3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(11):2031-2039. doi:10.7150/ijms.96269 This issue Cite
Research Paper
Effects of different levels of physical activity on arterial stiffness and physical fitness performance in firefighters
1. Graduate Institute of Sports Science, National Taiwan Sport University, Taoyuan City, Taiwan.
2. Shulin Branch Fifth Corps, Fire Department, New Taipei City Government, New Taipei City, Taiwan.
Received 2024-3-14; Accepted 2024-7-18; Published 2024-8-1
Abstract
Background: Firefighters have lower levels of physical activity while on call. It is critical to understand the impact of firefighters' physical activity on arterial stiffness. This study classified groups by physical activity level and combined peripheral vascular monitor measurement to explore the relationships between the level of physical activity and cardiovascular (CV) risk and physical fitness (PF) of firefighters, as well as the acute response to arterial stiffness (AS) following maximal aerobic exercise test (MAET) intervention.
Methods: The International Physical Activity Questionnaire (IPAQ) was used to classify the participants into 3 groups: low, moderate, and high level of physical activity group, respectively. A total of 36 participants were recruited, 12 in each group. Participants were assessed for body composition, rest brachial-ankle pulse wave velocity (baPWV), handgrip strength (HGS), maximal oxygen uptake (V̇O2max), and MAET baPWV.
Results: In the three groups, significant differences were observed in V̇O2max, HGS, relative fat mass (%FM), body mass index (BMI), muscle mass ratio (MMR), and Rest baPWV (p < 0.05). After maximal aerobic exercise, the MAET baPWV values decreased significantly in all groups (all p < 0.001). Rest baPWV was significantly correlated with firefighters' age, seniority, metabolic equivalents (METs), height and muscle mass (MM) (p < 0.05).
Conclusions: Firefighters with high levels of physical activity had better body composition and physical fitness and lower Rest baPWV. In all three groups, baPWV was lower after the MAET than before it. Therefore, regardless of a firefighter's level of physical activity, high-intensity aerobic exercise may have a beneficial effect on arterial stiffness.
Keywords: firefighter, arteriosclerosis, body composition, physical training
Introduction
Firefighters encounter many dangerous conditions during their professional duties and must maintain physical standards to improve occupational safety and performance [1]. Sufficient physical fitness improves the likelihood firefighters will successfully complete occupational tasks despite the constraints imposed by protective equipment (e.g., external firefighting gear, breathing apparatus) and the environment (e.g., increased temperature, smoke, carbon dioxide). Firefighting leads to significant cardiovascular strain, including alterations in cardiac function, vascular function, and hemostasis [2], leading to the danger of irreparable harm to the health of firefighters. A worrying situation is the high rate of overweight (BMI: 25.0-29.9 kg/m2) and obesity (BMI: ≥30.0 kg/m2) among firefighters, in which unsatisfactory physical fitness and obesity are associated with impaired work performance, increased risk of injury and duty-related sudden cardiac events [3-6].
Significant increases in the prevalence of overweight and obesity have been observed among firefighters in the United States, United Kingdom, and other developed countries, and many firefighters have also been noted to have one or more cardiovascular risk factors (such as obesity, hypertension, hyperlipidemia) and reduced aerobic capacity [7]. However, according to a survey by the National Fire Protection Association (NFPA), less than 25% of US firefighters meet the amount of exercise recommended by the American College of Sports Medicine (ACSM) [8-10]. According to the BMI data, approximately 50% of firefighters are overweight and 25% are obese [11, 12]. Despite this, most fire agencies nationwide do not have routine, long-term physical training plans [11, 12]. One of the main factors contributing to firefighters' obesity is their low levels of physical activity. Infrequent and non-occupational physical activity is limited (e.g., off the clock recreation, transportation, household) and may explain the observed BMI classifications [13].
Poor cardiorespiratory fitness (V̇O2max below age-sex-matched inactive levels) [14, 15] and a low physical activity (less than 3 days of moderate/vigorous intensity activity per week) [16] have been identified as determinants of increased arterial stiffness [17]. There is a similar association between sedentary physical activity and arteriosclerosis, and 13.4% of sedentary firefighters suffer from metabolic syndrome, which entails a higher risk of cardiovascular disease (CVD) factors in arteriosclerosis [18].
Sudden and intense physical exertion has been shown to trigger sudden cardiovascular events, especially in sedentary individuals [19, 20]. Sudden cardiovascular events account for 45% of all firefighter deaths [21]. In the past decade, prevention and response mechanisms have been actively used to reduce the occurrence of sudden cardiac death among firefighters, but it is still the number one killer of firefighters in the United States [21]. The level of physical activity and cardiorespiratory fitness are inversely related to future CVD incidence; however, each additional metabolic equivalent of aerobic exercise may reduce the risk of mortality by 13% and CVD mortality by 15% [22].
The European Society of Cardiology guidelines for the management of pulse wave velocity (PWV) is the gold standard for the assessment of arteriosclerosis and can be used as an indicator of vascular damage, vascular compliance, and treatment effect [23, 24]. Carotid-femoral PWV (cfPWV) [25] and brachial-ankle PWV (baPWV) [26] are the two most frequently applied PWV measurements. As a velocity, PWV can be conveniently measured as the distance divided by the time interval between two selected points of the arterial system [27]. To measure cfPWV which is central arterial stiffness (carotid and femoral arteries), requires great skill and takes more than 20 minutes [28]. A simpler method to determine baPWV which is peripheral arterial stiffness (brachial and ankle arteries) was developed in Japan, and the use of this procedure became widespread within a short time [28]. Considering the unique work characteristics of firefighters and their health monitoring needs, the baPWV measurement method is more feasible. This technology is convenient, cost-effective, and suitable for rapid screening in various settings. Therefore, it is reasonable to support the current practice of using baPWV for monitoring the health of firefighters. A possible indicator of hardening blood vessels is baPWV greater than 1400 cm/s [26].
