Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(11):2208-2214. doi:10.7150/ijms.95395 This issue Cite
Research Paper
Patients with hidradenitis suppurativa are associated with risk of new-onset glaucoma: a propensity-score-matched cohort study
1. Department of Nursing & Tungs' Taichung MetroHarbor Hospital, Taiwan.
2. School of Medicine, Chung Shan Medical University, Taichung, Taiwan.
3. Department of Ophthalmology, China Medical University Hospital, Taichung, Taiwan.
4. School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan.
5. Department of Anatomy, School of Medicine, Chung Shan Medical University, Taichung, Taiwan
6. Department of Medical Education, Chung Shan Medical University Hospital, Taichung, Taiwan.
7. Evidence-based Medicine Center, Chung Shan Medical University Hospital, Taichung, Taiwan.
8. Library, Chung Shan Medical University Hospital, Taichung, Taiwan.
9. Department of Neurosurgery, Mackay Memorial Hospital, Taipei 10449, Taiwan.
10. Department of Medicine, Mackay Medical College, New Taipei City 25245, Taiwan.
11. Department and Graduate Institute of Business Administration, National Taiwan University, Taipei, Taiwan.
12. Department of Pharmacology, Chung Shan Medical University, Taichung, Taiwan.
13. Orthopedics Department, Chi-Mei Medical Center, Tainan, Taiwan.
Received 2024-2-16; Accepted 2024-7-31; Published 2024-8-13
Abstract
Background: Ocular comorbidities of hidradenitis suppurativa (HS) has been widely evaluated; however real-world evidence was scarce. Moreover, risk of glaucoma in HS patients remained unclear. This study aimed to evaluate the 5-year glaucoma risk in HS patients.
Methods: This retrospective cohort study used the TriNetX database covering 2005-2017. In total, 53,281 HS patients were propensity score matched 1:1 to controls based on demographics, including comorbidities, medications, healthcare utilization, etc. Patients were followed for 5 years post-index date. Glaucoma risks were calculated based on hazard ratios and 95% confidence intervals (95% CI). Stratified analyses by sex and age were performed.
Results: After matching, baseline characteristics were similar between groups. HS was associated with a 1.25 times higher 5-year glaucoma risk (95% CI, 1.10-1.42). The risk was significant within 1 year (HR=1.37; 95% CI, 1.03-1.82), 3 years (HR=1.31; 95% CI, 1.12-1.54), and 5 years post-index. In subgroup analysis, women had a 1.28 times higher risk (95% CI, 1.10-1.49). Patients aged 18-64 years (HR=1.33; 95% CI, 1.14-1.55) and ≥65 years (HR=1.33; 95% CI, 1.05-1.67) also presented elevated glaucoma risks.
Conclusion: This real-world data analysis demonstrated a significantly increased 5-year glaucoma risk in HS patients versus matched controls. Ocular complications should be concerned while managing HS patients.
Keywords: hidradenitis suppurativa, glaucoma, real-world study, electronic medical records
Introduction
Hidradenitis Suppurativa (HS), alternatively referred to as acne inversa and Verneuil's disease, represents a persistent inflammatory skin condition marked by recurring painful nodules, abscesses, and scarring. This condition predominantly affects areas rich in apocrine glands, including the axillae, breasts, groin, and perineum [1]. The considerable psychological and emotional burden [2], coupled with physical comorbidities, can adversely affect patients' quality of life. The repercussions of this can result in a decrease in general health and a reduction in the quality of life, further compounding the already substantial effects of the disease [3]. While the precise workings of HS remain partially understood, it is established that pro-inflammatory cytokines, such as tumor necrosis factor, IL-1β, and IL-17, are central to the progression of the illness [1].
Glaucoma is recognized as a complex and multifactorial progressive neurodegenerative disease characterized by a spectrum of clinical features, encompassing various risk factors and underlying mechanisms [4]. Globally, its prevalence has been estimated at 3 to 4 percent among people aged 40-80 years, with projections indicating a significant increase in the burden of the disease, affecting around 111.8 million individuals by 2040, particularly affecting populations in Asia and Africa [5]. This impending surge highlights the pressing need for a comprehensive understanding of the disease's origin and the formulation of effective treatments.
