3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2025; 22(1):170-178. doi:10.7150/ijms.96981 This issue Cite
Research Paper
Analysis of User-Generated Posts on Social Media of Adjuvant Analgesics: A Machine Learning Study
1. Department of Medicine and Medical Specialities. University of Alcala, Alcala de Henares, 28801 Madrid, Spain.
2. Ramón y Cajal Institute of Sanitary Research (IRYCIS), 28034 Madrid, Spain.
3. ISGlobal, Barcelona, Spain.
4. CIBER Epidemiología y Salud Pública (CIBERESP), Madrid, Spain.
5. Cardiovascular and Nutritional Epidemiology, Unit of Institute of Environmental Medicine, Karolinska In-stitute, Stockholm, Sweden.
6. Departamento Teoria de la Señal y Comunicaciones y Sistemas Telemáticos y Computación, Escuela Tecnica Superior de Ingenieria de Telecomunicación, Universidad Rey Juan Carlos, 28942 Fuenlabrada, Spain.
7. Department of Psychiatry and CTS-549 Research Group, Institute of Neurosciences, University of Granada, Granada, Spain.
8. Department of Psychiatry, San Cecilio University Hospital, Granada, Spain.
9. Centro de Investigación Biomédica en Red Fisiopatología de la Obesidad y la Nutrición (CIBEROBN), Insti-tute of Health Carlos III, Madrid, Spain.
10. Department of Preventive Medicine and Public Health, Instituto de Investigación Sanitaria de Navarra (IdiSNA), University of Navarra, Pamplona, Spain.
11. Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA, USA.
12. Department of Psychiatry and Mental Health. Hospital Universitario Infanta Leonor, Madrid, Spain.
13. CIBERSAM-ISCIII (Biomedical Research Networking Centre in Mental Health), Madrid, Spain.
Received 2024-4-4; Accepted 2024-10-21; Published 2025-1-1
Abstract
Background: Antiepileptics and antidepressants are frequently prescribed for chronic pain, but their efficacy and potential adverse effects raise concerns, including dependency issues. Increased prescriptions, sometimes fraudulent, prompted reclassification of antiepileptics in some countries. Our aim is to comprehend opinions, perceptions, beliefs, and attitudes towards co-analgesics from online discussions on X (formerly known as Twitter), offering insights closer to reality than conventional surveys.
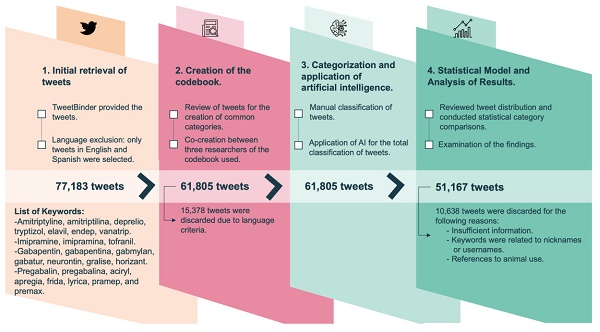
Methods: In this cross-sectional study, we collected 77,183 public posts about co-analgesics in English or Spanish from January 1st 2019 to December 31st, 2020. A total of 51,167 post were included, and 2,000 were manually analyzed using a researcher-created codebook. Machine learning classifiers were then applied to the remaining datasets to determine the number of publications for each user type and identify categories through content analysis.
Results: Of the 51,167 posts analyzed, 78% discussed anticonvulsants and 24% discussed analgesic antidepressants (Percentages add up to more than 100% because there were 1,300 posts containing references to both types of medications). Only 13% were authored by healthcare professionals, while 67% were from patients. Medical content predominated, with 70% noting low medication efficacy and almost 50% referencing side effects. Non-medical content included challenges in dispensing (25%), complaints about high costs (15%), and trivialization of medication use (10%).
Conclusions: This study offers valuable insights into public perceptions of co-analgesics. Findings aid in designing public health communications to raise awareness of associated risks, urging both healthcare providers and the public to optimize drug use.
Keywords: Machine Learning, Pain, Coanalgesics, X social media, Twitter
Introduction
Chronic pain is a common reason for seeking medical attention and often requires a multifactorial approach to management. Opioids are the cornerstone of pain treatment but have serious long term side effects [1,2]. Their misuse has created a huge public health problem in many countries, particularly in the United States, with a heavy death toll [3]. The inappropriate use of this medication is also associated with increased rates of anxiety and depressive disorders [3].
Therefore, it is common to use adjunctive medications such as pregabalin, gabapentin, and tricyclic antidepressants. In fact, there has been an increasing use and prescription of these adjunctive medications [4,5]. Studies have shown a rise in amitriptyline prescriptions for purposes other than depression [6], with antidepressants being the most commonly used for off-label indications [7]. Amitriptyline was the third most prescribed antidepressant in Germany in 2008 and the second most prescribed antidepressant in England between 2015 and 2019 [8-10]. In Canada, almost half (48.4%) of amitriptyline prescriptions are for pain relief [11]. The use of gabapentinoids in the United States has more than tripled between 2002 and 2015, with a 50% increase in prescriptions between 2012 and 2016 [12], and the number of prescriptions continues to rise in the USA [13]. In the United Kingdom, the use of pregabalin increased by 350% between 2008 and 2013, and the rate of patients newly treated with gabapentinoids tripled from 2007 to 2017 in primary care [14], and nowadays the figures seem to be stabilizing [15,16].
However, caution must be exercised when using these adjunctive medications, as they have multiple pharmacological interactions and are often used in combination with other drugs [17,18]. They are also associated with relatively common side effects such as dizziness, drowsiness, difficulties in memory or concentration, nausea, and vomiting [10,19]. Furthermore, there is an increasing off-label use of these medications, which is concerning [5,20-22]. Tricyclic antidepressants in particular are commonly used in suicide attempts [23].