To our knowledge, there is currently a lack of relevant data on the impact of on-duty and off-duty physical activities (e.g., occupational, recreational, transportation, household, and exercise/leisure activities) and cardiopulmonary function on arterial stiffness in firefighters in Taiwan, and the degree of change in arterial stiffness (i.e. baPWV) after maximum intensity exercise also needs to be confirmed. Maximal intensity exercise directly impacts arteriosclerosis and blood vessel stiffness. By measuring baPWV before and after exercise, the immediate effects on vascular health can be assessed, which is particularly important for firefighters [29] or non-firefighters such as athletes [30]. Therefore, this study aims to determine the relationships between the level of physical activity and arterial stiffness, between the level of physical activity and physical fitness performance, and between arterial stiffness and physical fitness performance in firefighters. We hypothesize that firefighters' levels of physical activity would associate with arterial stiffness and overall physical fitness, and that maximal intensity exercise will alter their arterial stiffness.
Methods
Study design
In this study, firefighters from different departments in northern Taiwan urban were grouped into three groups by level of physical activity, which according to the total physical activity volume reported on the International Physical Activity Questionnaire (IPAQ), using metabolic equivalents (METs) as the cut-off point [16]. In order to reduce participants' self-report bias, the same experimenter assisted all participants in completing the IPAQ by explaining each question. The three groups were the low level of physical activity (LPAL, <600 MET-min/week), moderate level of physical activity (MPAL, 600-3,000 MET-min/week), and high level of physical activity groups (HPAL, >3,000 MET-min/week) [16]. An arteriosclerosis tester (OMRON HBP-8000, Omron Healthcare Co., Ltd, Kyoto, Japan) was used to investigate differences in arterial stiffness among firefighters with different levels of physical activity and the effects following maximal intensity exercise.
Participants
A total of 36 male firefighters (12 per group) who had passed the national examination and had been trained for more than one year voluntarily participated in this study. Participants were eligible if they were currently in active service and between 20 and 49 years of age. Participants were included if not on cardiovascular acting drugs. Exclusion criteria were those who had any cardiovascular disease or chronic disease diagnosed by a medical doctor, or smoker who smoked at least one cigarette per day. The participants could eat or drink 2 hours before the test, but they must avoid high-intensity exercise, caffeine and alcohol consumption in the 12 hours preceding the test. Sufficient sleep (≥ 7 hours) [31] is required the night before the test. The participants were not allowed to take any cardiovascular acting drugs. The sample size was estimated with a software program (G*Power v3.1.9.7; Heinrich-Heine-Universität Dusseldorf) with an effect size of 0.5, alpha error of 0.05, and statistical power of 0.8. Thus, the total sample size of participants required for the study was determined to be 33 (i.e., at least 11 participants per group). Before any experimental testing began, all participants completed informed consent.
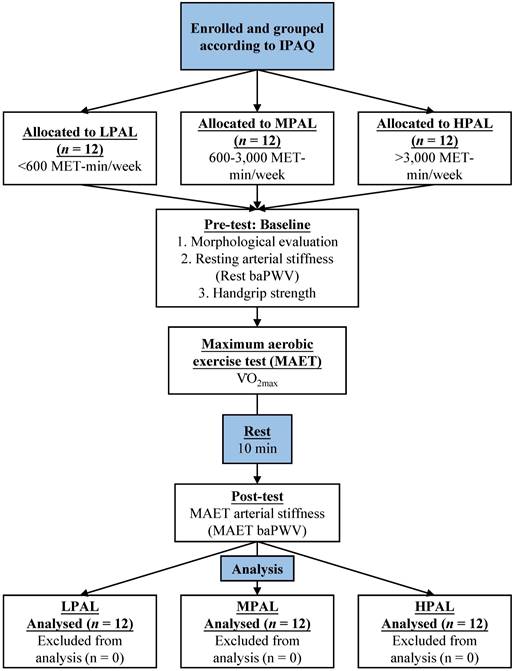
Procedures
After the morphological evaluations, all participants were assessed for resting arterial stiffness, handgrip strength, maximum aerobic exercise test (MAET), and post-MAET arterial stiffness after 10 minutes of rest. The flow design of the study is shown in Fig. 1.
Experimental procedure description.
Morphological evaluation
Morphological evaluations were assessed through standard procedures [32, 33]. The weight, body mass index (BMI), relative fat mass (%FM), muscle mass (MM), and muscle mass ratio (MMR) of all participants were measured using a body composition analyzer (InBody 570, Biospace, Inc. Seoul, Korea), with additional inputs of their age and height measured by the height measurement equipment H900 (NAGATA Scale Co., Ltd. Tainan, Taiwan). The InBody® 570 serves as a reliable method to estimate body composition with a multi-frequency bioelectrical impedance analyzer [32].
Rest and post-MAET arterial stiffness testing
The data on baPWV were measured with an arteriosclerosis tester (OMRON HBP-8000, Omron Healthcare Co., Ltd, Kyoto, Japan) which with high reliability (ICC greater than 0.95) [34]. The measurement of baPWV was performed by a trained examiner. The room temperature of the testing room was maintained at 22-25°C. Participants wore light short-sleeved sportswear and rested for > 5 minutes in a supine position on the massage table, and they were instructed to keep their bodies relaxed [35]. Then the participants were asked to turn both palms upward by their sides. Four blood pressure cuffs were tied to the upper arms and ankles respectively, in accordance with established methods [35]. The average values of the baPWV on the left and right sides was calculated [35]. Two measurements were taken and if these values deviated by >5 mmHg, a third measurement was performed. The average of the two closest values was used [36].
Participants laid supine to passively rest for 10 minutes immediately following the MAET [37]. Then, the examiner performed the same arterial stiffness test process again [35]. For each measurement taken, the average baPWV on the left and right sides was calculated.