The prominent characteristics of glaucoma encompass degeneration of retinal ganglion cells (RGC), thinning of the retinal nerve fiber layer, and deformation of the optic disc [6]. Its development primarily involves a complex interplay between increased intraocular pressure, vascular irregularities, neurodegeneration, and chronic inflammation [7]. Neurodegeneration process can lead to a state described as para-inflammation, which denotes the adaptive reaction to detrimental stress or dysfunction. Intense para-inflammation can trigger the release of significant amounts of cytokines and chemokines, resulting in irreparable damage to the neural retina [4].
Although there is currently a lack of in-depth research exploring the relationship between HS and glaucoma, and glaucoma is seldom discussed as an ocular complication of HS [8, 9], both conditions are associated with mechanisms linked to inflammation. A recent study underscored the significant role of IL-38 in the immunopathology of chronic primary angle-closure glaucoma (CPACG) and HS [10, 11]. Consequently, this investigation focused specifically on evaluating the 5-year risk of glaucoma in patients with HS. The expected outcome of this research is to improve the understanding of the interplay between these two diseases by the medical community, offering a valuable reference for future clinical diagnosis and treatment.
Methods and Materials
This study was conducted retrospectively using de-identified data from the TriNetX research network, which is a global platform containing electronic medical records from over 120 healthcare organizations worldwide. The TriNetX collaborative network has been extensively used in previous studies to examine associations between exposures and outcomes [12-14]. In this study, we accessed the United States-based network (US collaborative network) containing records from 60 healthcare organizations and approximately 87 million patients for analysis. To extract the baseline information of study participants, we identified respective ICD-10-CM for diseases identification and RxNorm for medication records (Table S1). This study was approved by the Institutional Review Board of Tungs' Taichung MetroHarbor Hospital (IRB TTMHH No.: 112208N).
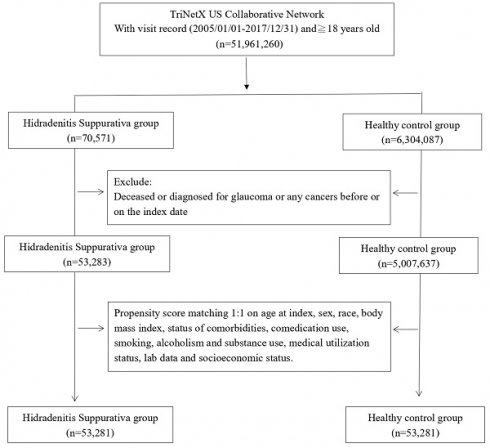
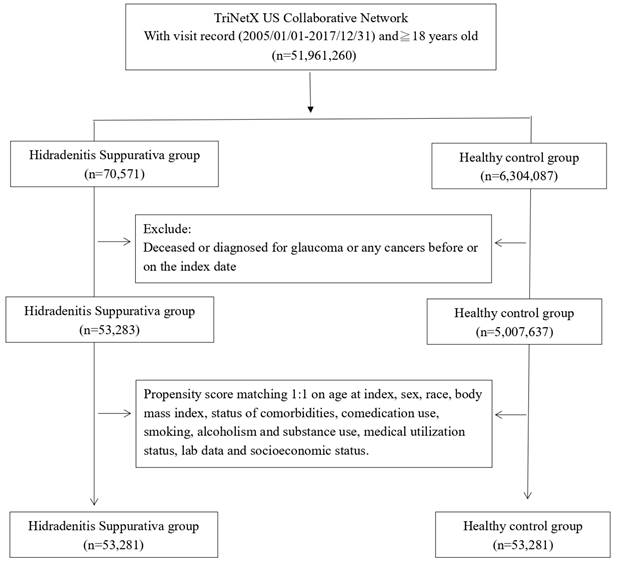
The study population was selected from the TriNetX network by identifying patients aged 18 years or older with a documented history of HS between January 1, 2005 and December 31, 2017. Each patient was followed for a minimum of 5 years after the initial recorded HS diagnosis date, which was defined as the index date. Patients were excluded if they were deceased before the index date, had any glaucoma diagnosis or had any cancer diagnosis prior to the index date. A healthy control cohort was constructed by selecting patients who had undergone general medical examination within the study timeframe. Propensity score matching at a 1:1 ratio was implemented to match the HS and control cohorts based on demographic and clinical characteristics, including age, gender, substance use, race, comorbidities, comedications, lab results, socioeconomic factors, and prior healthcare utilization. After matching, the final analytic sample consisted of 53,281 HS patients and 53,281 matched controls.
