Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(14):2705-2713. doi:10.7150/ijms.103532 This issue Cite
Research Paper
Innovative Categorization and Operative Management of Auditory Ossicle Disruption Following Trauma: Therapeutic Efficacy and Interventional Paradigms
1. Department of Otolaryngology, Head and Neck Surgery, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou 510120, P.R. China.
2. Department of Otolaryngology, Head and Neck Surgery, ShenShan Medical Center, Memorial Hospital of Sun Yat-sen University, Shanwei 516400, P.R. China.
Received 2024-9-11; Accepted 2024-10-4; Published 2024-10-14
Abstract
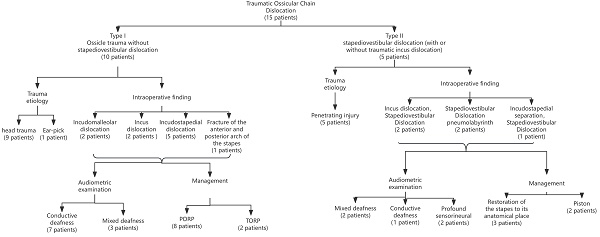
Currently, there is no consensus on the treatment protocol for ossicular chain trauma. This study aims to investigate the classification and treatment strategies for traumatic ossicular chain dislocation. We retrospectively analyzed 15 patients. Traumatic ossicular chain dislocations were categorized based on the location of trauma identified during surgery: Type I—ossicular trauma without stapediovestibular dislocation; Type II—stapediovestibular dislocation (with or without associated incus dislocation). Of the 10 patients with Type I trauma, 9 experienced head trauma, and 1 had a penetrating injury to the external auditory canal. Among these, 2 cases involved incudomalleolar dislocation, 2 cases incus dislocation, 5 cases incudostapedial dislocation, and 1 case a fracture of the anterior and posterior arches of the stapes. Seven patients exhibited conductive hearing loss, while 3 presented with mixed hearing loss. Ossiculoplasty was performed using partial ossicular replacement prostheses (PORP) in 8 patients and total ossicular replacement prostheses (TORP) in 2 patients. Postoperative air conduction thresholds significantly improved in all 10 patients. In Type II trauma, all 5 patients had a penetrating injury to the external auditory canal, resulting in varying degrees of hearing loss. Postoperatively, 3 patients experienced improvement in hearing, while 2 showed no significant change. All patients developed vertigo and tinnitus following the trauma, with vertigo resolving after surgery. Pneumolabyrinth was detected in 2 patients. We propose a novel classification system for traumatic ossicular chain dislocation. Treatment strategies should be tailored according to the specific trauma type.
Keywords: Traumatic Ossicular Chain Dislocation, Classification, Ossiculoplasty, Stapediovestibular Dislocation, Pneumolabyrinth
Introduction
Ossicular chain trauma can arise from various etiologies [1, 2], including head injuries, such as those resulting from traffic accidents or falls from heights, as well as penetrating injuries to the external auditory canal, often caused by the insertion of foreign objects. Head trauma is frequently accompanied by temporal bone fractures, leading to varying degrees of facial paralysis, whereas penetrating injuries typically do not result in such complications. Studies have suggested that head trauma is the most common cause of ossicular chain damage [3, 4]. Hough [5] proposed three primary mechanisms underlying ossicular chain injury: 1) The shock from head trauma can cause skull fractures, leading to the instantaneous separation of tissues, thereby reducing their elasticity and structural integrity; 2) According to Newton's first law—which states that an object in motion or at rest will remain in that state unless acted upon by an external force—when the head is struck while relatively stationary, it moves, but the intracranial structures, including the ossicular chain, remain stationary, resulting in inertial forces that can cause injury to the ossicles; 3) Violent stimulation can cause the contraction of intratympanic muscles, subjecting the auditory ossicles to multidirectional forces [6].
Ossicular chain trauma typically manifests as either ossicular dislocation or fracture, with dislocation being more common. Research has shown that the incus is more frequently affected than the malleus and stapes [7-10]. The difference in incidence may be due to the anatomical characteristics of each ossicle, rather than trauma alone. The stapes are protected by the annular ligament and the stapedius muscle, while the malleus is stabilized by the anterior and lateral ligaments, along with the tensor tympani tendon attached to the superior part of the malleus handle [11]. Consequently, when the middle ear is subjected to trauma, the incus is more prone to displacement or fracture. Dislocation of the incus can occur at the incudomalleolar joint, the incudostapedial joint, or both, with incudostapedial dislocation being the most common [3].
Currently, the types of ossicular chain trauma have yet to be systematically classified. Clinically, ossicular chain disruption can be roughly categorized based on tympanic exploration into several types [3, 12, 13]: incudostapedial dislocation, incudomalleolar separation or dislocation, dislocation of the malleus or incus, stapediovestibular dislocation (both external and internal), and ossicle fracture [14].
Due to the limited number of cases, particularly those involving stapediovestibular dislocation, no standardized treatment protocol currently exists. Given the relative lack of research, the purpose of this study is to investigate the classification and treatment of traumatic ossicular chain dislocation [15].
Materials and Methods
Ethical statement
All of the participants provided informed consent and the study received approval from the Institutional Review Board (SYSKY-2024-889-01) of Sun Yat-sen Memorial Hospital's ethics committee. Written informed consent was obtained from all participants in accordance with the principles defined in the Declaration of Helsinki.