Moreover, the recreational use of tricyclic antidepressants and anticonvulsants has been well documented, and there has been an alert about the increasing prescriptions [24-26] and misuse, especially of pregabalin [27,28]. While pregabalin is considered a controlled substance by the FDA, indicating potential for abuse, it is widely perceived as having minimal abuse liability by patients [29]. In France, pregabalin has become the most frequently included drug in counterfeit prescription forms submitted to pharmacies, as reported in the 2019 OSIAP survey [30].
On the other hand, there are many patients who are correctly prescribed these adjunctive medications, but due to their negative beliefs about the treatment patients tend to not adhere properly [31,32]. In this context, intentional non-adherence has been described in patients with chronic disease, often attributed to feeling well and deciding not to take the medication due to fear of side effects [33,34]. Therefore, it is important to understand the opinions, perceptions, beliefs, and attitudes that patients, healthcare professionals, and society most frequently maintain towards these medications used in pain treatment. Analyzing spontaneous online discussions, such as those on social media platforms, can provide insights closer to reality than traditional survey methods [35,36]. In fact, this type of analysis is also being used for pharmacovigilance purposes [37-39]. Moreover, con-versations on social media are generated in a more informal and spontaneous environment, making it more likely to reflect people's true beliefs [40-42]. Finally, analyzing these posts allows us to understand the opinions of the general population, including patients who are reluctant to participate in conventional surveys, as well as their family members or acquaintances [43-45].
In this infodemiology study, we utilized the social network X, formerly and more commonly known as Twitter. We aimed to: 1) Quantify the frequency of communications on Twitter about adjunctive medications for pain relief (i.e., co-analgesics) and the interest they generate; 2) Characterize the types of users of co-analgesics participating in these conversations; 3) Identify the main thematic content of the posts related to co-analgesics, with a focus on detecting online sales or other activities that may be detrimental to health.
Materials and Methods
Twitter search and data collection strategy
In this quantitative and qualitative observational study, we focused on searching for posts that referenced co-analgesics. We gathered all publicly available posts utilizing a set of keywords derived from the brand names and generic names of the most commonly prescribed active constituents of pregabalin, gabapentin, amitriptyline, and imipramine in both the United States and Spain. The keywords included were: amitrytiline, amitriptilina, deprelio, tryptizol, elavil, endep, vanatrip, imipramine, Imipramina, tofranil, gabapentin, gabapentina, gabmylan, gabatur, neurontin, gralise, horizant, pregabalin, pregabalina, aciryl, apregia, frida, lyrica, pramep, and premax (Figure 1).
The inclusion criteria for posts were as follows: 1) Published from an open account; 2) Including any of the listed keywords in the post; 3) Posted between January 2019 and December 2020; 4) Written in either Spanish or English. We also collected supplementary data for the posts: the number of retweets and likes generated by each post, as well as the profile description of the users. The tool used for post collection was Tweet Binder, which allows access to 100% of public posts.
Content analysis process
A total of 77,183 posts were collected, of which 15,378 posts were excluded for being written in a language other than English or Spanish (Figure 1). A codebook was created to analyze the posts. The codebook was completed after the discussion and analysis of 300 posts by 3 researchers. In the codebook, the type of user is the first classified domain, followed by distinguishing between medical and non-medical content. Additionally, we identified posts that posed questions. Regarding the type of user, we distinguished between patients, family members and friends, healthcare professionals, or institutions. To determine the type of user, we examined the profile and the content of the post itself.
Flowchart.
Regarding the content, if it was medical in nature, we classified it according to whether it referred to the good or poor efficacy of a drug and whether it mentioned adverse effects. Finally, we classified fake medical content. A paramount consideration was the meticulous specificity of medical content categories. Additionally, in the non-medical content, we distinguished four themes: 1) Management issues; 2) Economic aspects; 3) Solidarity; and 4) Trivialization. Under the category of management issues, we discerned bureaucratic, commercial, and legal content related to pharmacy delivery, medical appointments, commercial aspects, and legal facets. Within the realm of economic considerations, we ascertained whether it pertained to the cost of the pharmaceutical agent.
We grouped the posts by their keywords into 2 categories. The anticonvulsants category contained posts corresponding to pregabalin or gabapentin, and the tricyclics category contained posts corresponding to imipramine and amitriptyline. We selected a total of 1,000 posts for each category, which were manually classified according to the discussed codebook. When the content did not provide sufficient information, when the username matched a keyword, or when the post referred to the use of the drug in animals, it was classified as unclassifiable. Unclassifiable posts were excluded from the study.
Machine-learning classifier
Technological advances in recent years have allowed the development of multiple emerging scientific disciplines, among them artificial intelligence (AI). AI refers to the development of computer systems that can perform tasks typically requiring human intelligence. It involves the creation of algorithms and models that enable machines to learn from data, reason, recognize patterns, and make decisions autonomously [46]. Within AI we can find several branches and one of them is Machine Learning, ML whose objective is to create computational models that extract knowledge from data with a reasonable capacity for generalization. Finally, within ML you can find Deep Learning (DL). DL uses models called neural networks, which are AI methods inspired by human brain neurons whose function is to process information [47]. Neural networks have multiple applications ranging from market prediction [48], through detection of infections [49] or the detection of faces in images [50].
Inside ML we are able to find, another type of differentiation depending on the type data used to train the model: supervised, unsupervised and semi-supervised Learning [51]. In supervised learning, algorithms are trained with labeled data and they learn patterns to make predictions on new data. Unsupervised learning involves training the algorithm on unlabeled data to identifies inherent patterns or clusters. Lastly, semi-supervised learning is a combination of supervised and unsupervised learning and it utilizes a mix of labeled and unlabeled data during training. The model leverages the labeled data to learn from known patterns and utilizes the unlabeled data to generalize and infer patterns across the entire dataset. The goal of semi-supervised learning is to maximize the learning performance of the model through such newly-labeled examples while minimizing the work required of human annotators [52].