Maximum handgrip strength (HGS) testing of dominant hand
A Takei 5401 handgrip digital dynamometer (Takei Scientific Instruments Co., Ltd, Tokyo, Japan) was used for HGS measurement. Participants stood in a standing position with their elbows straight and relaxed. When they heard the start command, they exerted maximum force for at least 3 seconds until the value on the handgrip strength indicator stopped increasing [37]. The highest value of three measurements was taken as the final result.
Maximal aerobic exercise test (MAET)
MAET was performed with the Cardiopulmonary Exercise Testing System (Vmax Encore 29 System, VIASYS Healthcare Inc, Yorba Linda, CA, USA). Before each test, the instrument was warmed up for at least 15 minutes before being calibrated. Participants wore a face mask (Hans-Rudolph) that covered their noses and mouths and a chest strap heart rate monitor (Polar H10, Polar Electro Oy, Finland). The initial speed of the treadmill was set at 7.2 km/h, and the speed increased by 1.8 km/h every 2 minutes until the participant was exhausted [39]. Rate of Perceived Exertion (RPE) was evaluated every 2 minutes using a 6-20 category-ratio scale [40]. The test was completed when the participants reached volitional exhaustion or met at least three of the following criteria [41, 42]: 1) peak heart rate greater than 90% of predicted maximum heart rate (HRmax = 220 - age); 2) plateau in oxygen consumption (i.e., < 2.1 mL/kg/min increase in V̇O2max with concurrent increase in workload); 3) respiratory exchange ratio > 1.1; and 4) RPE of 18-20. Maximal oxygen uptake (V̇O2max) was defined as the highest 20-second value achieved during a MAET.
Statistical Analysis
All data are presented as mean ± standard deviation (SD). The statistical software IBM Statistical Package for the Social Sciences (SPSS) (version 20, IBM Corp., New York, NY, USA) was used for statistical analysis. The normal distribution of the data was analyzed by Shapiro-Wilks test. One-way analysis of variance (ANOVA) with post-hoc Bonferroni was used to test whether there was a significant difference in METs, morphological characteristics, and physical fitness between groups with different levels of physical activity. A 2 x 3 repeated-measures ANOVA examined the interaction between group (LPAL, MPAL and HPAL) and tests (Rest baPWV, MAET baPWV). To evaluate the differences between Rest baPWV and MAET baPWV, we compared the differences in baPWV of each group at rest and after MAET by a paired t-test. One-way ANOVA with post-hoc Bonferroni was used to assess the effects of baPWV in the three groups. Pearson's correlation coefficient was used to analyze the correlations between Rest baPWV and METs, age, seniority, morphological evaluations, and physical fitness parameters. The level of significance was set at p < 0.05.
Results
The basic characteristics of participants
All continuous data showed normal distributions (p > 0.05) by Shapiro-Wilks test, meeting the statistical assumptions of parametric tests. Table 1 presents total data and differences in physical activity (METs), age, seniority, morphological characteristics, and physical fitness in groups with different physical activity levels. The results showed significant differences in METs (F = 131.12, p < 0.001), weight (F = 3.70, p = 0.035), body mass index (BMI, F = 3.63, p = 0.037), relative fat mass (%FM, F = 17.90, p < 0.001), muscle mass ratio (MMR, F = 16.53, p < 0.001), and V̇O2max (F = 20.28, p < 0.001) and handgrip strength (HGS, F = 3.71, p = 0.035). Specifically, according to the post-hoc results, METs was significantly higher in the HPAL than in the MPAL and LPAL; relative fat mass was significantly lower in the HPAL than in the MPAL and LPAG; BMI was significantly lower in the HPAL than in the LPAL; MMR was significantly higher in the HPAL than in the MPAL and LPAL; V̇O2max was significantly higher in the HPAL than in the MPAL and LPAL, and also significantly higher in the MPAL than in the LPAL. Handgrip strength was significantly higher in the HPAL than in the LPAL. Rest baPWV was significantly lower in the HPAL than in the LPAL.
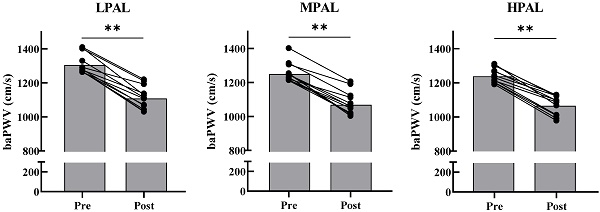
Differences in baPWV and the acute effect of MAET in the three groups
The results of the 2 x 3 repeated-measures ANOVA for baPWV among the three groups are shown in Table 2. No statistically significant group  test interactions were found for LPAL, MPAL, and HPAL (F = 1.06, p = 0.364, ƞ2 = 0.09). A significant effect was observed in groups (F = 3.48, p = 0.049, ƞ2 = 0.24) and tests (F = 413.69, p < 0.001, ƞ2 = 0.97), respectively. Post-hoc comparisons using the Bonferroni method revealed a significant difference in Rest baPWV between the HPAL and LPAL (p = 0.018); with paired t-tests revealed that the MAET baPWV values decreased significantly from Rest baPWV in LPAL (p < 0.001), MPAL (p < 0.001), and HPAL (p < 0.001), respectively.
test interactions were found for LPAL, MPAL, and HPAL (F = 1.06, p = 0.364, ƞ2 = 0.09). A significant effect was observed in groups (F = 3.48, p = 0.049, ƞ2 = 0.24) and tests (F = 413.69, p < 0.001, ƞ2 = 0.97), respectively. Post-hoc comparisons using the Bonferroni method revealed a significant difference in Rest baPWV between the HPAL and LPAL (p = 0.018); with paired t-tests revealed that the MAET baPWV values decreased significantly from Rest baPWV in LPAL (p < 0.001), MPAL (p < 0.001), and HPAL (p < 0.001), respectively.