Study design
This retrospective study analyzed 15 patients diagnosed with traumatic ossicular chain dislocation at the Department of Otorhinolaryngology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, between 2015 and 2023. The patients' ages ranged from 14 to 62 years, with 11 males and 4 females. The etiologies of trauma included head trauma in 9 patients and penetrating injuries to the external auditory canal in 6 patients. One patient was admitted directly to the emergency department, while the remaining patients received initial conservative treatment at local hospitals. The interval between the trauma and admission to our hospital varied from 1 month to 6 years. The primary symptoms reported were hearing loss, vertigo, and tinnitus, as detailed in Table 1.
All patients underwent pure tone audiometry both preoperatively and 6 months postoperatively. Air conduction (AC) and air-bone gap (ABG) thresholds were calculated as averages across frequencies of 0.5, 1.0, 2.0, and 4.0 kHz. Additionally, all patients received high-resolution computed tomography (HRCT) scans of the temporal bone prior to surgery, with cranial MRI performed to exclude craniocerebral or cranial nerve injuries [16]. Based on the intraoperative findings regarding the trauma location, traumatic ossicular chain dislocations were classified as follows: Type I, Ossicular trauma without stapediovestibular dislocation and Type II, Stapediovestibular dislocation (with or without associated incus dislocation).
Statistical analysis
Statistical analysis was carried out with SPSS version 27.0 (IBM Corporation, NY, USA). Descriptive statistics were shown as mean ± standard deviation or median (inter-quartile range), based on the normality of the data. Independent t-tests or Mann-Whitney U tests were used for comparing groups, as suitable. Categorical data were presented as counts and percentages. For comparing categorical data between groups, Fisher's exact tests or chi-squared tests were applied. A two-sided p-value of less than 0.05 was considered statistically significant.
Results
Table 1 provides a detailed overview of the clinical and treatment characteristics of the 15 patients included in this study. All patients exhibited varying degrees of hearing loss, with 8 patients (53.3%) presenting with conductive hearing loss, 6 patients (40%) with mixed hearing loss, and 1 patient (6.7%) with profound hearing loss. Additionally, 9 patients (60%) reported tinnitus, and 5 patients (33.3%) experienced vertigo.
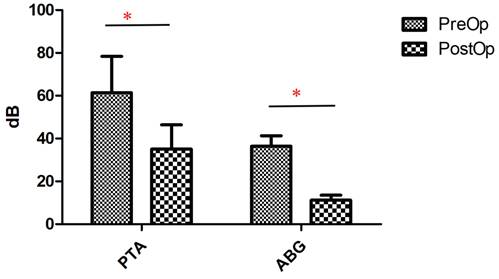
The traumas were categorized into two types based on the presence of stapediovestibular dislocation (as detailed in Table 2). Among the 10 patients classified with Type I trauma, 9 had sustained head trauma, while 1 had suffered a penetrating injury to the external auditory canal (caused by an ear pick). In this group, 2 patients exhibited incudomalleolar dislocation, 2 patients had incus dislocation (one of whom also had a fracture of the anterior and posterior arches of the stapes), 5 patients presented with incudostapedial dislocation, and 1 patient had a fracture of the anterior and posterior arches of the stapes. Of the 10 patients with Type I trauma, 7 had conductive hearing loss, and 3 had mixed hearing loss. Ossicular reconstruction was performed using a partial ossicular replacement prosthesis (PORP) in 8 patients and a total ossicular replacement prosthesis (TORP) in 2 patients. Postoperative pure tone audiometry revealed a significant improvement in hearing thresholds in all 10 patients (p < 0.05) (Figure 1).
Comparison of pure-tone audiometry (PTA) and ABG thresholds of type I trauma patients before and after surgery. *p<0.05.