For this project, we adopted a Semi-supervised Learning approach using a pretrained neural network called xlm-roberta-base [53]. This network is a multilingual version of RoBERTa pretrained on a large corpus in a self-supervised fashion. This means it was pretrained on the raw texts only, with no humans labelling them. However, semi-supervised learning requires labeled data. Therefore, it was necessary to train the network in a process called fine-tuning. The manually classified posts were normalized by removing special characters such as users and links. The data was then randomly split into two subsets using stratification for each category: 80% of the posts were allocated for training, while the remaining 20% were used for testing. This separation was performed using a seed to ensure replicability. The training subset was used for fine-tuning the network, and the testing subset was used to validate its performance on our dataset. The weighted F1-score was computed in all the categories to check the performance of the models. We executed the random split and the training three times with different seeds to ensure the good performance of the models in different partitions. In all the three iterations the model achieves similar results. In none of the categories the F1-score drops below 75%, so the precision of the models is sufficiently high. Besides, this fine-tuning methodology has shown promising results in previous studies [54]. Finally, we used the fine-tunned network model (trained to apply our classification) to categorize the posts that had not been classified by hand.
Statistical analysis
The study involved analyzing the frequency distribution of posts across various categories based on post characteristics. Percentage of posts or the median of likes and retweets in each category are reported. To compare the proportions of posts between categories, Pearson's chi-square test was utilized, yielding a p-value indicating statistical significance.
The statistical analyses were performed using the software packages STATA v16 (StataCorp).
Ethical considerations
This project received approval from the ethics committee of Hospital Príncipe de Asturias (OE 14_2020). The ethical principles in research outlined in the Declaration of Helsinki (7th revision, 2013) were followed. This study did not directly involve human subjects or include any interventions, but solely utilized publicly available posts. Nevertheless, we have taken care not to disclose any usernames or quote posts that could reveal them, to protect their privacy.
Results
The most prevalent themes are the perceived low efficacy and the side effects reported by patients
Out of the total collected posts, 51,167 were deemed classifiable. Among these, 78% referred to anticonvulsants, and 24% to analgesic antidepressants. There were 1,300 posts in total containing references to both types of medications. Posts about anticonvulsants generated four times more "highly liked" posts and eight times more "highly retweeted" posts compared to analgesic antidepressants. In terms of user type, patients clearly stood out, generating two-thirds of the total posts. Furthermore, posts posted by healthcare professionals, institutions and family/friends received the most likes and retweets. (Table 1).
Regarding the content type, medical content was four times more frequent than non-medical content. 70% of the medical content posts referred to the low efficacy of the medications, while only 7% mentioned good efficacy. On the other hand, nearly 50% of the posts made mentions to the presence of side effects. (Table 1).
As for non-medical content, posts related to management predominated. Specifically, 25% of non-medical content posts mentioned difficulties in dispensing the medication at the pharmacy. Additionally, almost 15% of the posts expressed complaints about the high cost of the medication. Around 25% of the non-medical content posts requested some form of assistance. Finally, 10% of the non-medical content posts trivialized the use of the medication.
The medical posts that received the most likes/retweets were those referring to low efficacy and those mentioning the presence of side effects. In contrast, in the non-medical content posts, those discussing pharmaceutical dispensation and seeking help received the most likes/retweets (Table 1).
Healthcare professionals are the ones who post the most medical content, while institutions post the least
All users post about medical content, but healthcare professionals, in particular, address medical topics in nearly 90% of their posts. However, healthcare institutions only post about medical topics in two thirds of their posts. (Table 2). Questions were more frequent in posts with non-medical content, and the users who asked the most questions were family members or friends. The percentage of medical posts that considered the medication to be ineffective or minimally effective was 75% for analgesic antidepressants and 69% for anticonvulsants. In other words, users' perception of efficacy was very similar in both pharmacological groups.
Number of posts generated by type of drug, type of user or type of content and number of posts that have generated at least 10 retweets or 10 likes. Percentages add up to more than 100% because there were 1,300 posts containing references to both types of medications. Relative % refers to the number of posts with likes and retweets in relation to their specific number of posts.