We performed stratified analyses by age and sex to evaluate the HS-outcome association across various populations. Sensitivity analyses were also conducted using various matching algorithms (including: Crude model without matching; Model 1: propensity score matching performed on age at index and sex; Model 2: Propensity score matching was performed on age at index, sex, race and comorbidities; Model 3: Propensity score matching was performed on age at index, sex, race, comedications and substance use; Model 4: Propensity score matching was performed on age at index, sex, race, body mass index, status of comorbidities, comedication use, smoking, alcoholism and substance use, medical utilization status, lab data regarding inflammation status, socioeconomic status, and the use of corticosteroids) and washout periods (6 months, 12 months and 24 months). All analyses were executed using the TriNetX system. Hazard ratios and 95% confidence intervals were calculated where applicable. Propensity score matching utilized greedy nearest neighbor matching with a 0.1 caliper width. Standardized differences above 0.1 were considered statistically significant when assessing matched baseline characteristics between cohorts.
Results
Some of the potential confounders, including age, sex, and socioeconomic issues, were significantly different between the HS group and controls. Before matching, people with HS were more likely to have comorbidities such as diabetes, migraine, and sleep apnea. Moreover, the ratio of substance uses and socioeconomic problems was also significantly higher in the HS group. After matching, differences between the two groups became insignificant (Table 1). In the current study, patients with HS were on average 33.6 years old and mostly white (44.7%).
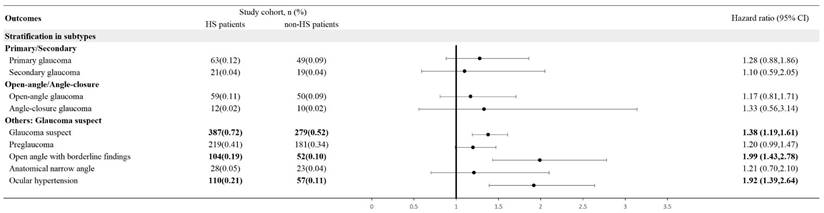
After matching on covariates, HS patients had a 37% higher risk of developing glaucoma in the first year after the index date compared to controls. The risk remained significantly elevated at 31% and 25% higher at 3 and 5 years after the index date (Table 2). Stratification analysis breaks down the risk by gender and age subgroups. Female HS patients had a statistically significant 28% higher risk of developing glaucoma within 5 years compared to female controls. However, the 5-year glaucoma risk for male HS patients was not significant compared to males without HS (HR, 1.21; 95% CI, 0.96, 1.52). Both young (18-64 years) and elderly (≥65 years) HS patients had around 30% higher risks of developing glaucoma within 5 years versus their age-matched controls (Table 3). In stratification based on subtypes, primary, secondary, open-angle and angle-closed glaucoma did not present statistically significant risk in HS patients. However, risk of glaucoma suspect (HR=1.38; 95% CI, 1.19-1.61), including ocular hypertension (HR=1.92; 95% CI, 1.39-2.64) and open angle with borderline findings (HR= 1.99; 95% CI, 1.43-2.78), were significantly increased in HS patients (Figure 2).
Using different propensity score matching variables, washout periods, HS patients consistently showed statistically significantly elevated hazards of developing glaucoma, with risks ranging from 19% to 90% higher than controls without HS (Table S2). While excluding all incident glaucoma occurring within 24 months after index date, the significance of HS-glaucoma association remained, with the HR of 1.23 (95% CI, 1.06,1.42) (Table S3).
Patient selection process.
Forest plot: stratification in subtypes of glaucoma. Legends: 95% CI, 95% confidence interval; HS, hidradenitis suppurativa.