METs, morphological characteristics, and physical fitness of participants in the three groups.
| All groups | LPAL | MPAL | HPAL | p-Value | |
|---|---|---|---|---|---|
| n =36 | n = 12 | n = 12 | n = 12 | ||
| METs | 1909.8 ± 1383.7 | 434.7 ± 132.1†‡ | 1726.3 ± 648.0† | 3568.3 ± 493.5 | <0.001 |
| 95% CI | 350.8-518.6 | 1314.6-2138.1 | 3254.7-3881.8 | ||
| Age (years) | 34.7 ± 5.9 | 36.0 ± 6.9 | 32.3 ± 5.8 | 35.8 ± 4.8 | 0.238 |
| 95% CI | 31.6-4.04 | 28.7-36.0 | 32.8-38.8 | ||
| Seniority (years) | 12.0 ± 6.5 | 14.1 ± 7.1 | 10.8 ± 6.1 | 11.1 ± 6.1 | 0.401 |
| 95% CI | 9.56-18.6 | 6.9-14.7 | 7.2-15.0 | ||
| Height (cm) | 176.2 ± 4.4 | 177.1 ± 4.4 | 176.3 ± 4.3 | 175.1 ± 4.7 | 0.546 |
| 95% CI | 174.3-179.9 | 173.6-179.1 | 172.1-178.1 | ||
| Weight (kg) | 80.2 ± 10.4 | 84.9 ± 11.6† | 81.3 ± 8.5 | 74.4 ± 8.5 | 0.035 |
| 95% CI | 77.6-92.3 | 75.9-86.8 | 69.0-79.8 | ||
| BMI (kg/m2) | 25.8 ± 2.8 | 27.1 ± 3.3† | 26.1 ± 1.8 | 24.3 ± 2.5 | 0.037 |
| 95% CI | 25.0-29.2 | 24.9-27.2 | 22.7-25.8 | ||
| %FM (%) | 23.3 ± 6.7 | 28.3 ± 6.2† | 24.7 ± 3.6† | 16.9 ± 4.1 | <0.001 |
| 95% CI | 24.4-32.3 | 22.4-27.0 | 14.3-19.5 | ||
| MM (kg) | 35.5 ± 3.2 | 34.2 ± 3.9 | 34.6 ± 2.7 | 34.9 ± 3.0 | 0.881 |
| 95% CI | 31.7-36.7 | 32.9-36.2 | 33.0-36.8 | ||
| MMR (%) | 43.4 ± 3.9 | 40.5 ± 3.6† | 42.6 ± 2.3† | 47.0 ± 2.4 | <0.001 |
| 95% CI | 38.2-42.8 | 41.2-44.1 | 45.5-48.5 | ||
| V̇O2max (ml/kg/min) | 43.9 ± 7.0 | 37.6 ± 5.8†‡ | 44.0 ± 3.8† | 50.1 ± 4.6 | <0.001 |
| 95% CI | 33.9-41.3 | 41.6-46.4 | 47.1-53.0 | ||
| HGS (kg) | 47.9 ± 4.6 | 45.2 ± 3.9† | 49.1 ± 4.8 | 49.5 ± 4.1 | 0.035 |
| 95% CI | 42.7-47.7 | 46.1-52.2 | 46.9-52.1 |
All data are presented as means ± SD. LPAL, low level of physical activity group. MPAL, moderate level of physical activity group. HPAL, high level of physical activity group. METs, metabolic equivalents. Seniority, work seniority. BMI, body mass index. %FM, relative fat mass. MM, muscle mass. MMR, muscle mass ratio. V̇O2max, maximal oxygen uptake. HGS, handgrip strength.
† Significantly difference from HPAL, p < 0.05. ‡ Significantly difference from MPAL, p < 0.05.
Changes in baPWV after maximal aerobic exercise testing for LPAL, MPAL, and HPAL. LPAL, low level of physical activity group. MPAL, moderate level of physical activity group. HPAL, high level of physical activity group. Gray bars represent the group mean. Solid black dots represent individual data points at pre and post-test, respectively. ** Indicates post-test was significantly difference from pre-test, p < 0.001.
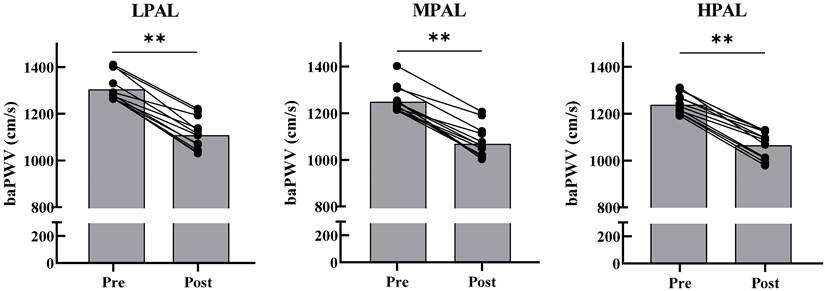
Measures results obtained Rest baPWV and MAET baPWV with different levels of physical activity groups.
| LPAL | MPAL | HPAL | p Group | p Test | p Group  Test Test | |
|---|---|---|---|---|---|---|
| n = 12 | n = 12 | n = 12 | ||||
| Rest baPWV (cm/s) | 1310.6 ± 60.5† | 1258.8 ± 56.5 | 1245.8 ± 43.5 | 0.049 | <0.001 | 0.364 |
| 95% CI | 1272.1-1349.1 | 1222.9-1294.6 | 1218.1-1273.4 | |||
| MAET baPWV (cm/s) | 1113.7 ± 67.6** | 1077.5 ± 68.1** | 1070.5 ± 56.9** | |||
| 95% CI | 1070.7-1156.6 | 1034.2-1120.8 | 1034.4-1106.6 |
All data are presented as means ± SD. LPAL, low level of physical activity group. MPAL, moderate level of physical activity group. HPAL, high level of physical activity group. baPWV, brachial-ankle pulse wave velocity. MAET, maximal aerobic exercise test.