| Total posts | Posts with > 10 likes | Posts with > 10 retweets | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | Total % (Relative %) | n | Total % (Relative %) | |||
| COANALGESIC | ||||||||
| Total Coanalgesic | 51,167 | 100.0% | 2,108 | 4.10% | 983 | 1.90% | ||
| Tricyclic Antidepressants | 12,512 | 24.5% | 423 | 0.83% (3.38%) | 112 | 0.20% (0.89%) | ||
| Gabapentinoids | 39,955 | 78.1% | 1,751 | 3.42% (4.38%) | 892 | 1.70% (2.23%) | ||
| User | ||||||||
| Patient | 34,418 | 67.3% | 1,088 | 2.1% (3.16%) | 364 | 0.7% (1.06%) | ||
| Family / friend | 5,104 | 10.0% | 196 | 0.3% (3.84%) | 161 | 0.3% (3.1%) | ||
| Healthcare professional | 6,830 | 13.3% | 528 | 1.0% (7.73%) | 191 | 0.4% (2.8%) | ||
| Institution | 4,815 | 9.4% | 296 | 0.5% (6,15%) | 267 | 0.5% (5.54%) | ||
| Content | ||||||||
| Total Medical content | 40,767 | 79.6% | 1,637 | 3.2% (4.02%) | 405 | 0.7% (1%) | ||
| Efficacy | 31,914 | 62.37% | 1,269 | 2.48% (3.98%) | 295 | 72.8% (0.92%) | ||
| - None or little efficacy | 28,863 | 56.41% | 1,165 | 2.28% (4%) | 277 | 68.4% (0.96%) | ||
| - Good efficacy | 3,051 | 5.96% | 104 | 0.2% (3.4%) | 18 | 4.4% (0.59%) | ||
| Side effects | 19,398 | 37.91% | 893 | 1.75% (4.6%) | 285 | 70.4% (1.47%) | ||
| Total No medical content | 10,400 | 20.3% | 471 | 0.9% (4.52%) | 578 | 1.1% (5.56%) | ||
| Management issues | 6,439 | 12.58% | 284 | 0.56% (4.41%) | 147 | 0.28% (2.28%) | ||
| - Pharmacological dispensing | 2,679 | 5.24% | 93 | 0.18% (3.47%) | 58 | 0.11% (2.16%) | ||
| - Medical prescription | 1,368 | 2.67% | 69 | 0.13% (5%) | 36 | 0.07% (2.63%) | ||
| - Commercial | 1,244 | 2.43% | 55 | 0.11% (4.42%) | 23 | 0.05% (1.85%) | ||
| - Legal issues | 1,148 | 2.24% | 67 | 0.13% (5.84%) | 30 | 0.05% (2.61%) | ||
| Economic aspects | 1,477 | 2.89% | 57 | 0.11% (3.86%) | 31 | 0.05% (2.1%) | ||
| Refers to solidarity | 2,542 | 4.97% | 101 | 0.2% (3.97%) | 442 | 0.86% (17.4%) | ||
| Trivialization | 1,091 | 2.13% | 64 | 0.13% (5.87%) | 14 | 0.03% (1.29%) | ||
| - Humour/Joke | 389 | 0.76% | 23 | 0.04% (5.91%) | 5 | <0.01% (1.29%) | ||
| - Recreational use | 578 | 1.13% | 36 | 0.07% (6.22%) | 8 | <0.01% (1.4%) | ||
| - Song/Poetry/Book | 124 | 0.24% | 5 | <0.01% (4%) | 1 | <0.01% (0.8%) | ||
| Query | ||||||||
| Refer to a Query | 4,200 | 8.2% | 131 | 0.2% (3.11%) | 52 | 0.1% (1.24%) | ||
Number of posts according to publication content and user type. The P value was <0.001 for all comparisons.
| Patient | Family/friend | Healthcare professional | Institution | |||||
|---|---|---|---|---|---|---|---|---|
| N posts | % | N posts | % | N posts | % | N posts | % | |
| Medical content | 28,084 | 81.6% | 3,743 | 73.3% | 5,877 | 86.0% | 3,063 | 63.6% |
| Non-medical content | 6,334 | 18.4% | 1,361 | 26.7% | 953 | 14.0% | 1,752 | 36.4% |
| TOTAL | 34,418 | 100.0% | 5,104 | 100.0% | 6,830 | 100.0% | 4,815 | 100.0% |
| P value <0.001 | ||||||||
Similarly, the percentage of posts mentioning side effects was quite similar in both groups. Anticonvulsants had a slightly higher percentage of posts referring to problems with pharmacy dispensation. We also found a slight increase in the percentage of posts about legal issues related to anticonvulsants. Anticonvulsants had a slightly higher percentage of posts describing recreational use. Anticonvulsants were clearly the subject of a higher percentage of posts mentioning high cost. As for solidarity, antidepressants received a higher percentage of posts (Table 3).
Distribution of drug categories according to medical and non-medical content posts. The P value was <0.001 for all comparisons.
| CATEGORIES | Tricyclic Antidepressants | Gabapentinoids | P-value | ||
|---|---|---|---|---|---|
| N posts | % | N posts | % | ||
| Medical content | |||||
| Total Medical Content | 11,504 | 30,471 | |||
| None or little efficiency | 8,637 | 75.1% | 21,084 | 69.2% | P<0.001 |
| Good efficacy | 750 | 6.5% | 2,448 | 8.0% | |
| Side effects | 5,106 | 44.4% | 14,768 | 48.5% | P<0.001 |
| No Medical content | |||||
| Total No Medical Content | 1,008 | 9,484 | |||
| Total Management | 472 | 46.8% | 6,037 | 63.7% | P<0.001 |
| -Pharmacological dispensing | 155 | 32.8% | 2,533 | 42.0% | |
| -Medical prescription | 109 | 23.1% | 1,280 | 21.2% | |
| -Commercial | 131 | 27.8% | 1,127 | 18.7% | |
| -Legal issues | 77 | 16.3% | 1,097 | 18.2% | |
| Refers to a high cost | 63 | 6.3% | 1,425 | 15.0% | P<0.001 |
| Refers to solidarity | 287 | 28.5% | 2,258 | 23.8% | P<0.001 |
| Total Trivialization | 172 | 17.1% | 924 | 9.7% | P<0.001 |
| -Humor/Joke | 56 | 32.6% | 336 | 36.4% | |
| -Recreational use | 76 | 44.2% | 504 | 54.5% | |
| -Song/Poetry/Book | 40 | 23.3% | 84 | 9.1% | |
Discussion
Our results show that anticonvulsants have been the subject of many more posts than analgesic antidepressants, and they have generated more social media engagement. In terms of content, medical content prevailed, with a reference to the low efficacy of the medication in up to 70% of the occasions and mentioning the presence of side effects in 50% of the posts. This proportion was very similar in both pharmacological groups.