Baseline characteristics of study subjects (before and after propensity score matching)
| Before matching | After matchinga | ||||||
|---|---|---|---|---|---|---|---|
| HS cohort (n=53,283) | Control cohort (n= 5,007,637) | Std diff | HS cohort (n=53,281) | Control cohort (n=53,281) | Std diff | ||
| Age at index | |||||||
| Mean ± SD | 33.6±14.1 | 37.8±20.7 | 0.23 | 33.6±14.1 | 34.2±14.7 | 0.04 | |
| Sex | |||||||
| Male | 13347 (25.0) | 2163477 (43.2) | 0.39 | 13347 (25.1) | 13376 (25.1) | 0.00 | |
| Female | 39555 (74.2) | 2756615 (55.0) | 0.41 | 39553 (74.2) | 39501 (74.1) | 0.00 | |
| Race, n (%) | |||||||
| White | 23835 (44.7) | 3031232 (60.5) | 0.32 | 23835 (44.7) | 23832 (44.7) | 0.00 | |
| Black or African American | 18601 (34.9) | 746722 (14.9) | 0.48 | 18599 (34.9) | 18854 (35.4) | 0.01 | |
| Asian | 852 (1.6) | 172463 (3.4) | 0.12 | 852 (1.6) | 1523 (2.9) | 0.09 | |
| American Indian or Alaska Native | 239 (0.4) | 16275 (0.3) | 0.02 | 239 (0.4) | 197 (0.4) | 0.01 | |
| Socioeconomic status | |||||||
| Socioeconomic/psychosocial circumstances problem | 1020 (1.9) | 35043 (0.7) | 0.11 | 1019 (1.9) | 920 (1.7) | 0.01 | |
| Lifestyle | |||||||
| Alcohol dependence, smoking and substance use | 6320 (11.9) | 161468 (3.2) | 0.33 | 6318 (11.9) | 6441 (12.1) | 0.01 | |
| Comorbidities | |||||||
| Hypertension | 6673 (12.5) | 488193 (9.7) | 0.09 | 6673 (12.5) | 6807 (12.8) | 0.01 | |
| Diabetes mellitus | 3897 (7.3) | 202434 (4.0) | 0.14 | 3896 (7.3) | 3902 (7.3) | 0.00 | |
| Hyperlipidemia | 3524 (6.6) | 321210 (6.4) | 0.01 | 3524 (6.6) | 3419 (6.4) | 0.01 | |
| Migraine | 2392 (4.5) | 82403 (1.6) | 0.17 | 2392 (4.5) | 1979 (3.7) | 0.04 | |
| Sleep apnea | 2179 (4.1) | 76427 (1.5) | 0.16 | 2178 (4.1) | 2151 (4.0) | 0.00 | |
| Medications | |||||||
| Promethazine | 3939 (7.4) | 145044 (2.9) | 0.20 | 3937 (7.4) | 3958 (7.4) | 0.00 | |
| Ipratropium | 1702 (3.2) | 63227 (1.3) | 0.13 | 1702 (3.2) | 1635 (3.1) | 0.01 | |
| Phenylephrine | 1019 (1.9) | 45038 (0.9) | 0.09 | 1018 (1.9) | 913 (1.7) | 0.01 | |
| Ephedrine | 733 (1.4) | 28616 (0.6) | 0.08 | 732 (1.4) | 608 (1.1) | 0.02 | |
| Medical Utilization Status | |||||||
| Ambulatory visit | 29843 (56.0) | 2320931 (46.3) | 0.19 | 29841 (56.0) | 29989 (56.3) | 0.01 | |
| Inpatient visit | 8750 (16.4) | 536300 (10.7) | 0.17 | 8749 (16.4) | 8723 (16.4) | 0.00 | |
| Laboratory data | |||||||
| BMI, n (%) | |||||||
| ≥ 35 (kg/m2) | 4182 (7.8) | 103063 (2.1) | 0.27 | 4180 (7.8) | 4315 (8.1) | 0.01 | |
| C reactive protein, n (%) | |||||||
| ≥ 3 (mg/L) | 2172 (4.1) | 73078 (1.5) | 0.16 | 2171 (4.1) | 2162 (4.1) | 0.00 | |
HS: Hidradenitis Suppurativa; BMI, body mass index; SD, standardized difference
a Propensity score matching was performed on age at index, sex, race, body mass index, status of comorbidities (including diabetes mellitus, hypertension, hyperlipidemia, migraines, sleep apnea), status of comedication use (phenylephrine, ephedrine, promethazine, ipratropium bromide), status of smoking, alcoholism and substance use, medical utilization status, lab data regarding inflammation status (CRP) and socioeconomic status.