† Significantly difference from HPAL, p < 0.05.
** Indicates MAET baPWV was significantly difference from Rest baPWV, p < 0.001.
Correlations between Rest baPWV, physical activity, age, seniority, physical fitness and morphological attributes.
| n = 36 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| baPWV | METs | Age | Seniority | VO2max | HGS | Height | Weight | BMI | MM | MMR | |
| METs | -0.415* | - | |||||||||
| Age | 0.500** | 0.020 | - | ||||||||
| Seniority | 0.538** | -0.142 | 0.904** | - | |||||||
| V̇O2max | -0.334* | 0.701** | -0.323 | -0.448** | - | ||||||
| HGS | -0.159 | 0.385* | -0.178 | -0.116 | 0.171 | - | |||||
| Height | -0.365* | -0.193 | -0.053 | -0.134 | -0.299 | -0.156 | - | ||||
| Weight | -0.067 | -0.382* | 0.173 | 0.275 | -0.641** | 0.050 | 0.554** | - | |||
| BMI | 0.103 | -0.372* | 0.227 | 0.380* | -0.620** | 0.126 | 0.207 | 0.928** | - | ||
| MM | -0.324 | 0.125 | 0.135 | 0.149 | -0.189 | 0.317 | 0.552** | 0.698** | 0.565** | - | |
| MMR | -0.233 | 0.683** | -0.104 | -0.245 | 0.717** | 0.247 | -0.241 | -0.702** | -0.729** | 0.012 | - |
| %FM | 0.234 | -0.697** | 0.101 | 0.251 | -0.730** | -0.226 | 0.241 | 0.732** | 0.763** | 0.034 | -0.997** |
baPWV, brachial-ankle pulse wave velocity. METs, metabolic equivalents. V̇O2max, maximal oxygen uptake. HGS, handgrip strength. BMI, body mass index. MM, muscle mass. MMR, muscle mass ratio. %FM, relative fat mass.
* Correlation is significant at the 0.05 level (2-tailed).
** Correlation is significant at the 0.01 level (2-tailed).
Correlation between the Rest baPWV, physical activity, age, seniority, physical fitness and morphological attributes
Table 3 shows the results of the correlation analysis between Rest baPWV, physical activity, age, seniority, physical fitness and morphological attributes. The results showed that Rest baPWV was positively correlated with age (r = 0.500, p = 0.002) and seniority (r = 0.538, p = 0.001), but negatively correlated with METs (r = -0.415, p = 0.012), height (r = -0.384, p = 0.021) and V̇O2max (r = -0.334, p = 0.046). METs was positively correlated with V̇O2max (r = 0.701, p < 0.001), handgrip strength (r = 0.385, p = 0.020) and MMR (r = 0.683, p < 0.001), but negatively correlated with weight (r = -0.382, p = 0.021), BMI (r = -0.372, p = 0.025) and relative fat mass (r = -0.697, p < 0.001). Seniority was positively correlated with BMI (r = 0.380, p = 0.022), but negatively correlated with V̇O2max (r = -0.480, p = 0.006). V̇O2max was positively correlated with MMR (r = 0.717, p < 0.001), but negatively correlated with weight (r = -0.641, p < 0.001), BMI (r = -0.620, p < 0.001) and relative fat mass (r = -0.730, p < 0.001).
Discussion
The primary aim of this study was to evaluate whether different levels of physical activity affect morphological attributes, physical fitness, and Rest baPWV in firefighters. In addition, the impact of different levels of physical activity on MAET baPWV after MAET was also examined in firefighters. The current study found that only highly physically active firefighters met the NFPA recommended indicators for safe fire rescue work in terms of body composition and physical fitness (PBF ≤ 18%, V̇O2max ≥ 42 ml/kg/min) [12, 29, 43], and they also had lower arterial stiffness. When the MAET was performed, arterial stiffness decreased in all three groups of firefighters.
Being overweight not only makes firefighters susceptible to CVD but may also lead to major cardiovascular events, such as myocardial infarction or fatal arrhythmia. Firefighters in Taiwan remain on call in the fire station for a long time. If they fail to develop exercise habits, they can easily develop low activity levels and a sedentary lifestyle. This study found that in terms of body composition, the difference between %FM and MMR were most significant between the different activity groups (p < 0.001). The HPAL had the lowest %FM (16.9 ± 4.1%) and the highest MMR (47.0 ± 2.4%), as well as better physical fitness performance. The NFPA maintains that, to perform fire rescue tasks safely and competently, firefighters need to pay equal attention to aerobic capacity and muscle strength training, their %FM should be optimized to less than 18% as much as possible, and they should have a V̇O2max of at least 42 ml/kg/min [12, 29, 43]. The results of this study showed that (i) the HPAL presented the NFPA's recommended values for %FM and V̇O2max; (ii) the MPAL presented the NFPA's recommended value for V̇O2max, but the same is not observed for %FM; and (iii) LPAL does not reach the values recommended by the NFPA for %FM and V̇O2max.
Research on the physical fitness of firefighters has confirmed that excessive body fat easily causes increases in body temperature and makes it difficult for heat to dissipate. This is not conducive to firefighters' disaster relief operations. It has also been reported that, for every additional year a firefighter's age increases, their body mass will also increase, for an average weight gain of 0.42 kg, BMI gain of 0.13 kg/m2, and %FM gain of 0.18% [44]. Ras and Leach (2022) investigated the relationship between levels of physical activity and physical fitness factors in firefighters. They used questionnaires to collect data on levels of physical activity and found that age and BMI were important predictors of insufficient physical activity among firefighters [45]. Corresponding to the results of this study, their results showed that working experience had a strong positive correlation with BMI, while differences in physical activity had a strong negative correlation with %FM and a strong positive correlation with MMR. However, age was not found to have correlations with %FM or MMR, suggesting that, as age increases but the level of physical activity is maintained, physical fitness can still be maintained above the levels recommended by the NFPA. The most urgent task in fire service is fire rescue. Research by Nazari et al. (2018) pointed out that, for the fire hose task in fire service, the correlation between firefighters' V̇O2max and HGS was the highest. In addition, they also found a correlation between the performance of weight-bearing ladder climbing tasks and V̇O2max [46]. It can be seen that high V̇O2max and MMR levels can improve task efficiency and performance, and physical fitness levels can be maintained through physical training as age increases.