Interestingly, patients emerged as the primary contributors to the highest volume of postings, whereas the contributions from family/friends, healthcare professionals and institutional accounts elicited the greatest level of interest. This reflects that it is the consumer themselves who turn to social media to obtain information, understanding, and support from others. In several previous studies that have examined the type of user engaging in health-related discussions, it has also been found that the most common type of user is patients [43,45]. Likewise, it was also noteworthy for us that despite healthcare professionals are the second group of users identified, their presence in this social media is quite limited in comparison to the highly represented group of patients. Previous studies analysing social media posts related to health topics, the proportion of involved healthcare professionals has been higher than what we found in the present study [54,55].
Pain is a challenging syndrome or symptom to treat. In fact, it is very common to combine medications to achieve adequate pain control. However, in many cases, even with combination therapy, adequate pain control is not achieved [1]. In our study, we found that the most frequently repeated topic in the posts is the low efficacy of these medications. On the contrary, other studies that have also analyzed social media posts about different types of treatments reported a higher perceived efficacy by users, even in posts about diseases such as obesity or ADHD (Attention- Deficit/Hyperactivity Disorder) that are difficult to treat and also require multidisciplinary approaches and combination of treatments [42,55]. On the other hand, despite being medications better tolerated than opioids, adjuvants also have side effects [56], which is reflected in the content of the posts. Nearly 37.9% of the posts mentioned some side effect, which is a higher percentage than reported in other studies analyzing posts about medical treatments [43,45].
Another prevalent topic in the posts is related to dispensing issues at pharmacies. This is concerning because previous studies have reported that this type of medication is frequently included in counterfeit prescriptions [30,57-59]. Furthermore, 13% of the posts identified reservations from doctors about prescribing these medications. This finding is consistent with previous research, as an increasing number of doctors are opposed to their prescription due to agencies warning about the risks associated with their abuse [27,60-62]. In fact, since 2015, a dozen countries worldwide have regulated the prescription and dispensing procedures for pregabalin, and several countries have extended these restrictions to gabapentin[63-65].
2.4% of the posts promoted the medication through social media. Until now, promotion of non-opioid medications through social media had not been reported, which may reflect people's need to alleviate their pain. A potential explanation for this finding is that the posts we analyzed were published throughout 2019 and 2020, partially coinciding with the COVID-19 pandemic. Access to doctors was severely restricted in many regions of the world due to the pandemic. However, the presence of such posts may also be reflecting the existence of irregular online sales, as previously described. It is concerning that despite the efforts made by multiple institutions to regulate access to analgesics, their use without medical prescription continues to increase. Indeed, in a recent survey conducted in the United States, 17% of gabapentin users admitted to obtaining the medication without a medical prescription [56].
On the other hand, 14% of the posts referred to the high cost of the medication. This perception has also been described for other treatments for chronic diseases, such as diabetes. This fact has implications for clinical practice as it leads patients to lean towards cheaper treatments, sometimes at the expense of a diminished efficacy [66,67]. Finally, it is worth noting that we have found minimal stigmatizing content, and we have not found references to suicide or any indication that these medications are currently being used for overdoses. This finding is particularly positive, yet it is crucial to monitor online discussions about drugs used as pain adjuvants, as recent studies indicate an increasing trend in the misuse of gabapentin and pregabalin [25,68-70]. In France, there was a notable rise in reports of gabapentinoid abuse, increasing from 24 cases between 2010 and 2017 to 71 cases in 2018, and further escalating to a total of 117 cases in 2019 [30]. Additionally, the count of gabapentinoid users within the substance-using population increased by a factor of 2.6 between 2018 and 2019. Similarly, in the United Kingdom, using data from the National Programme on Substance Abuse Deaths (NPSAD), it was observed that the number of deaths related to the use of gabapentinoids increased from 8.9% in 2014 to 32.3% in 2020 [71]. In these cases, gabapentin and pregabalin were obtained illicitly in 38.0% of cases. Similar findings have been reported in other European countries [72,73] but also in Australia, as well as Arab and African countries [63,74,75].
Limitations
This study has several limitations. First, it is noteworthy that Twitter users typically skew towards younger demographics, thereby potentially limiting the generalizability of these findings to the broader populace, especially to older cohorts. Indeed, individuals aged 50 to 64 accounted for a mere 21%, while those over 65 represented only 10% of the entire Twitter user base [76]. Second, although our search tool has access to 100% of posts, we may have excluded posts referring to these drugs but using different keywords. Third, while we analyzed the number of retweets and likes generated by each post as an indicator of user interest in a given topic, these engagement metrics can be influenced by other factors and may not accurately reflect user interest. Fourth, we did not geolocate the origin of the posts, thus, even though the posts were written in English, we are uncertain whether they originated from countries such as the UK, the USA, or Australia, for example. Another limitation of this study is the method used to split the dataset into training and test sets. An additional experiment with a split that ensures data leakage is not occurring should be attempted to generalize the results. Finally, content analysis involves a degree of subjectivity, which we have attempted to minimize through prior training and our previous experience in this type of analysis.
Conclusions
This mixed-method analysis of Twitter posts offers a unique and insightful approach to capturing public opinions regarding tricyclic antidepressants, pregabalin, and gabapentin. Unlike traditional survey methods, this approach mitigates social desirability biases by observing spontaneous discussions on a platform unaffected by clinical supervision and closed-ended questions. We found that the most active user type is patients, suggesting that patients frequently turn to social media to express themselves, seek information, find support, and address their medical queries. In fact, the most frequently discussed topics were efficacy, considered low in most posts, and side effects. The prevalence of medically oriented posts underscores the contemporary practice of discussing medical topics on social media, which should encourage institutions and healthcare professionals to engage actively in disseminating accurate medical information through these channels.
Acknowledgements
Funding
This study has been funded by Instituto de Salud Carlos III (ISCIII) through the project “FIS-PI22/00653” and co-funded by the European Union.