Risk of glaucoma under different follow-up timea
| Outcomes | Hazard ratio (95% Confidence interval)b | ||
|---|---|---|---|
| 1 year | 3 years | 5 years | |
| Glaucoma | 1.37 (1.03, 1.82) | 1.31 (1.12, 1.54) | 1.25 (1.10, 1.42) |
HS: hidradenitis suppurativa
aData present here were the value of follow up from 90 days after index date to the respective following up years.
b Propensity score matching was performed on age at index, sex, race, body mass index, status of comorbidities (including diabetes mellitus, hypertension, hyperlipidemia, migraines, sleep apnea), status of comedication use (phenylephrine, ephedrine, promethazine, ipratropium bromide), status of smoking, alcoholism and substance use, medical utilization status, lab data regarding inflammation status (CRP) and socioeconomic status.
Stratification analysis of glaucoma risk in HS patients
| Cases occurring new-onset glaucoma | |||
|---|---|---|---|
| Subgroups | HS cohort (No. of event/ HS patient amount in each subgroup) | Control cohort (No. of event/ non-HS patient amount in each subgroup) | HR (95% CI)a |
| Gender | |||
| Male | 159/13345 | 132/13345 | 1.21 (0.96,1.52) |
| Female | 383/39373 | 296/39373 | 1.28 (1.10,1.49) |
| Age at index date | |||
| 18-64 years old | 382/48325 | 283/48325 | 1.33 (1.14,1.55) |
| ≥ 65 years old | 164/4953 | 126/4953 | 1.33 (1.05,1.67) |
a Propensity score matching was performed on age at index, sex, race, body mass index, status of comorbidities (including diabetes mellitus, hypertension, hyperlipidemia, migraines, sleep apnea), status of comedication use (phenylephrine, ephedrine, promethazine, ipratropium bromide), status of smoking, alcoholism and substance use, medical utilization status, lab data regarding inflammation status (CRP) and socioeconomic status.
Discussion
Utilizing a global-federated, large-scale electronic medical records database, we observed that people with HS were associated with high risk of developing glaucoma, with the HR of 1.25 (95% CI, 1.10,1.42) in five-year follow up. The current study provided real-world evidence based on adjustment in critical covariates, and could serve as potential references for clinicians while managing HS patients with risk of ophthalmologic comorbidities. Several studies have previously suggested a strong relationship between HS and various inflammatory diseases [15-17]. However, the possible association between HS and glaucoma is still unclear. Our study provides robust data, aiming to fill the evidence gap in this field.
HS is characterized by numerus comorbidities, including cardiovascular and renal disease, endocrine dysfunction, and a series of immune-mediated diseases [18]. Pathogenesis of HS is associated with dysregulation of immune system. Hyperkeratosis of infundibular epithelium causes propagation of bacteria. This activates macrophages to secrete pro-inflammatory factors. IL-12 and IL-23 produced by macrophages stimulate TH1 and TH17 cells, which leads to strengthen the positive feedback of immune system. Due to bacterial propagation and immune dysregulation, follicle might be ruptured, which increases immune cell infiltration [19]. This facilitates the elevation of IL-36γ from keratinocytes [20]. A study indicated that IL-36γ induces G-CSF, a potential factor associated with HS lesions [21]. Another study showed an elevation of IL-36α, IL-36β, IL-36γ and IL-36Ra in HS lesioned area, while IL-38 is increasing in both perilesional and lesioned area [22]. Therefore, IL-36 and IL-38 play a crucial role in pathogenesis of HS.
Glaucoma is known to be a chronic eye disease, characterized by retinal ganglion cell atrophy with corresponding vision loss. Glaucoma can be categorized into various types, with primary open-angle glaucoma and primary angle-closure glaucoma being the two most prevalent forms. The pathogenesis of glaucoma is not well-established, involving intraocular pressure elevation, abnormal structural defect and blood flow, immune dysregulation, and low intracranial pressure [23]. A recent study reveals potential correlation between IL-36, IL-37, IL-38, and chronic primary angle closure glaucoma (CPACG). Significant elevation of IL-36, IL-37 and IL-38 was detected in CPACG groups compared to age-related cataracts [24]. IL-36 is commonly seen in various acute and chronic inflammatory disease, including skin, eye, kidney, liver, intestinal inflammation [25, 26]. IL-38 is a potential anti-inflammatory cytokine, with extensive biological activity. It commonly involves in IL-1, IL-36 and TLR receptor pathway [27].
