8) | 62 (11.3) | 347 (15.7) | 0.005 |
| Vascular complication | 28 (1.0) | 4 (0.7) | 24 (1.1) | 0.360 |
| Bleeding/transfusion | 587 (21.2) | 109 (19.6) | 478 (21.5) | 0.336 |
| Infection | 364 (13.2) | 74 (13.3) | 290 (13.2) | 0.901 |
| Sepsis/shock | 292 (10.6) | 57 (10.3) | 235 (10.7) | 0.787 |
| Tracheostomy/mechanical ventilation | 121 (4.3) | 27 (4.8) | 94 (4.2) | 0.488 |
| AKI | 541 (19.7) | 108 (19.6) | 433 (19.7) | 0.965 |
| Wound and device-related complication | 227 (8.2) | 30 (5.4) | 197 (8.9) | 0.003 |
| Prolonged LOS a, b | 780 (28.1) | 103 (18.5) | 677 (30.6) | <0.001 |
| Unfavorable discharge a | 490 (18.0) | 76 (14.1) | 414 (19.0) | 0.008 |
Abbreviation: RARC, robotic-assisted radical cystectomy; ORC, open radical cystectomy; AMI, acute myocardial infarction; CVA, cerebrovascular accident; VTE, venous thromboembolism; AKI, acute kidney injury; LOS, length of stay in hospital.
Continuous variables are presented as mean ± SE; categorical variables are presented as unweighted counts (weighted percentage).
a Excluding patients who died in the hospital.
b LOS > 11 days.
p-value < 0.05 shown in bold.
Associations between RARC vs. ORC and in-hospital outcomes
| Outcomes | Surgery | Univariable | Multivariable | ||
|---|---|---|---|---|---|
| OR (95% CI) | P-value | aOR (95% CI) | P-value | ||
| In-hospital mortality c | RARC vs ORC | 1.25 (0.69, 2.28) | 0.460 | 1.48 (0.81, 2.69) | 0.203 |
| Prolonged LOS a, b, d | RARC vs ORC | 0.51 (0.41, 0.63) | <0.001 | 0.56 (0.45, 0.71) | <0.001 |
| Unfavorable discharge a, d | RARC vs ORC | 0.70 (0.54, 0.91) | 0.008 | 0.74 (0.56, 0.97) | 0.028 |
| Complication, any d | RARC vs ORC | 0.80 (0.67, 0.96) | 0.017 | 0.83 (0.69, 1.01) | 0.057 |
| Infection d | RARC vs ORC | 1.02 (0.78, 1.33) | 0.900 | 1.08 (0.83, 1.42) | 0.568 |
| Urinary complications d | RARC vs ORC | 0.68 (0.52, 0.89) | 0.005 | 0.75 (0.57, 0.98) | 0.037 |
| AKI d | RARC vs ORC | 1.00 (0.80, 1.25) | 0.965 | 1.04 (0.82, 1.31) | 0.764 |
| Wound and device-related complication d | RARC vs ORC | 0.58 (0.40, 0.84) | 0.004 | 0.59 (0.41, 0.86) | 0.006 |
Abbreviation: LOS, length of stay in hospital; AKI, acute kidney injury; OR, odd ratio; aOR, adjusted odd ratio; CI, confidence interval; CCI, Charlson Comorbidity Index.
P-value < 0.05 is shown in bold.
a Excluding patients who died in the hospital.
b LOS > 8 days.
c Adjusted for age group, smoking, CCI, and emergency admission.
d Adjusted for age group, sex, insurance status, smoking, diabetes mellitus with end-organ damage, CCI, emergency admission, and weekend admission.