Clinical Characters of 15 Cases with Traumatic Ossicular Chain Dislocation
| Patient | Age/Sex | Trauma etiology | Treatment delay | Clinical symptoms | Intraoperative finding | Management | Audiometric examination | Preop-PTA, dB | Preop-ABG, dB | Postop-PTA, dB | Postop-ABG, dB |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 14/M | Head trauma | 1month | Hearing loss | IS separation | PORP | Conductive | 50 | 35 | 30 | 12.5 |
| 2 | 40/M | Head trauma | 1month | Hearing loss | IS separation | PORP | Conductive | 58.75 | 35 | 33.75 | 10 |
| 3 | 51/M | Head trauma | 1month | Hearing loss | Incus dislocation | PORP | Conductive | 48.75 | 37.5 | 20 | 7.5 |
| 4 | 62/F | Ear-pick | 13days | Hearing loss, Tinnitus | Incus dislocation Fracture of the anterior and posterior arch of the stape | TORP | Mixed | 92 | 45 | 60 | 15 |
| 5 | 31/M | Head trauma | 9months | Hearing loss | IM separation | PORP | Conductive | 44 | 31 | 28 | 12 |
| 6 | 26/M | Traffic accident | 2years | Hearing loss, Tinnitus | IS separation | PORP | Mixed | 76 | 32.5 | 40 | 10 |
| 7 | 38/M | Head trauma | 7months | Hearing loss, Tinnitus | IM separation | PORP | Mixed | 82 | 40 | 45 | 9 |
| 8 | 41/F | Head trauma | 1month | Hearing loss | IS separation | PORP | Conductive | 47 | 35 | 24 | 9 |
| 9 | 49/F | Head trauma | 3years | Hearing loss | IS separation | PORP | Conductive | 65 | 42 | 35 | 11 |
| 10 | 31/F | Head trauma | 6years | Hearing loss, Tinnitus | Fracture of the anterior and posterior arch of the stape | TORP | Conductive | 67 | 40 | 36 | 12 |
| 11 | 39/M | The branch | 3months | Hearing loss, Vertigo, Tinnitus | Incus dislocation, Stapediovestibular Dislocation | Piston (0.4*7mm) | Conductive | 57.5 | 36.25 | 32.5 | 12.5 |
| 12 | 42/M | Ear-pick | 5months | Hearing loss, Vertigo, Tinnitus | Stapediovestibular Dislocation pneumolabyrinth | RO | Mixed | 88.75 | 48.75 | 53.75 | 5 |
| 13 | 33/M | Ear-pick | 1year | Hearing loss, Vertigo, Tinnitus | Incus dislocation, Stapediovestibular Dislocation | Piston (0.4*7mm) | Mixed | 85 | 30 | 70 | 25 |
| 14 | 19/M | Bamboo chopsticks | Immediately | Hearing loss, Vertigo, Tinnitus | IS separation, Stapediovestibular Dislocation | Medication and RO | Profound sensorineural | >100 | NA | >100 | NA |
| 15 | 50/M | Ear-pick | 4months | Hearing loss, Vertigo, Tinnitus | Stapediovestibular Dislocation pneumolabyrinth | Medication and RO | Profound sensorineural | >100 | NA | >100 | NA |
RO, restoration of the stapes to its anatomical place
The Classification for Traumatic Ossicular Chain Dislocation
| Type I | Type II | |
|---|---|---|
| Total number of patients | 10 | 5 |
| Cause: Head trauma (impact, car accident) | 9 | / |
| Cause: Penetrating trauma of the external auditory canal | 1 | 5 |
| Audiometric examination | ||
| Conductive | 7 | 1 |
| Mixed | 3 | 2 |
| Profound sensorineural | / | 2 |
Case information for Patient 11. A and B: Stapediovestibular dislocation can be seen in the HRCT. C: the preoperative audiogram of patient 11. D: the postoperative audiogram.
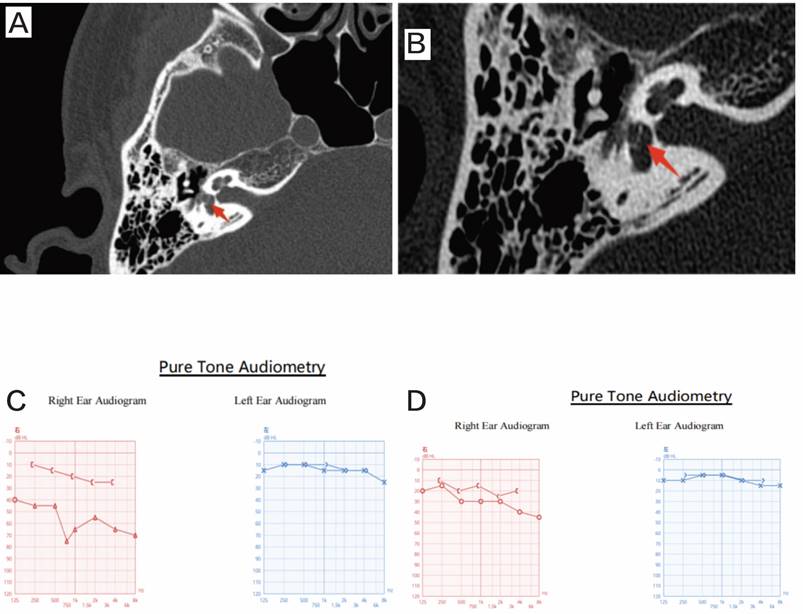
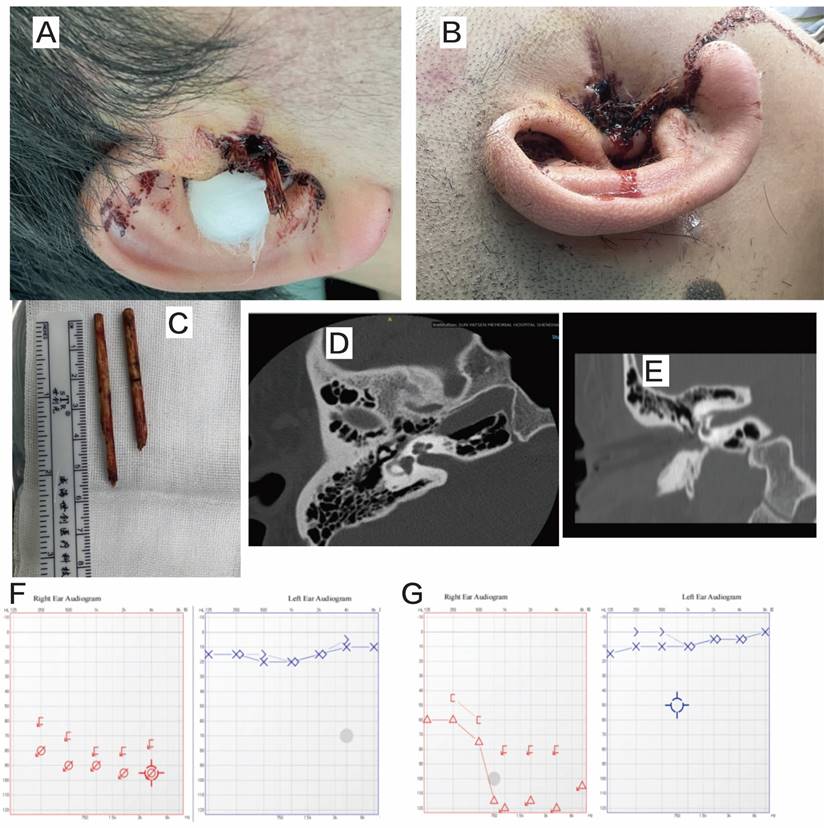
All 5 patients with Type II trauma had sustained penetrating injuries, leading to varying degrees of hearing loss. Specifically, 2 patients had mixed hearing loss, 1 had conductive hearing loss, and 2 had profound hearing loss. Postoperative hearing improvement was observed in patients 11-13, whereas no significant change was noted in patients 14-15. All 5 patients developed vertigo and tinnitus following the trauma. Among these, 2 patients (patients 11 and 13) exhibited incus dislocation, and 2 patients (patients 12 and 15) were diagnosed with pneumolabyrinth.