From pathogenesis of HS and glaucoma, it is evident that HS and glaucoma share a common mechanism involving IL-36 and IL-38 elevation. IL-36 is traditionally considered to be produced in various cells including keratinocytes, with fewer evidence related to eye structure [26]. However, recent studies provide a novel insight into IL-36 as a potential factor to immune-mediated eye disease [24, 28]. Therefore, dysregulation of IL-36-mediated immune pathway might be a possible factor for both HS and glaucoma.
Systemic inflammation in HS patients causes local upregulation of IL-36 and dysregulation of IL-38, which potentially leads to immune-mediated glaucoma. Under such circumstance, the use of steroid could serve as a potential confounding factor given that steroid use is related to glaucoma. However, as presented in the model 4 of Table S2, after adding steroid use as covariates for matching, the HS-glaucoma association remained. However, the definite mechanism of IL-36 and IL-38 in both HS and glaucoma is still unclear. Though IL-36 and IL-38 are elevated in both HS and CPACG, the observed association may be a result of chronic inflammation in both diseases. Further investigations are needed to provide conclusive evidence.
In addition, the HS-glaucoma association may potentially be affected by different sex groups. In our study, female HS patients had a higher risk than controls, while the risk of male patients was not significant compared to controls group. Females are considered one of the risk factors of glaucoma, and HS is also seemed to be female-predominant. Given the mechanisms and epidemiology of two diseases, we hypothesized that females may encounter a stronger inflammatory response, which elevates more IL-36 and IL-38 and in turn enhanced the risk of new-onset glaucoma. On the contrary, male patients may lack of enough responses, leading to absence of HS-glaucoma association.
Several limitations should be noted in our study. Firstly, due to the retrospective nature of this study, the causation of the observed association could not be established. Secondly, due to limitation of data, the definition of subtypes of glaucoma could be limited to misclassification bias as the definition was given based on administrative codes. Likewise, the data of HS patients' disease severity and treatment history were unavailable. As a result, we were incapable of assessing the influence of different HS stages on glaucoma. Third, in observational studies, issue of confounding bias should be prudently interpreted though propensity score matching has been performed [29, 30]. Residual confounding bias may exist with possibility to affect our outcome. Consequently, the results of our study should be interpreted cautiously. Fourth, although stratified analyses and propensity score matching were performed on age at index, sex, race, and other factors of cohorts and controls in the current study, as in previous studies utilizing the US collaborative network in the TriNetX system [31], the generalizability to populations outside the United States may be limited and should be considered with caution. Given that previous studies have shown racial disparities in the epidemiology and pathophysiology of glaucoma, particularly the higher prevalence in Black and Hispanic populations [32], future studies should consider potential differences in the observed association between HS and glaucoma and focus on the effects of genetic variants and the diversity of living environments.
To sum up, our findings indicate an elevated risk of glaucoma in individuals with HS across various follow-up periods. This underscores the importance for clinicians to be mindful of ophthalmic comorbidities in HS patients when providing medical care. Glaucoma can negatively impact patients' quality of life [33]. Early glaucoma screening could potentially reduce the comorbidity burden of HS patients, thereby preventing impairment in their quality of life. In this case, the clinical implication of our current study's findings is that we provide clinicians with real-world evidence regarding the early detection of ophthalmology-related comorbidities. Clinicians could integrate our findings into clinical practice, promote the collection of glaucoma-related family history, and result in the early detection of new-onset glaucoma. Current evidence could potentially serve as a basis for future comorbidity screening guidelines for HS.
Supplementary Material
Supplementary tables.
Acknowledgements
Author contributions
All the authors involved in drafting or revising the article and approved of the submitted version.
Study conception and design: Li CP, Lin CY, Lu HY, Chen SN, Chen SJ, Tsai RY, Chang HC, Gau SY
Data acquisition: Gau SY, Chang HC, Li CP
Data analysis and demonstration: Gau SY, Chang HC, Li CP, Chen SN, Chen SJ
Original draft preparation: Li CP, Lin CY, Lu HY, Chen SN, Chen SJ, Tsai RY, Chang HC, Gau SY
Statement of ethics
This study was approved by the Institutional Review Board of Tungs' Taichung MetroHarbor Hospital (IRB TTMHH No.: 112208N). Informed consent was exempted by the IRB.