Associations between RARC and ORC and in-hospital outcomes, stratified by age and Charlson Comorbidity Index (CCI)
The relations between RARC and ORC and in-hospital outcomes stratified by age and CCI are shown in Table 4. After adjustment, patients < 70 years old who received RARC were significantly less likely to have urinary complications (aOR = 0.59, 95% CI: 0.41, 0.84) and wound and device-related complications (aOR = 0.55, 95% CI: 0.32, 0.94) compared to those who received ORC. In patients with a CCI of 0-1, those that received RARC were significantly less likely to have urinary complications (aOR = 0.74, 95% CI: 0.56, 0.98) and wound and device-related complications (aOR = 0.63, 95% CI: 0.43, 0.93) compared to those that received ORC.
Discussion
The present study used a nationally representative sample of the US to compare the outcomes of RARC and ORC in patients with bladder cancer and DM. The results showed that RARC is independently associated with a lower risk of prolonged LOS, unfavorable discharge, urinary complications, and wound and device-related complication than ORC.
Associations between RARC vs. ORC and in-hospital outcomes, stratified by age and CCI
| Subgroup | Surgery | Infection | Urinary complications | AKI | Wound and device-related complication | ||||
|---|---|---|---|---|---|---|---|---|---|
| aOR (95% CI) | P-value | aOR (95% CI) | P-value | aOR (95% CI) | P-value | aOR (95% CI) | P-value | ||
| Age group | |||||||||
| < 70 | RARC vs. ORC | 1.11 (0.77, 1.60) | 0.575 | 0.59 (0.41, 0.84) | 0.003 | 1.00 (0.73, 1.37) | 0.989 | 0.55 (0.32, 0.94) | 0.029 |
| 70+ | RARC vs. ORC | 1.04 (0.72, 1.50) | 0.821 | 0.94 (0.66, 1.36) | 0.751 | 1.08 (0.79, 1.47) | 0.641 | 0.63 (0.39, 1.03) | 0.064 |
| CCI | |||||||||
| 0-1 | RARC vs. ORC | 1.10 (0.84, 1.45) | 0.492 | 0.74 (0.56, 0.98) | 0.034 | 1.06 (0.84, 1.34) | 0.633 | 0.63 (0.43, 0.93) | 0.018 |
| 2+ | RARC vs. ORC | 0.54 (0.18, 1.60) | 0.243 | 0.66 (0.21, 2.12) | 0.470 | 0.73 (0.32, 1.67) | 0.432 | NA | |
Abbreviation: AKI, acute kidney injury; RARC, robotic-assisted radical cystectomy; ORC, open radical cystectomy; CCI, Charlson Comorbidity Index; aOR, adjusted odd ratio; CI, confidence interval; NA, not applicable.
P-value < 0.05 is shown in bold.
The benefits of RARC are more prominent among patients < 70 years old and with a CCI score of 0-1 than in older patients. These results add further information to the literature which support the advantages of RARC over ORC, and specifically the advantages are seen in patients with DM.
DM has become a world-wide health concern, with a prevalence that is increasing yearly, in association with the obesity epidemic [2, 6, 9]. The incidence of bladder cancer is also increasing [1, 2]. Though some studies have found that type 2 DM is not associated with an increased risk of bladder cancer [9], many studies have shown that patients with DM have a higher risk of developing cancer in general, and specifically bladder cancer [10, 18]. Notably, systematic reviews and meta-analyses have suggested that DM is associated with a poorer prognosis in patients with bladder cancer who undergo surgery (recurrence rate, cancer-specific survival) [19, 20]. The negative impact of diabetes on bladder cancer outcomes, especially following surgeries like radical cystectomy, may be attributed to several mechanisms, including heightened inflammation and an increased susceptibility to infections [19, 20]. As such, it is important to understand how the type of surgery and other factors influences the outcomes of patients with DM and bladder cancer who require surgery.
Radical cystectomy is the procedure of choice for patients with bladder cancer, and is a difficult procedure that can be associated with complications and marked morbidity. RARC simplifies the procedure and provides an improved surgical field compared to an open procedure [21]. However, the learning curve is steep, and as a relatively new technology, it is important to determine how outcomes of RARC compare to that of the gold standard, ORC. A number of randomized controlled trials (RCTs) have compared RARC and ORC with respect to different outcomes, and the trials have indicated that RARC provides similar or better clinical and oncological outcomes as ORC [4, 14, 15].