Author contributions
FC, MAM y MAA-M: conceptualization, validation, and resources. MAA-M, CD-V, JS, FC and TV: methodology and data curation. CD-V, JS and FJLA: formal analysis. FC, OFM, CGM, LGR, MAM-G, MAO, MAM and MAA-M: investigation, writing original draft, review and editing. MAM, MAO and MAA-M: supervision. All authors have read and agreed to the published version of the manuscript.
Institutional review board statement
This project received approval from the ethics committee of the Hospital Principe de Asturias (OE 14_2020) and is compliant with the research ethics principles of the Declaration of Helsinki (seventh revision, 2013). This study did not directly involve human subjects, nor did it include any intervention; instead uses only publicly available posts (subject to universal access through the internet according to the Terms of Service that all users in Twitter accept). Nevertheless, we have taken care to not directly reveal in this report any username, and we have avoided citing posts that could be offensive or compromised to someone.
Data availability statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. The Lancet. 2021;397(10289):2082-2097
2. Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019;123(2):e273-e283
3. van Rijswijk SM, van Beek MHCT, Schoof GM, Schene AH, Steegers M, Schellekens AF. Iatrogenic opioid use disorder, chronic pain and psychiatric comorbidity: A systematic review. Gen Hosp Psychiatry. 2019;59:37-50
4. Flemming R. Patterns of pregabalin prescribing in four German federal states: analysis of routine data to investigate potential misuse of pregabalin. BMJ Open. 2022;12(7):e060104
5. van den Driest JJ, Schiphof D, de Wilde M, Bindels PJE, van der Lei J, Bierma-Zeinstra SMA. Antidepressant and anticonvulsant prescription rates in patients with osteoarthritis: a population-based cohort study. Rheumatology. 2021;60(5):2206-2216
6. Schneider J, Patterson M, Jimenez XF. Beyond depression: Other uses for tricyclic antidepressants. Cleve Clin J Med. 2019;86(12):807-814
7. Wong J, Motulsky A, Abrahamowicz M, Eguale T, Buckeridge DL, Tamblyn R. Off-label indications for antidepressants in primary care: descriptive study of prescriptions from an indication based electronic prescribing system. BMJ. 2017:j603.
8. Lalji HM, McGrogan A, Bailey SJ. An analysis of antidepressant prescribing trends in England 2015-2019. J Affect Disord Rep. 2021;6:100205
9. Thour A, Marwaha R. Amitriptyline. [Updated 2023 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537225/
10. Brueckle MS, Thomas ET, Seide SE. et al. Adverse drug reactions associated with amitriptyline — protocol for a systematic multiple-indication review and meta-analysis. Syst Rev. 2020;9(1):59
11. Wong J, Motulsky A, Eguale T, Buckeridge DL, Abrahamowicz M, Tamblyn R. Treatment Indications for Antidepressants Prescribed in Primary Care in Quebec, Canada, 2006-2015. JAMA. 2016;315(20):2230
12. Johansen ME. Gabapentinoid Use in the United States 2002 Through 2015. JAMA Intern Med. 2018;178(2):292
13. NFLIS-Drug Special Report. Gabapentin and Pregabalin Reported in NFLIS, 2011-2020. CODE: DEA PRB 2021-54. U.S. Drug Enforcement Administration Diversion Control Division 8701 Morrissette Drive Springfield, VA 22152.; 2022. Accessed August 2. 2024 https://www.nflis.deadiversion.usdoj.gov/nflisdata/docs/NFLIS_Gabapentin_Pregabalin_2011-2020.pdf
14. Montastruc F, Loo SY, Renoux C. Trends in First Gabapentin and Pregabalin Prescriptions in Primary Care in the United Kingdom, 1993-2017. JAMA. 2018;320(20):2149
15. Benassayag Kaduri N, Dressler R, Abu Ahmad W, Rotshild V. Trends in Pregabalin Use and Prescribing Patterns in the Adult Population: A 10-Year Pharmacoepidemiologic Study. CNS Drugs. 2024;38(2):153-162
16. Ashworth J, Bajpai R, Muller S. et al. Trends in gabapentinoid prescribing in UK primary care using the Clinical Practice Research Datalink: an observational study. The Lancet Regional Health - Europe. 2023;27:100579
17. Kardas P, Urbański F, Lichwierowicz A. et al. The Prevalence of Selected Potential Drug-Drug Interactions of Analgesic Drugs and Possible Methods of Preventing Them: Lessons Learned From the Analysis of the Real-World National Database of 38 Million Citizens of Poland. Front Pharmacol. 2021 11
18. Gillman PK. Tricyclic antidepressant pharmacology and therapeutic drug interactions updated. Br J Pharmacol. 2007;151(6):737-748
19. Onakpoya IJ, Thomas ET, Lee JJ, Goldacre B, Heneghan CJ. Benefits and harms of pregabalin in the management of neuropathic pain: a rapid review and meta-analysis of randomised clinical trials. BMJ Open. 2019;9(1):e023600
20. Kolasinski SL, Neogi T, Hochberg MC. et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis & Rheumatology. 2020;72(2):220-233
21. Farag HM, Yunusa I, Goswami H, Sultan I, Doucette JA, Eguale T. Comparison of Amitriptyline and US Food and Drug Administration-Approved Treatments for Fibromyalgia. JAMA Netw Open. 2022;5(5):e2212939
22. Bendtsen L, Jensen R. Amitriptyline Reduces Myofascial Tenderness in Patients with Chronic Tension-Type Headache. Cephalalgia. 2000;20(6):603-610