In the 2 patients with Type II trauma and incus dislocation, intraoperative findings revealed depression of the stapes. Following the removal of the stapes, the incus dislocation was confirmed. The oval window was sealed with fat, and a piston (0.4 × 7 mm) was placed between the fat and the neck of the malleus. Postoperatively, vertigo resolved in these patients (Figure 2).
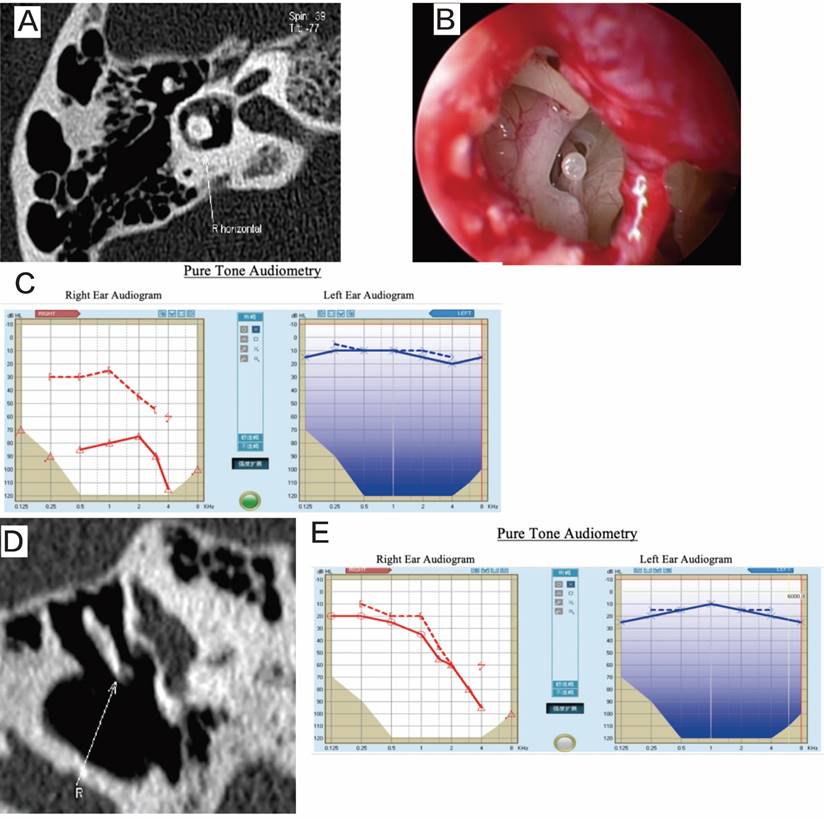
The 2 patients with pneumolabyrinth experienced recurrent positional vertigo and positive Roll test results after the trauma. Based on the trauma history and HRCT findings, it was determined that stapediovestibular dislocation with pneumolabyrinth had occurred. Intraoperative exploration revealed stapes depression. After removing the stapes, the vestibule was sealed with fat, and the stapes was repositioned. Vertigo resolved in both patients postoperatively (Figure 3).
One patient was admitted to the emergency department on the day of the trauma. Pure tone audiometry indicated profound sensorineural deafness, and HRCT revealed incudomalleolar dislocation. Intraoperative exploration showed slight depression of the stapes with perilymphatic leakage from the oval window. The stapes was repositioned, and the footplate was sealed with fat. No perilymphatic fistulae were observed postoperatively, and the patient's vertigo resolved (Figure 4).
Patient 12. A: preoperative CT, revealing pneumolabyrinth. B: the deep depression of the stapes into the vestibule. C: preoperative audiogram. D: postoperative HRCT, showing that the pneumolabyrinth has been resolved. E: postoperative audiogram.
Discussion
Ossicular chain trauma is predominantly caused by head injuries, while the incidence of direct injury (penetrating trauma) to the external auditory canal is relatively low [17, 18]. A previous study reported that of 166 cases of traumatic ossicle dislocation, 160 (96%) were attributable to head trauma [3]. Similarly, another study involving 42 patients with traumatic ossicle dislocation found that 39 (92.8%) had experienced head trauma [9]. Interestingly, cultural practices appear to influence the etiology of such trauma. For instance, a study conducted in Japan identified ear-picking injuries as the most common cause of traumatic ossicle dislocation, which is linked to the cultural practice of using ear picks for ear cleaning in Japan [19, 20]. In our country, the use of ear picks or cotton swabs for ear cleaning is also prevalent. In our study, 5 of the 15 patients sustained direct injuries to the external auditory canal: 3 from ear picking, 1 from an accidental stab with a tree branch, and 1 from the insertion of bamboo chopsticks into the ear canal.
Patient 14. A and B: penetrating trauma to the external auditory canal (bamboo chopsticks). C: the foreign body (bamboo chopsticks). D and E: preoperative HRCT. F: preoperative audiogram. G: postoperative audiogram.