In recent years, a number of literature reviews, and systematic reviews and meta-analyses have been published examining various outcomes of RARC compared to ORC. For example, a review of the literature by Iqbal et al. [22]. published in 2021 suggested that functional outcomes are similar between RARC and ORC. In 2023, 2 systematic reviews and meta-analyses of randomized controlled trials compared RARC and ORC. Fontanet et al. [23]. included 8 RCTs comprised of 1,024 patients and found that RARC is not inferior to ORC in terms of surgical safety and oncological outcomes, and RARC was associated with a lower blood transfusion rate. Liu et al. [24]. also examined RCTs and reported that oncological outcomes, postoperative complications, and health-related quality of life were similar between the 2 procedures. An analysis of RCTs by Khetrapal et al. [25]. found similar oncological outcomes between the 2 procedures, and that RARC was associated with less blood loss and a shorter hospital stay. An analysis by Kimura et al. [26]. that included 6 RCTs and 31 non-randomized comparative studies no differences in quality of life score assessment, complications, length of hospital stay and mortality between the 2 procedures. In a unique study, Aminoltejari et al. [27]. examined the data from current systematic reviews and meta-analyses. The analysis found that oncological outcomes and complications were similar between the 2 procedures, but quality of life outcomes required further study.
In contrast to previous literature that did not specifically address DM patients, our results indicate that the advantages of RARC appear to be even more pronounced in individuals with DM. Yuanming et al. [28]. conducted a comprehensive analysis of risk factors for adverse perioperative outcomes in patients undergoing RARC. Notably, DM emerged as an independent risk factor associated with prolonged LOS. It is known that, DM patients, who contend with compromised immune responses and complex medical conditions, exhibit a heightened vulnerability to postoperative complications across various surgical settings [18]. As mentioned previously, RARC, characterized by its minimally invasive approach, which entails smaller incisions, equips surgeons with enhanced precision and dexterity. This technique mitigates tissue trauma, reduces blood loss, and expedites the recovery process. For DM patients, these advantages contribute to improved wound healing, consequently positively impacting both wound complication rates and need for prolonged hospitalization. Therefore, it could provide larger benefit than in those without DM.
Finally, our investigations within the DM subgroup consistently demonstrated the superiority of RARC over ORC in several short-term outcomes. This held true even after rigorous control for various clinical factors, emphasizing the critical role of RARC in improving outcomes within this patient subgroup. Notably, our findings indicate that younger individuals (<70y), and those with lower comorbidity burdens, might gain even more substantial advantages from RARC in terms of short-term outcomes. This highlights that even in the population where surgery can be tolerated, RARC still emerges as a more favorable procedure.
Strength and Limitations
The strength of the study is the analysis based on a very large, nationally representative sample. The results are likely generalizable to the entire population of the US. However, this study also has several limitations. First, due to the retrospective and observational design of the study, it's important to interpret the findings cautiously, recognizing the potential for selection bias. Second, errors in coding are possible, much like in prior claim-based studies that use the ICD code system. Third, the exact T stage was not recorded in the dataset, precluding our analysis. Also, the duration and treatment modality for DM was not available in the database. Additionally, the NIS database does not contain data on long-term follow-up, readmission rates, or survival after discharge, making it impossible to conduct an analysis. Lastly, although important, preoperative performance status and intraoperative characteristics such as type of urinary diversion, duration of the procedure, and amount of blood lost, were not taken into account in the analysis due to lack of data.
Conclusions
In patients with DM and bladder cancer opting for surgery, compared to ORC, RARC appears to be associated with better short-term outcomes in terms of reduced risks for prolonged LOS, unfavorable discharge, urinary complication, as well as wound and device-related complications. Prospective studies are still warranted to further validate these findings.