Data sharing statement
Data in this study were retrieved from TriNetX Research Network. All data available in the database were administrated by the TriNetX platform. Detailed information can be retrieved at the official website of the research network (https://trinetx.com).
Competing Interests
The authors have declared that no competing interest exists.
References
1. Sabat R, Jemec GBE, Matusiak Ł, Kimball AB, Prens E, Wolk K. Hidradenitis suppurativa. Nat Rev Dis Primers. 2020;6:18
2. Jfri A, Netchiporouk E, Raymond K, Litvinov IV, O'Brien E. Association of clinical severity scores with psychosocial impact in patients with hidradenitis suppurativa. J Am Acad Dermatol. 2021;84:1712-5
3. Garg A, Malviya N, Strunk A, Wright S, Alavi A, Alhusayen R. et al. Comorbidity screening in hidradenitis suppurativa: Evidence-based recommendations from the US and Canadian Hidradenitis Suppurativa Foundations. J Am Acad Dermatol. 2022;86:1092-101
4. Baudouin C, Kolko M, Melik-Parsadaniantz S, Messmer EM. Inflammation in Glaucoma: From the back to the front of the eye, and beyond. Prog Retin Eye Res. 2021;83:100916
5. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081-90
6. Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. Jama. 2014;311:1901-11
7. Schuster AK, Erb C, Hoffmann EM, Dietlein T, Pfeiffer N. The Diagnosis and Treatment of Glaucoma. Dtsch Arztebl Int. 2020;117:225-34
8. Saygın D, Syed AU, Lowder CY, Srivastava S, Maya JJ, Hajj-Ali RA. Characteristics of inflammatory eye disease associated with hidradenitis suppurativa. Eur J Rheumatol. 2018;5:165-8
9. Lee DJ, Desai S, Laurent E, Kopplin LJ. Characterization and Management of Inflammatory Eye Disease in Patients with Hidradenitis Suppurativa. Ocul Immunol Inflamm. 2021;29:1318-23
10. Xie L, Huang Z, Li H, Liu X, Zheng S, Su W. IL-38: A New Player in Inflammatory Autoimmune Disorders. Biomolecules. 2019;9:345
11. Esmaeilzadeh A, Bahmaie N, Nouri E, Hajkazemi MJ, Zareh Rafie M. Immunobiological Properties and Clinical Applications of Interleukin-38 for Immune-Mediated Disorders: A Systematic Review Study. Int J Mol Sci. 2021;22:12552
12. Yong SB, Gau SY, Li CJ, Tseng CW, Wang SI, Wei JCC. Associations between COVID-19 outcomes and asthmatic patients with inhaled corticosteroid. Front Pharmacol. 2023;14:1204297
13. Chang H-C, Lin C-Y, Guo Y-C, Lu H-Y, Lee C-Y, Wu M-C. et al. Association between hidradenitis suppurativa and atopic diseases: a multi-center, propensity-score-matched cohort study. International Journal of Medical Sciences. 2024;21:299-305
14. Chang H-C, Wu C-L, Chiu T-M, Liao W-C, Gau S-Y. Risk of osteoarthritis in patients with hidradenitis suppurativa: a global federated health network analysis. Frontiers in Immunology. 2023;14:1285560
15. Gau SY, Chan WL, Tsai JD. Risk of Atopic Diseases in Patients with Hidradenitis Suppurativa: A Systematic Review and Meta-Analysis of Observational Studies. Dermatology. 2023;239:314-22
16. Gau SY, Hsiao YP, Liao WC, Ma KS, Wu MC. Risk of liver dysfunction and non-alcoholic fatty liver diseases in people with hidradenitis suppurativa: A systematic review and meta-analysis of real-world evidences. Front Immunol. 2022;13:959691
17. Gau SY, Preclaro IAC, Wei JC, Lee CY, Kuan YH, Hsiao YP. et al. Risk of psoriasis in people with hidradenitis suppurativa: A systematic review and meta-analysis. Front Immunol. 2022;13:1033844