23. Kerr GW. Tricyclic antidepressant overdose: a review. Emergency Medicine Journal. 2001;18(4):236-241 doi:10.1136/emj.18.4.236
24. Goodman CW, Brett AS. Gabapentin and Pregabalin for Pain — Is Increased Prescribing a Cause for Concern? New England Journal of Medicine. 2017;377(5):411-414
25. Evoy KE, Sadrameli S, Contreras J, Covvey JR, Peckham AM, Morrison MD. Abuse and Misuse of Pregabalin and Gabapentin: A Systematic Review Update. Drugs. 2021;81(1):125-156
26. Lockhart P, Guthrie B. Trends in primary care antidepressant prescribing 1995-2007: a longitudinal population database analysis. British Journal of General Practice. 2011;61(590):e565-e572
27. Prahlow JA, Landrum JE. Amitriptyline Abuse and Misuse. American Journal of Forensic Medicine & Pathology. 2005;26(1):86-88
28. Sein Anand J, Chodorowski Z, Habrat B. Recreational amitriptyline abuse. Przegl Lek. 2005;62(6):397-398
29. M Peckham A, Ananickal M, Sclar D. Gabapentin use, abuse, and the US opioid epidemic: the case for reclassification as a controlled substance and the need for pharmacovigilance. Risk Manag Healthc Policy. 2018;11:109-116
30. Tambon M, Ponté C, Jouanjus E, Fouilhé N, Micallef J, Lapeyre-Mestre M. Gabapentinoid Abuse in France: Evidence on Health Consequences and New Points of Vigilance. Front Psychiatry. 2021;12:639780
31. Chapman SCE, Horne R, Chater A, Hukins D, Smithson WH. Patients' perspectives on antiepileptic medication: Relationships between beliefs about medicines and adherence among patients with epilepsy in UK primary care. Epilepsy & Behavior. 2014;31:312-320
32. Soffin EM, Lee BH, Kumar KK, Wu CL. The prescription opioid crisis: role of the anaesthesiologist in reducing opioid use and misuse. Br J Anaesth. 2019;122(6):e198-e208
33. Willey C, Redding C, Stafford J. et al. Stages of change for adherence with medication regimens for chronic disease: Development and validation of a measure. Clin Ther. 2000;22(7):858-871
34. Groenewegen A, Tofighy A, Ryvlin P, Steinhoff BJ, Dedeken P. Measures for improving treatment outcomes for patients with epilepsy — Results from a large multinational patient-physician survey. Epilepsy & Behavior. 2014;34:58-67
35. Mohammed MA, Moles RJ, Chen TF. Medication-related burden and patients' lived experience with medicine: a systematic review and metasynthesis of qualitative studies. BMJ Open. 2016;6(2):e010035
36. Haslam C. Patients' experiences of medication for anxiety and depression: effects on working life. Fam Pract. 2004;21(2):204-212
37. Zhou Z, Hultgren KE. Complementing the US Food and Drug Administration Adverse Event Reporting System With Adverse Drug Reaction Reporting From Social Media: Comparative Analysis. JMIR Public Health Surveill. 2020;6(3):e19266
38. Sarker A, Ginn R, Nikfarjam A. et al. Utilizing social media data for pharmacovigilance: A review. J Biomed Inform. 2015;54:202-212
39. Golder S, Norman G, Loke YK. Systematic review on the prevalence, frequency and comparative value of adverse events data in social media. Br J Clin Pharmacol. 2015;80(4):878-888
40. Branley DB, Covey J. Pro-ana versus Pro-recovery: A Content Analytic Comparison of Social Media Users' Communication about Eating Disorders on Twitter and Tumblr. Front Psychol. 2017;8:1356
41. Emmert-Streib F, Yli-Harja O, Dehmer M. Utilizing Social Media Data for Psychoanalysis to Study Human Personality. Front Psychol. 2019;10:2596
42. Alvarez-Mon MA, de Anta L, Llavero-Valero M. et al. Areas of Interest and Attitudes towards the Pharmacological Treatment of Attention Deficit Hyperactivity Disorder: Thematic and Quantitative Analysis Using Twitter. J Clin Med. 2021;10(12):2668
43. Golder S, O'Connor K, Hennessy S, Gross R, Gonzalez-Hernandez G. Assessment of Beliefs and Attitudes About Statins Posted on Twitter. JAMA Netw Open. 2020;3(6):e208953
44. Farrar M, Lundt L, Franey E, Yonan C. Patient perspective of tardive dyskinesia: results from a social media listening study. BMC Psychiatry. 2021;21(1):94
45. Golder S, Bach M, O'Connor K, Gross R, Hennessy S, Gonzalez Hernandez G. Public Perspectives on Anti-Diabetic Drugs: Exploratory Analysis of Twitter Posts. JMIR Diabetes. 2021;6(1):e24681
46. Helm JM, Swiergosz AM, Haeberle HS. et al. Machine Learning and Artificial Intelligence: Definitions, Applications, and Future Directions. Curr Rev Musculoskelet Med. 2020;13(1):69-76
47. LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521(7553):436-444
48. Jiang W. Applications of deep learning in stock market prediction: Recent progress. Expert Syst Appl. 2021;184:115537
49. Strauman AS, Bianchi FM, Mikalsen KØ, Kampffmeyer M, Soguero-Ruiz C, Jenssen R. Classification of postoperative surgical site infections from blood measurements with missing data using recurrent neural networks. arXiv. 2017
50. Zhao ZQ, Zheng P, Xu ST, Wu X. Object Detection With Deep Learning: A Review. IEEE Trans Neural Netw Learn Syst. 2019;30(11):3212-3232
51. C A Padmanabha Reddy Y, Viswanath P, Eswara Reddy B. Semi-supervised learning: a brief review. International Journal of Engineering & Technology. 2018;7(1.8):81