Based on the presence of stapediovestibular dislocation, the traumas were categorized into Type I and Type II. Etiologically, Type I traumas were primarily caused by head injuries (9/10) [21, 22], while Type II traumas were exclusively associated with penetrating injuries to the external auditory canal (5/5). In terms of hearing impairment, Type I traumas were mainly accompanied by conductive hearing loss, whereas Type II traumas predominantly resulted in reduced bone conduction, with both mixed and profound sensorineural hearing loss being possible. Patients with Type II trauma exhibited more severe hearing impairment [21], while those with Type I trauma demonstrated more significant postoperative hearing improvement. Symptomatically, Type II patients were more likely to experience tinnitus and vertigo. We hypothesize that Type II patients suffered varying degrees of stapediovestibular dislocation, depression, perilymphatic fistula, or even pneumolabyrinth, which contributed to varying degrees of decreased bone conduction and vertigo. According to the literature, stapediovestibular dislocation can lead to lymphatic exposure, resulting in a range of cochlear vestibular symptoms, including sensorineural hearing loss, mixed hearing loss, and vertigo. Studies have indicated that some patients experience lymphadenopathy immediately following an accident. Patients who lose consciousness or sustain more serious injuries to other organs may overlook vestibular system symptoms. Regarding treatment delay, only 1 patient was admitted to the emergency department, while the remaining patients received conservative treatment at local hospitals and later sought further medical care due to hearing loss or vertigo. Compared to Type I trauma, the treatment delays for Type II trauma were shorter, likely due to the recurrent vertigo experienced by Type II patients after conservative treatment, whereas the longer treatment delay for Type I trauma may be attributed to the patients' primary concern with hearing improvement.
In treating Type I patients, ossiculoplasty was performed based on the separation or dislocation of the ossicles and the condition of the stapes. Partial ossicular replacement prostheses (PORPs) or total ossicular replacement prostheses (TORPs) were utilized for reconstruction. Postoperative hearing improvement was significant, with air-bone gap (ABG) thresholds reduced to within 10 dB in 50% (5/10) and within 20 dB in 100% (10/10) of patients. A previous study reported that 73.3% and 100% of patients had postoperative ABG thresholds within 10 dB and 20 dB, respectively [8]. Another study [17] indicated that ABG thresholds ranged from 0-10 dB in 65% of patients and from 11-20 dB in 30%. Yet another study [23, 24] compared different ossicle materials and reconstruction methods, such as autologous ossicles or titanium ossicular replacement prostheses. In the study by Chien et al. [25], the hearing outcomes of the titanium prosthesis group and the autologous incus group were compared, and both groups demonstrated good hearing restoration.
For Type II patients, after intraoperative exploration of the vestibule and stapes, different ossicle reconstruction methods were employed depending on whether the incus was dislocated. In two cases of incus dislocation, both the stapes and incus were removed, the oval window was sealed with fat, and a piston (0.4 × 7 mm) was placed between the fat and the neck of the malleus. In two patients with normal incus anatomy but presenting with pneumolabyrinth, the stapes was first removed, the vestibule was filled with fat, and the stapes was repositioned between the incus and the fat. One patient with preoperative profound sensorineural deafness underwent stapes repositioning during surgery. However, hearing improvement was not significant in the two patients with profound sensorineural deafness, while the remaining three patients showed varying degrees of improvement [26].
Studies have shown that stapediovestibular dislocation is a rare occurrence [27-31], which can be categorized into internal dislocation (depression into the vestibule) and external dislocation, with the latter being even rarer. Internal dislocations are often caused by direct penetrating injuries with cotton swabs or ear picks, whereas external dislocation can occur when ligaments are torn by traumatic force. Comminuted fractures of the stapes footplate can also result in stapediovestibular dislocation. Surgical exploration in all five of our patients revealed internal dislocation [32, 33].
Currently, there is no consensus on the treatment protocol for stapediovestibular dislocation [34]. Some studies suggest that removal of the stapes may cause additional damage, leading to postoperative hearing loss [28, 34, 35]. It has also been proposed that if the stapes remains in the vestibule, scar formation around the stapes may eventually occupy the vestibular space, causing late-onset inner ear injury [36-38]. Certain studies recommend surgical exploration to remove the stapes from the vestibule [28, 36, 39]. Arragg and Paparella suggested that immediate surgical intervention, including resection or elevation of the stapes, is necessary for stapes fractures involving depression into the vestibule [30, 40]. However, even when stapes depressed deep into the vestibule are removed, hearing restoration may not be satisfactory, and there is a risk of sensorineural hearing loss [34]. According to one study [36, 41], when dislocation of the stapes into the vestibule is suspected, it is crucial to assess the depth of stapes depression and the presence of fractures. Studies have demonstrated that when the stapes are only slightly depressed into the vestibule, good hearing reconstruction outcomes can be achieved regardless of whether the stapes is resected [30, 42]. However, when the stapes are deeply compressed into the vestibule, the risk of inner ear injury increases, leading to poor postoperative hearing recovery [37, 43, 44]. The treatment of stapediovestibular dislocation depends on the integrity and position of the stapes, as well as the preoperative hearing status. The most common approaches include reduction or removal of the stapes, followed by sealing the oval window with fascia or fat before hearing reconstruction [45, 46].