Supplementary Material
Supplementary tables.
Acknowledgements
Author contributions
Conception and design, Acquisition of data, Analysis and interpretation of data, Critical revision of the manuscript and statistical analysis were performed by CH Chung, I-Shen Huang, Wei-Tang Kao; Drafting of the manuscript, literature research, clinical studies, experimental studies, Obtaining funding, Administrative, technical or material support were performed by CH Chung, Wei-Tang Kao; Final approval of the manuscript, guarantor of integrity of the entire study, definition of intellectual content, Supervision were performed by Wei-Tang Kao. All authors read and approved the final manuscript.
Ethics statement
This study complies with the terms of the NIS data-use agreement. Given that this study solely involved the analysis of secondary data, there was no direct involvement of the general public or patients. It was granted exemption from requiring IRB approval.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Dobruch J, Oszczudłowski M. Bladder Cancer: Current Challenges and Future Directions. Medicina (Kaunas). 2021;57(8):749
2. Sung H, Ferlay J, Siegel RL. et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-49
3. Aminoltejari K, Black PC. Radical cystectomy: a review of techniques, developments and controversies. Transl Androl Urol. 2020;9(6):3073-81
4. Catto JWF, Khetrapal P, Ricciardi F. et al. Effect of Robot-Assisted Radical Cystectomy With Intracorporeal Urinary Diversion vs Open Radical Cystectomy on 90-Day Morbidity and Mortality Among Patients With Bladder Cancer: A Randomized Clinical Trial. Jama. 2022;327(21):2092-103
5. Gopisetty D, Levine B, Liu N. et al. How Does Diabetes Affect Daily Life? A Beyond-A1C Perspective on Unmet Needs. Clin Diabetes. 2018;36(2):133-7
6. Saeedi P, Petersohn I, Salpea P. et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843
7. Glovaci D, Fan W, Wong ND. Epidemiology of Diabetes Mellitus and Cardiovascular Disease. Curr Cardiol Rep. 2019;21(4):21
8. Pearson-Stuttard J, Papadimitriou N, Markozannes G. et al. Type 2 Diabetes and Cancer: An Umbrella Review of Observational and Mendelian Randomization Studies. Cancer Epidemiol Biomarkers Prev. 2021;30(6):1218-28
9. Pan Y, Lee CY, Lee LM. et al. Incidence of Bladder Cancer in Type 2 Diabetes Mellitus Patients: A Population-Based Cohort Study. Medicina (Kaunas). 2020;56(9):441
10. Choi YH, Park YM, Hur KJ. et al. Duration of diabetes mellitus and risk of kidney and bladder cancer: a longitudinal nationwide cohort study. Am J Cancer Res. 2022;12(8):4050-61
11. Tuderti G, Chiacchio G, Mastroianni R. et al. Impact of diabetes mellitus on oncologic outcomes in patients receiving robot-assisted radical cystectomy for bladder cancer. World J Urol. 2024;42(1):479
12. Xu Y, Huo R, Chen X. et al. Diabetes mellitus and the risk of bladder cancer: A PRISMA-compliant meta-analysis of cohort studies. Medicine (Baltimore). 2017;96(46):e8588
13. Drayton DJ, Birch RJ, D'Souza-Ferrer C. et al. Diabetes mellitus and perioperative outcomes: a scoping review of the literature. Br J Anaesth. 2022;128(5):817-28
14. Parekh DJ, Reis IM, Castle EP. et al. Robot-assisted radical cystectomy versus open radical cystectomy in patients with bladder cancer (RAZOR): an open-label, randomised, phase 3, non-inferiority trial. Lancet. 2018;391(10139):2525-36
15. Bochner BH, Dalbagni G, Marzouk KH. et al. Randomized Trial Comparing Open Radical Cystectomy and Robot-assisted Laparoscopic Radical Cystectomy: Oncologic Outcomes. Eur Urol. 2018;74(4):465-71
16. Mastroianni R, Tuderti G, Ferriero M. et al. Robot-assisted Radical Cystectomy with Totally Intracorporeal Urinary Diversion Versus Open Radical Cystectomy: 3-Year Outcomes from a Randomised Controlled Trial. Eur Urol. 2024;85(5):422-30
17. HCUP Databases [updated June 2024. Healthcare Cost and Utilization Project (HCUP) and Agency for Healthcare Research and Quality]. Available from: https://hcup-us.ahrq.gov/nisoverview.jsp.