18. Nguyen TV, Damiani G, Orenstein LAV, Hamzavi I, Jemec GB. Hidradenitis suppurativa: an update on epidemiology, phenotypes, diagnosis, pathogenesis, comorbidities and quality of life. J Eur Acad Dermatol Venereol. 2021;35:50-61
19. Sabat R, Jemec GBE, Matusiak L, Kimball AB, Prens E, Wolk K. Hidradenitis suppurativa. Nat Rev Dis Primers. 2020;6:18
20. Sachen KL, Arnold Greving CN, Towne JE. Role of IL-36 cytokines in psoriasis and other inflammatory skin conditions. Cytokine. 2022;156:155897
21. Wolk K, Brembach TC, Simaite D, Bartnik E, Cucinotta S, Pokrywka A. et al. Activity and components of the granulocyte colony-stimulating factor pathway in hidradenitis suppurativa. Br J Dermatol. 2021;185:164-76
22. Hessam S, Sand M, Gambichler T, Skrygan M, Ruddel I, Bechara FG. Interleukin-36 in hidradenitis suppurativa: evidence for a distinctive proinflammatory role and a key factor in the development of an inflammatory loop. Br J Dermatol. 2018;178:761-7
23. Kang JM, Tanna AP. Glaucoma. Med Clin North Am. 2021;105:493-510
24. Zhang JL, Song XY, Chen YY, Nguyen THA, Zhang JY, Bao SS. et al. Novel inflammatory cytokines (IL-36, 37, 38) in the aqueous humor from patients with chronic primary angle closure glaucoma. Int Immunopharmacol. 2019;71:164-8
25. Neurath MF. IL-36 in chronic inflammation and cancer. Cytokine Growth Factor Rev. 2020;55:70-9
26. Elias M, Zhao S, Le HT, Wang J, Neurath MF, Neufert C. et al. IL-36 in chronic inflammation and fibrosis - bridging the gap? J Clin Invest. 2021;131:e144336
27. Garraud T, Harel M, Boutet MA, Le Goff B, Blanchard F. The enigmatic role of IL-38 in inflammatory diseases. Cytokine Growth Factor Rev. 2018;39:26-35
28. Li JM, Lu R, Zhang Y, Lin J, Hua X, Pflugfelder SC. et al. IL-36alpha/IL-36RA/IL-38 signaling mediates inflammation and barrier disruption in human corneal epithelial cells under hyperosmotic stress. Ocul Surf. 2021;22:163-71
29. Huang KH, Lee CH, Cheng YD, Gau SY, Tsai TH, Chung NJ. et al. Correlation between long-term use of metformin and incidence of NAFLD among patients with type 2 diabetes mellitus: A real-world cohort study. Front Endocrinol (Lausanne). 2022;13:1027484
30. Huang SC, Gau SY, Huang JY, Wu WJ, Wei JC. Increased Risk of Hypothyroidism in People with Asthma: Evidence from a Real-World Population-Based Study. J Clin Med. 2022;11:2776
31. Li CP, Lo SW, Tsai RY, Chang HC, Gau SY. New-Onset Hidradenitis Suppurativa in Psoriasis Patients: A Multi-Center, Retrospective Cohort Study. Life (Basel, Switzerland). 2024 14
32. Siegfried CJ, Shui YB. Racial Disparities in Glaucoma: From Epidemiology to Pathophysiology. Missouri medicine. 2022;119:49-54
33. Montana CL, Bhorade AM. Glaucoma and quality of life: fall and driving risk. Current opinion in ophthalmology. 2018;29:135-40
Author contact
![]() Corresponding author: Shiu-Jau Chen, MD, PhD. Department of Neurosurgery, Mackay Memorial Hospital, Taipei, Taiwan. No. 92, Sec. 2, Zhongshan N. Rd., Zhongshan Dist., Taipei City, 104217, Taiwan. Tel.: 886 2 26360303; Email: Chenshiujaucom.
Corresponding author: Shiu-Jau Chen, MD, PhD. Department of Neurosurgery, Mackay Memorial Hospital, Taipei, Taiwan. No. 92, Sec. 2, Zhongshan N. Rd., Zhongshan Dist., Taipei City, 104217, Taiwan. Tel.: 886 2 26360303; Email: Chenshiujaucom.

 Global reach, higher impact
Global reach, higher impact