In this study, two patients experienced recurrent paroxysmal positional vertigo after trauma, and pneumolabyrinth was detected via HRCT examination. Ederies et al. [47, 48] proposed the “pneumopositional” theory, wherein the movement of air bubbles in the vestibule or semicircular canal induces positional vertigo. This hypothesis is supported by HRCT findings [49, 50], which showed air movement in the vestibule or semicircular canal as the body position changed, leading to cupular deflection and ampullary stimulation, followed by the onset of nystagmus and vertigo. Tsubota et al. [51, 52] identified three predictive factors for hearing improvement following pneumolabyrinth: bone conduction hearing level after trauma, the interval between injury and surgery, and the presence of stapes lesions. A meta-analysis by Hidaka et al. [53, 54] found that while vestibular symptoms in patients with pneumolabyrinth were effectively alleviated after treatment, hearing outcomes varied: among those with pneumolabyrinth limited to the vestibular organ, 48% of patients experienced hearing improvement, but if pneumolabyrinth extended to both the vestibule and cochlea, hearing did not improve significantly. In our study, one patient with severe mixed hearing loss before surgery showed postoperative hearing improvement, while the other, who had very severe preoperative hearing loss, did not experience hearing improvement after surgery. The meta-analysis by Hidaka et al. found no significant difference in efficacy between conservative and surgical treatments [55, 56].
In our study, patients with Type I trauma showed substantial postoperative hearing improvement. Different ossiculoplasty methods were selected based on the presence of structures above the stapes [57, 58]. Ossicular replacement prostheses were used for reconstruction, resulting in effective postoperative hearing improvement. Conversely, in Type II patients who experienced repeated paroxysmal positional vertigo after the trauma event, pneumolabyrinth should be suspected. Postoperatively, vertigo in Type II patients was effectively alleviated, although hearing compensation was poor [59, 60]. After carefully removing the stapes during surgery, the vestibule was sealed with fat or fascia [61, 62]. Different hearing reconstruction methods were chosen based on the condition of the incus. If the incus was normal, the stapes were reduced; if the incus was dislocated, a piston (0.4 × 7 mm) was used for hearing reconstruction. Treatment strategies were tailored according to the classification, guiding the prognosis of the patients [63].
The sample size of this study was small, and future research should aim to increase the number of patients analyzed. Additionally, for Type I patients, a control group consisting of those undergoing different ossiculoplasty methods, such as autologous ossicles, could be included. Extending the follow-up period would allow for better observation of patient prognosis, particularly in terms of vertigo and hearing improvement in Type II trauma patients.
Funding
This research is supported by the National Natural Science Foundation of China (Grant No. 82101227) and the Science and Technology Foundation of Guangzhou (Grant No. 2023A04J2091).
Competing Interests
The authors have declared that no competing interest exists.
References
1. Yetiser S, Hidir Y, Birkent H, Satar B, Durmaz A. Traumatic ossicular dislocations: etiology and management. Am J Otolaryngol. 2008;29:31-6
2. Han S, Yeo CD, Lee EJ. Two Cases of Multiple Ossicular Chain Disruption After Penetrating Injury and Tympanic Membrane Healing. J Audiol Otol. 2023;27:246-50
3. Meriot P, Veillon F, Garcia JF, Nonent M, Jezequel J, Bourjat P. et al. CT appearances of ossicular injuries. Radiographics. 1997;17:1445-54
4. Ghonim MR, Shabana YK, Ashraf B, Salem MA. Traumatic ossicular disruption with intact tympanic membrane: treatment modalities in 42 patients: Our experience. Clin Otolaryngol. 2016;41:176-9
5. Hough JV. Incudostapedial joint separation: etiology, treatment and significance. Laryngoscope. 1959;69:644-64
6. Deng M, Wang M, Zhang Q, Jiang B, Yan L, Bian Y. et al. Point-of-care ultrasound-guided submucosal paclitaxel injection in tracheal stenosis model. J Transl Int Med. 2023;11:70-80
7. Osetinsky LM, Hamilton GS 3rd, Carlson ML. Sport Injuries of the Ear and Temporal Bone. Clin Sports Med. 2017;36:315-35
8. Kim MS, Chung J, Kang JY, Choi JW. Transcanal endoscopic ear surgery for traumatic ossicular injury. Acta Otolaryngol. 2020;140:22-6
9. Delrue S, Verhaert N, Dinther JV, Zarowski A, Somers T, Desloovere C. et al. Surgical Management and Hearing Outcome of Traumatic Ossicular Injuries. J Int Adv Otol. 2016;12:231-6
10. Kreuzer PM, Landgrebe M, Vielsmeier V, Kleinjung T, De Ridder D, Langguth B. Trauma-associated tinnitus. J Head Trauma Rehabil. 2014;29:432-42