In Taiwan, in addition to fighting fires, members of the fire department also have additional responsibilities, such as emergency medical rescue, fire safety inspections, and document processing. This workload also leads to a lack of time for exercise, hypertension, dyslipidemia, and obesity, thereby increasing the incidence of CVD. Ras et al. (2022) pointed out that during their careers, firefighters will encounter many risk factors, which will have negative effects on the body and cause accidental injuries. The highest proportion of deaths is caused by CVD stemming from a lack of exercise and overwork, which increases cardiovascular damage, accounting for 45% of the causes of death [45]. Gendron et al. (2020) conducted a study on firefighters' levels of physical activity and cardiovascular health indicators in Quebec, Canada. The results showed that firefighters who engaged in physical training while on duty had better cardiovascular health markers than those who did not [47].
Arterial stiffness is considered an important risk factor for CVD and can predict adverse cardiovascular outcomes [48, 49]. Therefore, assessing arterial stiffness may facilitate the identification of early-stage vascular diseases [50]. The average Rest baPWV value of participants in this study was 1271.6 ± 68.8 cm/s, but the analysis also showed that Rest baPWV was not significantly related to V̇O2max. In addition, Rest baPWV had a strong positive correlation with age and work seniority. There were significant differences in Rest baPWV between the three groups, with Rest baPWV significantly higher in the LPAL than in the HPAL. A baPWV result greater than 1400 cm/s indicates that blood vessels may tend to harden [25]. The average Rest baPWV value of LPAL was 1310.4 ± 80.4 cm/s, which is close to the recommended warning threshold of 1400 cm/s. It is necessary to pay attention to the subsequent tendency of blood vessels to harden.
This study showed that arterial stiffness decreased in all three groups after 10 minutes of MAET. Arterial stiffness significantly decreased by 14% in the HPAL, by 14% in the MPAL, and by 15% in the LPAL. In related literature, research by Santos et al. (2023) found that young and lean firefighters with high aerobic fitness showed significant decreases in arterial stiffness after simulated fire rescue operations and maximum aerobic exercise [51]. Niebauer et al. (2020) pointed out that a low-activity or sedentary lifestyle is likely to increase PWV and the risk of CVD. In that study, PWV was measured before exercise and 10 minutes after maximum intensity exercise. It was found that higher exercise intensity will lead to a decrease in PWV, while exercise intensity not exceeding 50% V̇O2max will not reduce PWV. Furthermore, in terms of the hemodynamic mechanism, high-intensity aerobic exercise will release higher amounts of nitric oxide, leading to greater relaxation of smooth muscle, followed by a further reduction in arterial stiffness [37]. In conclusion, the current study showed that the primary factors affecting baPWV are age, seniority, and level of physical activity. The group with the highest level of physical activity had the lowest Rest baPWV values, indicating better blood vessel elasticity. Ten minutes after high-intensity exercise in each group, decreases in baPWV were noted. However, the duration of such decreases in baPWV values will require follow-up research to confirm.
Limitations
This study has several limitations. First, this study may be limited by potential selection bias, namely the lack of female participants, who were not included in the current study because males predominantly constitute the local firefighter population. Therefore, these results may not be applicable to the physical fitness and cardiovascular health of female firefighters. Another limitation is that the firefighters tested in this study used a treadmill to measure their maximum aerobic exercise capacity in a fixed-temperature laboratory, which may not truly simulate the fatigue and physiological parameters produced during firefighting and disaster relief. Therefore, future studies should include larger sample sizes to confirm potential changes in arterial stiffness due to different health conditions, morphological and fitness attributes in both male and female firefighters.
Conclusions
The current study found that only highly active firefighters met the NFPA-recommended indicators for safe fire rescue work in terms of morphological attributes and physical fitness, and they also had lower arterial stiffness. When the maximum aerobic exercise test was performed, arterial stiffness decreased in all three groups of firefighters. The current study suggests that firefighters with low and medium activity levels should improve their activity levels and physical fitness to ensure safety and efficiency at work. Those of older age and longer working seniority should pay attention to the possibility of reductions in blood vessel elasticity. It is recommended that appropriate and periodized high-intensity physical training be implemented to reduce arterial stiffness and the incidence of arteriosclerosis, strengthening the total capability of disaster relief personnel while ensuring the health and safety of firefighters and protecting people's lives and property.
Abbreviations
ACSM: American College of Sports Medicine; AS: arterial stiffness; ANOVA: analysis of variance; baPWV: brachial-ankle pulse wave velocity; BMI: body mass index; CV: cardiovascular; CVD: cardiovascular disease; HGS: handgrip strength; HR: heart rate; HPAL: high level of physical activity group; IPAQ: International Physical Activity Questionnaire; LPAL: low level of physical activity group; MAET: maximal aerobic exercise test; METs: metabolic equivalents; MetS: metabolic syndrome; MPAL: moderate level of physical activity group; NFPA: National Fire Protection Association; PA: physical activity; PAL: physical activity level; %FM: relative fat mass; PF: physical fitness; PWV: pulse wave velocity; RPE: Rate of Perceived Exertion; MM: muscle mass; MMR: muscle mass ratio; SD: standard deviation; V̇O2max: maximal oxygen uptake.
Acknowledgements
The authors would like to thank all the participants of this study and their respective fire departments for their assistance. We also extend our gratitude to the principal investigator and the members of the Sports Technology Laboratory at National Taiwan Sport University for their support in the preparation and implementation of the study.