18. Zhang X, Hou A, Cao J. et al. Association of Diabetes Mellitus With Postoperative Complications and Mortality After Non-Cardiac Surgery: A Meta-Analysis and Systematic Review. Front Endocrinol (Lausanne). 2022;13:841256
19. Lu Y, Tao J. Diabetes Mellitus and Obesity as Risk Factors for Bladder Cancer Prognosis: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2021;12:699732
20. Dong L, Ying X, Tao S. et al. Diabetes Is a Risk Factor for the Prognosis of Patients with Bladder Cancer: A Meta-Analysis. J Oncol. 2022;2022:1997507
21. Han JH, Ku JH. Robot-assisted radical cystectomy: Where we are in 2023. Investig Clin Urol. 2023;64(2):107-17
22. Iqbal U, Durrani MM, Elsayed AS. et al. Functional outcomes after robot-assisted radical cystectomy: A review of literature. Int J Urol. 2021;28(5):493-501
23. Fontanet S, Basile G, Baboudjian M. et al. Robot-assisted vs. open radical cystectomy: systematic review and meta-analysis of randomized controlled trials. Actas Urol Esp (Engl Ed). 2023;47(5):261-70
24. Liu H, Zhou Z, Yao H. et al. Robot-assisted radical cystectomy vs open radical cystectomy in patients with bladder cancer: a systematic review and meta-analysis of randomized controlled trials. World Journal of Surgical Oncology. 2023;21(1):240
25. Khetrapal P, Wong JKL, Tan WP. et al. Robot-assisted Radical Cystectomy Versus Open Radical Cystectomy: A Systematic Review and Meta-analysis of Perioperative, Oncological, and Quality of Life Outcomes Using Randomized Controlled Trials. Eur Urol. 2023;84(4):393-405
26. Kimura S, Iwata T, Foerster B. et al. Comparison of perioperative complications and health-related quality of life between robot-assisted and open radical cystectomy: A systematic review and meta-analysis. Int J Urol. 2019;26(8):760-74
27. Aminoltejari K, Hird AE, Klaassen Z. et al. Robotic Versus Open Cystectomy for Bladder Cancer: Synthesizing the Data from Current Systematic Reviews and Meta-Analyses. Ann Surg Oncol. 2023;30(5):2976-87
28. Lee AY, Allen JC Jr, Teoh JY. et al. Predicting perioperative outcomes of robot-assisted radical cystectomy: Data from the Asian Robot-Assisted Radical Cystectomy Consortium. Int J Urol. 2022;29(9):1002-9
Author contact
![]() Corresponding author: Wei-Tang Kao, MD, PhD, Department of Urology, Shuang Ho Hospital, Taipei Medical University; Address: No. 291, Zhongzheng Rd., Zhonghe District, New Taipei City, 23561, Taiwan (R.O.C.); Tel.: +886 2-22490088; Email: kaovgh2008com.
Corresponding author: Wei-Tang Kao, MD, PhD, Department of Urology, Shuang Ho Hospital, Taipei Medical University; Address: No. 291, Zhongzheng Rd., Zhonghe District, New Taipei City, 23561, Taiwan (R.O.C.); Tel.: +886 2-22490088; Email: kaovgh2008com.

 Global reach, higher impact
Global reach, higher impact