11. Deng Y, Wang H, Guo X, Jiang S, Cai J. Long-term blood pressure outcomes of laparoscopic adrenalectomy in trHTN patients. J Transl Int Med. 2023;11:275-81
12. Choe KS, Arigo J, Zeifer B. Stapediovestibular dislocation. Otol Neurotol. 2002;23:102-3
13. Tos M. Prognosis of hearing loss in temporal bone fractures. J Laryngol Otol. 1971;85:1147-59
14. Dou L, Lu E, Tian D, Li F, Deng L, Zhang Y. Adrenomedullin induces cisplatin chemoresistance in ovarian cancer through reprogramming of glucose metabolism. J Transl Int Med. 2023;11:169-77
15. E IR, Bakarozi M, Dimas I, Galanis K, Lygoura V, N KG. et al. Total and individual PBC-40 scores are reliable for the assessment of health-related quality of life in Greek patients with primary biliary cholangitis. J Transl Int Med. 2023;11:246-54
16. He Q, Li J. The evolution of folate supplementation - from one size for all to personalized, precision, poly-paths. J Transl Int Med. 2023;11:128-37
17. Singh A, Kaur M. Ossicular injury caused by a knitting needle. J Clin Diagn Res. 2013;7:3018-9
18. Li Y, Yao Z, Li Y, Yang Z, Li M, Chen Z. et al. Prognostic value of serum ammonia in critical patients with non-hepatic disease: A prospective, observational, multicenter study. J Transl Int Med. 2023;11:401-9
19. Hakuba N, Iwanaga M, Tanaka S, Hiratsuka Y, Kumabe Y, Konishi M. et al. Ear-pick injury as a traumatic ossicular damage in Japan. Eur Arch Otorhinolaryngol. 2010;267:1035-9
20. Hyug Choi J, Sook Jun M, Yong Jeon J, Kim HS, Kyung Kim Y, Ho Jeon C. et al. Global lineage evolution pattern of sars-cov-2 in Africa, America, Europe, and Asia: A comparative analysis of variant clusters and their relevance across continents. J Transl Int Med. 2023;11:410-22
21. Chen X, Wang M, Yu K, Xu S, Qiu P, Lyu Z. et al. Chronic stress-induced immune dysregulation in breast cancer: Implications of psychosocial factors. J Transl Int Med. 2023;11:226-33
22. Liu N, Li D, Liu D, Liu Y, Lei J. FOSL2 participates in renal fibrosis via SGK1-mediated epithelial-mesenchymal transition of proximal tubular epithelial cells. J Transl Int Med. 2023;11:294-308
23. Spector GJ, Pratt LL, Randall G. A clinical study of delayed reconstruction in ossicular fractures. Laryngoscope. 1973;83:837-51
24. Zhang L, Jiang B, Zhu N, Tao M, Jun Y, Chen X. et al. Mitotic checkpoint kinase Mps1/TTK predicts prognosis of colon cancer patients and regulates tumor proliferation and differentiation via PKCα/ERK1/2 and PI3K/Akt pathway. Med Oncol. 2019;37:5
25. Chien CY, Tai SY, Chan LP, Wang HM, Chang NC, Wang LF. et al. Predictive Factors and Audiometric Outcome Comparison Between Titanium Prosthesis and Autologous Incus in Traumatic Ossicular Injury. Ann Otol Rhinol Laryngol. 2024;133:30-6
26. Zhu Y, Chi J, Cai S, Liu S, Yuan J, Xu H. et al. High-dose remifentanil exacerbates myocardial ischemia-reperfusion injury through activation of calcium-sensing receptor-mediated pyroptosis. Int J Med Sci. 2023;20:1570-83
27. Goodhill V. Traumatic fistulae. J Laryngol Otol. 1980;94:123-8
28. Lee JM, Lee HJ. Traumatic Stapes Luxation into the Vestibule. Ear Nose Throat J. 2022: 1455613221106215.
29. Nakajima T, Motegi M, Yamamoto Y. Penetrating Trauma-Induced Perilymphatic Fistula: A Case Report and Literature Review. Cureus. 2023;15:e36106
30. Arragg FG, Paparella MM. TRAUMATIC FRACTURE OF THE STAPES. Laryngoscope. 1964;74:1329-32
31. Yu W, Qin X, Zhang Y, Qiu P, Wang L, Zha W. et al. Curcumin suppresses doxorubicin-induced cardiomyocyte pyroptosis via a PI3K/Akt/mTOR-dependent manner. Cardiovasc Diagn Ther. 2020;10:752-69
32. Yao YP, Yang PJ, Lee CY, Huang JY, Yang SF, Lin HY. Utilization of sodium-glucose cotransporter 2 inhibitors on dry eye disease severity in patients with type 2 diabetes mellitus. Int J Med Sci. 2023;20:1705-10
33. Zhu L, Duan W, Yang B, Wang L. Decreased miR-329-3p upregulates Adamts4 and Dnajb1 in mouse hepatic I/R injury in an age-independent manner. Int J Med Sci. 2023;20:1562-9
34. Sarac S, Cengel S, Sennaroglu L. Pneumolabyrinth following traumatic luxation of the stapes into the vestibule. Int J Pediatr Otorhinolaryngol. 2006;70:159-61
35. Shao Y, Zhao T, Zhang W, He J, Lu F, Cai Y. et al. Presence of the apolipoprotein E-ε4 allele is associated with an increased risk of sepsis progression. Sci Rep. 2020;10:15735
36. Hatano A, Rikitake M, Komori M, Irie T, Moriyama H. Traumatic perilymphatic fistula with the luxation of the stapes into the vestibule. Auris Nasus Larynx. 2009;36:474-8
37. Yamasoba T, Amagai N, Karino S. Traumatic luxation of the stapes into the vestibule. Otolaryngol Head Neck Surg. 2003;129:287-90
38. Wen L, Cao Y, Cheng Q, Li X, Pan L, Li L. et al. Objectively measured near work, outdoor exposure and myopia in children. Br J Ophthalmol. 2020;104:1542-7