Author contributions
C.-H.C., Y.-J.H., and C.-H.H. designed the study. C.-H.C and C.-H.H. carried out the experiments. C.-H.C., Y.-J.H., and C.-H.H. analyzed the data. C.-H.C and C.-H.H. prepared the figure and tables and wrote the manuscript. All authors have read and agreed to the published version of the manuscript.
Ethics committee approval and patient consent
This study received ethical approval from the Institutional Review Board of Fu Jen Catholic University (New Taipei city, Taiwan) (Ethical Application Ref.: C111142).
Competing Interests
The authors have declared that no competing interest exists.
References
1. Horn GP, Gutzmer S, Fahs CA. et al. Physiological Recovery from Firefighting Activities in Rehabilitation and Beyond. Prehosp Emerg Care. 2011;15:214-5
2. Smith DL, DeBlois JP, Kales SN. et al. Cardiovascular Strain of Firefighting and the Risk of Sudden Cardiac Events. Exerc Sport Sci Rev. 2016;44(3):90-7
3. Munir F, Clemes S, Houdmont J. et al. Overweight and obesity in UK firefighters. Occup Med (Lond). 2012;62(5):362-5
4. Albert CM, Mittleman MA, Chae CU. et al. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343:1355-61
5. Skinner TL, Kelly VG, Boytar AN. et al. Aviation rescue firefighters physical fitness and predictors of task performance. J Sci Med Sport. 2020;23:1228-33
6. Mathias KC, Wu Y, Stewart DF. et al. Differences in 5-year weight change between younger and older US firefighters. BMC Public Health. 2021;21(1):1215
7. Smith DL. Firefighter Fitness: Improving Performance and Preventing Injuries and Fatalities. Curr Sports Med Rep. 2011;10:167-72
8. Durand G, Tsismenakis AJ, Jahnke SA. et al. Firefighters' physical activity: relation to fitness and cardiovascular disease risk. Med Sci Sports Exerc. 2011;43(9):1752-9
9. Garber CE, Blissmer B, Deschenes MR. et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334-59
10. Barry AM, Lyman KL, Dicks ND. et al. Firefighters Are More Physically Active On-Duty Compared to Off-Duty. Int J Environ Res Public Health. 2020;17(24):9380
11. Chizewski A, Box A, Kesler RM. et al. High Intensity Functional Training (HIFT) Improves Fitness in Recruit Firefighters. Int J Environ Res Public Health. 2021;18:13400
12. Storer TW, Dolezal BA, Abrazado ML. et al. Firefighter health and fitness assessment: a call to action. J Strength Cond Res. 2014;28(3):661-71
13. Durand G, Tsismenakis AJ, Jahnke SA. et al. Firefighters' physical activity: relation to fitness and cardiovascular disease risk. Med Sci Sports Exerc. 2011;43:1752-9
14. Scott JM, Thomas SM, Herndon JE 2nd. et al. Effects and tolerability of exercise therapy modality on cardiorespiratory fitness in lung cancer: a randomized controlled trial. J Cachexia Sarcopenia Muscle. 2021;12(6):1456-65
15. American College of Sports Medicine. ACSM's Guidelines for Graded Exercise Testing and Prescription, 10th ed. Philadelphia: Wolters Kluwer (Lippincott Williams & Wilkins). 2018:226-7
16. Forde C. Scoring the international physical activity questionnaire (IPAQ). Univ. Dublin 2018. Available at: https://ugc.futurelearn.com/uploads/files/bc/c5/bcc53b14-ec1e-4d90-88e3-1568682f32ae/IPAQ_PDF.pdf. Accessed 29 May. 2023
17. Boreham CA, Ferreira I, Twisk JW. et al. Cardiorespiratory fitness, physical activity, and arterial stiffness: the Northern Ireland Young Hearts Project. Hypertension. 2004;44:721-6
18. Leischik R, Foshag P, Strauß M. et al. Physical activity, cardiorespiratory fitness and carotid intima thickness: sedentary occupation as risk factor for atherosclerosis and obesity. Eur Rev Med Pharmacol Sci. 2015;19:3157-68
19. Mittleman MA, Maclure M, Tofler GH. et al. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329:1677-83
20. Cornell DJ, Noel SE, Zhang X. et al. Influence of a Training Academy on the Parasympathetic Nervous System Reactivation of Firefighter Recruits-An Observational Cohort Study. Int J Environ Res Public Health. 2020;18:109
21. U.S. Fire Administration. Firefighter Fatalities in the United States in 2021. Available at: https://www.usfa.fema.gov/downloads/pdf/publications/firefighter-fatalities-2021.pdf. Accessed 6 June. 2023
22. Baur DM, Christophi CA, Cook EF. et al. Low fitness is associated with exercise abnormalities among asymptomatic firefighters. Occup Med (Lond). 2012;62:566-9
23. Mancia G, Fagard R, Narkiewicz K. et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281-357
24. Pereira T, Correia C, Cardoso J. Novel Methods for Pulse Wave Velocity Measurement. J Med Biol Eng. 2015;35:555-65
25. West K, Spears K, Joyner B. et al. The acute effect of passively assisted trunk stretching on central arterial stiffness and blood pressure in middle-aged to older adults. Eur J Appl Physiol. 2024;124(6):1683-92
26. Zhou Y, Dan H, Bai L. et al. Nonlinear relationship with saturation effect observed between neutrophil to high-density lipoprotein cholesterol ratio and atherosclerosis in a health examination population: a cross-sectional study. BMC Cardiovasc Disord. 2022;22(1):424
27. Lu Y, Zhu M, Bai B. et al. Comparison of Carotid-Femoral and Brachial-Ankle Pulse-Wave Velocity in Association With Target Organ Damage in the Community-Dwelling Elderly Chinese: The Northern Shanghai Study. J Am Heart Assoc. 2017;6(2):e004168