52. Hady MFA, Schwenker F. Semi-supervised Learning. In: Handbook on Neural Information Processing. 2013:215-239
53. Conneau A, Khandelwal K, Goyal N. et al. Unsupervised Cross-lingual Representation Learning at Scale. In: Proceedings of the 58th Annual Meeting of the Association for Computational Linguistics. Association for Computational Linguistics. 2020:8440-8451
54. de Anta L, Alvarez-Mon MA, Donat-Vargas C. et al. Assessment of beliefs and attitudes about electroconvulsive therapy posted on Twitter: An observational study. European Psychiatry. 2023;66(1):e11
55. Alvarez-Mon MA, Llavero-Valero M, Asunsolo del Barco A. et al. Areas of Interest and Attitudes Toward Antiobesity Drugs: Thematic and Quantitative Analysis Using Twitter. J Med Internet Res. 2021;23(10):e24336
56. Magin PJ, Morgan S, Tapley A. et al. Anticholinergic medicines in an older primary care population: a cross-sectional analysis of medicines' levels of anticholinergic activity and clinical indications. J Clin Pharm Ther. 2016;41(5):486-492
57. Jouanjus E, Guernec G, Lapeyre-Mestre M. Medical prescriptions falsified by the patients: a 12-year national monitoring to assess prescription drug diversion. Fundam Clin Pharmacol. 2018;32(3):306-322
58. Kesselheim AS, Darby D, Studdert DM, Glynn R, Levin R, Avorn J. False Claims Act Prosecution Did Not Deter Off-Label Drug Use In The Case Of Neurontin. Health Aff. 2011;30(12):2318-2327
59. Boeuf O, Lapeyre-Mestre M. Survey of Forged Prescriptions to Investigate Risk of Psychoactive Medications Abuse in France. Drug Saf. 2007;30(3):265-276
60. Gahr M, Freudenmann RolandW, Hiemke C, Kölle MA, Schönfeldt-Lecuona C. Pregabalin abuse and dependence in Germany: results from a database query. Eur J Clin Pharmacol. 2013;69(6):1335-1342
61. International Narcotics Control Board. 2021 Annual Report; 2022. Accessed August 2. 2024 https://www.incb.org/documents/Publications/AnnualReports/AR2021/Annual_Report/E_INCB_2 524 021_1_eng.pdf
62. European Monitoring Centre for Drugs and Drug Addiction, 2010 Annual report on the state of the drugs problem in Europe, Publications Office; 2010. https://data.europa.eu/doi/10.2810/33349. Accessed August 2, 2024. https://op.europa.eu/en/publication-detail/-/publication/9b6ed0af-83ee-40ea-ae00-2da84a67c9f8
63. Schaffer AL, Busingye D, Chidwick K, Brett J, Blogg S. Pregabalin prescribing patterns in Australian general practice, 2012-2018: a cross-sectional study. BJGP Open. 2021;5(1):bjgpopen20X101120
64. Iacobucci G. UK government to reclassify pregabalin and gabapentin after rise in deaths. BMJ. 2017;358:j4441
65. Mayor S. Pregabalin and gabapentin become controlled drugs to cut deaths from misuse. BMJ. 2018;363:k4364
66. Fishman J, Cohen G, Josephson C. et al. Patient emotions and perceptions of antiepileptic drug changes and titration during treatment for epilepsy. Epilepsy & Behavior. 2017;69:44-52
67. Mathieson S, O'Keeffe M, Traeger AC, Ferreira GE, Abdel Shaheed C. Content and sentiment analysis of gabapentinoid-related tweets: An infodemiology study. Drug Alcohol Rev. 2024;43(1):45-55
68. Evoy KE, Morrison MD, Saklad SR. Abuse and Misuse of Pregabalin and Gabapentin. Drugs. 2017;77(4):403-426
69. Smith R V, Havens JR, Walsh SL. Gabapentin misuse, abuse and diversion: a systematic review. Addiction. 2016;111(7):1160-1174 doi:10.1111/add.13324
70. Hägg S, Jönsson AK, Ahlner J. Current Evidence on Abuse and Misuse of Gabapentinoids. Drug Saf. 2020;43(12):1235-1254
71. Kalk NJ, Chiu C, Sadoughi R. et al. Fatalities associated with gabapentinoids in England (2004-2020). Br J Clin Pharmacol. 2022;88(8):3911-3917
72. Kuhn D, Müller TJ, Mutschler J. [Pregabalin abuse and dependence in various European countries: Association with substitution policies]. Fortschr Neurol Psychiatr. 2021;89(11):553-561
73. Baftiu A, Johannessen Landmark C, Rusten IR, Feet SA, Johannessen SI, Larsson PG. Changes in utilisation of antiepileptic drugs in epilepsy and non-epilepsy disorders—a pharmacoepidemiological study and clinical implications. Eur J Clin Pharmacol. 2016;72(10):1245-1254
74. Alsheikh MY, Alshahrani AM, Almutairi RD. et al. Analysis of Gabapentinoids Abuse-Reports in the Middle East and North Africa Region Utilizing the Food and Drug Administration Adverse Event Reporting System. Pharmacology, Toxicology and Biomedical Reports. 2021;7(1):5-8
75. Althunian TA, Alomran MI, Alsagri GM, Alrasheed MM, Alshammari TM. The impact of regulatory restrictions on pregabalin use in Saudi Arabia: An interrupted time series analysis. Pharmacoepidemiol Drug Saf. 2022;31(5):577-582
76. Manchikanti L, Helm S, Fellows B. et al. Opioid epidemic in the United States. Pain Physician. 2012;15(3 Suppl):ES9-38
Author contact
![]() Corresponding author: fcarabotcom. Department of Medicine and Medical Specialities. University of Al-cala, 28801, Alcala de Henares, Madrid, Spain.
Corresponding author: fcarabotcom. Department of Medicine and Medical Specialities. University of Al-cala, 28801, Alcala de Henares, Madrid, Spain.

 Global reach, higher impact
Global reach, higher impact