39. Gao WL, Li XH, Dun XP, Jing XK, Yang K, Li YK. Grape Seed Proanthocyanidin Extract Ameliorates Streptozotocin-induced Cognitive and Synaptic Plasticity Deficits by Inhibiting Oxidative Stress and Preserving AKT and ERK Activities. Curr Med Sci. 2020;40:434-43
40. Chen L, Tian Q, Shi Z, Qiu Y, Lu Q, Liu C. Melatonin Alleviates Cardiac Function in Sepsis-Caused Myocarditis via Maintenance of Mitochondrial Function. Front Nutr. 2021;8:754235
41. Cao Y, Lan W, Wen L, Li X, Pan L, Wang X. et al. An effectiveness study of a wearable device (Clouclip) intervention in unhealthy visual behaviors among school-age children: A pilot study. Medicine (Baltimore). 2020;99:e17992
42. Chen L, Zhan CZ, Wang T, You H, Yao R. Curcumin Inhibits the Proliferation, Migration, Invasion, and Apoptosis of Diffuse Large B-Cell Lymphoma Cell Line by Regulating MiR-21/VHL Axis. Yonsei Med J. 2020;61:20-9
43. Cuny H, Bozon K, Kirk RB, Sheng DZ, Bröer S, Dunwoodie SL. Maternal heterozygosity of Slc6a19 causes metabolic perturbation and congenital NAD deficiency disorder in mice. Dis Model Mech. 2023;16:dmm049647
44. Huang Z, Yu P, Tang J. Characterization of Triple-Negative Breast Cancer MDA-MB-231 Cell Spheroid Model. Onco Targets Ther. 2020;13:5395-405
45. Tao J, Xue C, Wang X, Chen H, Liu Q, Jiang C. et al. GAS1 Promotes Ferroptosis of Liver Cells in Acetaminophen-Induced Acute Liver Failure. Int J Med Sci. 2023;20:1616-30
46. Wang L, Su X, Wang L, Luo J, Xiong Z, Leung GHD. et al. Identification of lncRNAs associated with uterine corpus endometrial cancer prognosis based on the competing endogenous RNA network. Int J Med Sci. 2023;20:1600-15
47. Ederies A, Yuen HW, Chen JM, Aviv RI, Symons SP. Traumatic stapes fracture with rotation and subluxation into the vestibule and pneumolabyrinth. Laryngoscope. 2009;119:1195-7
48. Ding L, Lu S, Zhou Y, Lyu D, Ouyang C, Ma Z. et al. The 3' Untranslated Region Protects the Heart from Angiotensin II-Induced Cardiac Dysfunction via AGGF1 Expression. Mol Ther. 2020;28:1119-32
49. Qin A, Yang D, Wang S, Dong L, Tan J, Tang Y. et al. Uric acid-based ratios for predicting renal failure in Chinese IgA nephropathy patients. Int J Med Sci. 2023;20:1584-91
50. Saldaña-Villa AK, Lara-Lemus R. The Structural Proteins of Membrane Rafts, Caveolins and Flotillins, in Lung Cancer: More Than Just Scaffold Elements. Int J Med Sci. 2023;20:1662-70
51. Amezcua López JA, García Morales E, Pérez-Rulfo Ibarra D, Solís Pacheco JR, Aguilar Uscanga BR. Effects of maternal toxic substance consumption during breastfeeding on lactic acid bacteria abundance and nutritional content. Int J Med Sci. 2023;20:1513-26
52. An N, Chen Z, Zhao P, Yin W. Extracellular Vesicles in Sepsis: Pathogenic Roles, Organ Damage, and Therapeutic Implications. Int J Med Sci. 2023;20:1722-31
53. Hidaka H, Miyazaki M, Kawase T, Kobayashi T. Traumatic pneumolabyrinth: air location and hearing outcome. Otol Neurotol. 2012;33:123-31
54. Jiang L, Chen T, Xiong L, Xu JH, Gong AY, Dai B. et al. Knockdown of m6A methyltransferase METTL3 in gastric cancer cells results in suppression of cell proliferation. Oncol Lett. 2020;20:2191-8
55. Lu Y, Lin Z, Wen L, Gao W, Pan L, Li X. et al. The Adaptation and Acceptance of Defocus Incorporated Multiple Segment Lens for Chinese Children. Am J Ophthalmol. 2020;211:207-16
56. Ayhan M, Cankaya AB. Custom-made Subperiosteal Implants: A Finite Element Analysis on Monoblock and Dual Implant Systems in Atrophic Maxilla. Int J Med Sci. 2023;20:1755-62
57. He T, Luo N, Kang J, Ling N, Zhang D. Use of metagenomic next-generation sequencing for diagnosis of peritonitis in end-stage liver disease. Int J Med Sci. 2023;20:1698-704
58. Huang S, Fu D, Wan Z, Huang Z, Li M, Li H. et al. DKK1 Ameliorates Myofibroblast Differentiation in Urethral Fibrosis in Vivo and in Vitro by Regulating the Canonical Wnt Pathway. Int J Med Sci. 2023;20:1631-43
59. Liang L, Liu Y, Wu X, Chen Y. Artesunate induces ferroptosis by inhibiting the nuclear localization of SREBP2 in myeloma cells. Int J Med Sci. 2023;20:1535-50
60. Liu Y, Lyu X, Tan S, Zhang X. Research Progress of Exosomal Non-Coding RNAs in Cardiac Remodeling. Int J Med Sci. 2023;20:1469-78
61. Peng X, Rao G, Li X, Tong N, Tian Y, Fu X. Preclinical models for Type 1 Diabetes Mellitus - A practical approach for research. Int J Med Sci. 2023;20:1644-61
62. Qi M, Yu J, Ping F, Xu L, Li W, Zhang H. et al. Tumor necrosis factor-alpha mediates the negative association between telomere length and kidney dysfunction. Int J Med Sci. 2023;20:1592-9
63. Peng Y, Wang Y, Zhou C, Mei W, Zeng C. PI3K/Akt/mTOR Pathway and Its Role in Cancer Therapeutics: Are We Making Headway? Front Oncol. 2022;12:819128
Author contact
![]() Corresponding author: Yongkang Ou, Ouyksysu.edu.cn.
Corresponding author: Yongkang Ou, Ouyksysu.edu.cn.

 Global reach, higher impact
Global reach, higher impact