28. Ito N, Ohishi M, Takagi T. et al. Clinical usefulness and limitations of brachial-ankle pulse wave velocity in the evaluation of cardiovascular complications in hypertensive patients. Hypertens Res. 2006;29(12):989-95
29. Nagel TR, Melton BF, Keeler JM. et al. Cardiorespiratory Fitness Is Inversely Associated With Aortic Arterial Stiffness in Firefighters. J Occup Environ Med. 2022;64:e641-6
30. Ianê-Siva C, Gonçalves R, de Oliveira Otoni C. et al. Aortic pulse wave comparison between controls and triathletes in baseline conditions and in response to acute maximum exercise. Sci Rep. 2023;13(1):15885
31. Hirshkowitz M, Whiton K, Albert SM. et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-3
32. Miller RM, Chambers TL, Burns SP. Validating InBody® 570 Multi-frequency Bioelectrical Impedance Analyzer versus DXA for Body Fat Percentage Analysis. J Exerc Physiol. 2016;19(5):71-8
33. Ndahimana D, Lee SH, Kim YJ. et al. Accuracy of dietary reference intake predictive equation for estimated energy requirements in female tennis athletes and non-athlete college students: comparison with the doubly labeled water method. Nutr Res Pract. 2017;11(1):51-6
34. Ichihashi S, Desormais I, Hashimoto T. et al. Accuracy and Reliability of the Ankle Brachial Index Measurement Using a Multicuff Oscillometric Device Versus the Doppler Method. Eur J Vasc Endovasc Surg. 2020;60(3):462-8
35. Liu X, Liu L, Wang R. et al. Early arteriosclerosis and its risk factors in subjects with prediabetes and new-onset diabetes. Endocr Connect. 2021;10:599-606
36. Melo X, Fernhall B, Santos DA. et al. The acute effect of maximal exercise on central and peripheral arterial stiffness indices and hemodynamics in children and adults. Appl Physiol Nutr Metab. 2016;41(3):266-76
37. Niebauer J, Müller EE, Schönfelder M. et al. Acute Effects of Winter Sports and Indoor Cycling on Arterial Stiffness. J Sports Sci Med. 2020;19:460-8
38. Seong JY, Ahn HY, Park Y. et al. Association Between Aerobic Exercise and Handgrip Strength in Adults: A Cross-Sectional Study Based on Data from the Korean National Health and Nutrition Examination Survey (2014-2017). J Nutr Health Aging. 2020;24(6):619-26
39. Lee MC, Jhang WL, Lee CC. et al. The Effect of Kefir Supplementation on Improving Human Endurance Exercise Performance and Antifatigue. Metabolites. 2021;11:136
40. Coquart JB, Garcin M, Parfitt G. et al. Prediction of maximal or peak oxygen uptake from ratings of perceived exertion. Sports Med. 2014;44(5):563-78
41. Balady GJ, Arena R, Sietsema K. et al. Interdisciplinary Council on Quality of Care and Outcomes Research. Clinician's Guide to Cardiopulmonary Exercise Testing in Adults: A Scientific Statement from the American Heart Association. Circulation. 2010;122:191-225
42. George JD, Paul SL, Hyde A. et al. Prediction of Maximum Oxygen Uptake Using Both Exercise and Non-Exercise Data. Meas Phys Educ Exerc Sci. 2009;13(1):1-12
43. National Fire Protection Association. NFPA 1582: Standard on Comprehensive Occupational Medical Program for Fire Departments. Quincy, MA: National Fire Protection Association. 2013
44. Bond CW, Waletzko SP, Reed V. et al. Retrospective Longitudinal Evaluation of Male Firefighter's Body Composition and Cardiovascular Health. J Occup Environ Med. 2022;64:123-30
45. Ras J, Leach L. Relationship Between Physical Activity, Coronary Artery Disease Risk Factors and Musculoskeletal Injuries in the City of Cape Town Fire and Rescue Service. Inquiry. 2022;59:00469580221084485
46. Nazari G, MacDermid JC, Sinden KE. et al. The Relationship between Physical Fitness and Simulated Firefighting Task Performance. Rehabil Res Pract. 2018;2018:3234176
47. Gendron P, Lajoie C, Laurencelle L. et al. Physical training in the fire station and firefighters' cardiovascular health. Occup Med (Lond). 2020;70:224-30
48. van Sloten TT, Sedaghat S, Laurent S. et al. Carotid stiffness is associated with incident stroke: a systematic review and individual participant data meta-analysis. J Am Coll Cardiol. 2015;66:2116-25
49. Ohkuma T, Ninomiya T, Tomiyama H. et al. Brachial-Ankle Pulse Wave Velocity and the Risk Prediction of Cardiovascular Disease: An Individual Participant Data Meta-Analysis. Hypertension. 2017;69:1045-52
50. Li W, Wang Y, Chen S. et al. Evaluation of Carotid Artery Atherosclerosis and Arterial Stiffness in Cardiovascular Disease Risk: An Ongoing Prospective Study From the Kailuan Cohort. Front Cardiovasc Med. 2022;9:812652
51. Santos V, Massuça LM, Monteiro L. et al. Comparison of Acute Arterial Responses Following a Rescue Simulation and Maximal Exercise in Professional Firefighters. Healthcare (Basel). 2023;11:1032
Author contact
![]() Corresponding author: Chun-Hao Chang, Ph.D. Graduate Institute of Sports Science, National Taiwan Sport University, Taoyuan 333325, Taiwan. Tel.: +886-3-3283201 ext: 2121, E-mail: hao781106edu.tw.
Corresponding author: Chun-Hao Chang, Ph.D. Graduate Institute of Sports Science, National Taiwan Sport University, Taoyuan 333325, Taiwan. Tel.: +886-3-3283201 ext: 2121, E-mail: hao781106edu.tw.

 Global reach, higher impact
Global reach, higher impact