3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(8):1378-1384. doi:10.7150/ijms.92837 This issue Cite
Research Paper
Validation of the Saga Fall Injury Risk Model
1. Department of General Medicine, Saga University Hospital, Saga, Japan.
2. Graduate School of Public Health, Shizuoka Graduate University of Public Health, Shizuoka, Japan.
3. Shimada Hospital of Medical Corporation Chouseikai, Saga, Japan.
4. Department of General Medicine, Yuai-Kai Foundation and Oda Hospital, Saga, Japan.
Received 2023-12-2; Accepted 2024-5-9; Published 2024-5-19
Abstract
Background: Predicting fall injuries can mitigate the sequelae of falls and potentially utilize medical resources effectively. This study aimed to externally validate the accuracy of the Saga Fall Injury Risk Model (SFIRM), consisting of six factors including age, sex, emergency transport, medical referral letter, Bedriddenness Rank, and history of falls, assessed upon admission.
Methods: This was a two-center, prospective, observational study. We included inpatients aged 20 years or older in two hospitals, an acute and a chronic care hospital, from October 2018 to September 2019. The predictive performance of the model was evaluated by calculating the area under the curve (AUC), 95% confidence interval (CI), and shrinkage coefficient of the entire study population. The minimum sample size of this study was 2,235 cases.
Results: A total of 3,549 patients, with a median age of 78 years, were included in the analysis, and men accounted for 47.9% of all the patients. Among these, 35 (0.99%) had fall injuries. The performance of the SFIRM, as measured by the AUC, was 0.721 (95% CI: 0.662-0.781). The observed fall incidence closely aligned with the predicted incidence calculated using the SFIRM, with a shrinkage coefficient of 0.867.
Conclusions: The external validation of the SFIRM in this two-center, prospective study showed good discrimination and calibration. This model can be easily applied upon admission and is valuable for fall injury prediction.
Keywords: Accidental Falls, Accidental Injuries, Validation Studies, Logistic Models, Risk Factors
Introduction
Falls in hospitals pose a significant problem because of their potential to cause physical burden [1] and psychological distress, such as fear and anxiety, among patients, their families, and healthcare workers [2,3]. Various prediction models have been developed to prevent falls; however, injuries occur in 15.7%-36.9% of all falls, with severe injuries occurring in 2.2%-12.8% of cases [4,5]. Fall-related injuries increase healthcare costs [6]. Many hospitals routinely use bed alarms, low beds, hip protectors, and other medical resources to prevent falls and fall injuries [7,8]. In addition to these physical preventative measures, fall prevention education and awareness for patients at high risk of falling and their families can reduce falls and associated disabilities [9]. However, given the limited medical resources and personnel, to ensure high-quality safety, it is possible to reduce medical costs by focusing on patients at a higher risk of fall injuries and efficiently allocating resources rather than targeting all patients.
Several models have been developed to predict fall-related injuries in older adults [10,11]. However, no specific established models or studies have targeted adult inpatients. Therefore, in our previous study, we developed a fall injury prediction model (Saga Fall Injury Risk Model [SFIRM]), using data from those with fall injuries and those without fall injuries or falls in the hospital that could be used to predict fall injuries [12]. The SFIRM is not a model for assessing the presence or absence of falls, but a simple model that can predict whether a fall injury will occur during hospitalization by evaluating all inpatients only once on admission [12]. The SFIRM comprises six factors including age, sex, emergency transport, medical referral letters, Bedriddenness Rank, and history of falls (Figure S1) [12]. In previous studies, Bedriddenness Rank has shown good inter-rater reliability and criterion-related validity [13]. Bedriddenness ranks were categorized into five major classes (normal, J: independence/autonomy, A: housebound, B: chair-bound, and C: bed-bound) [13]. Although external validation was not conducted in the previous study, internal validation showed an area under the curve (AUC) of 0.794 (95% confidence interval [95% CI]: 0.762-0.826) for this model [12]. Furthermore, the SFIRM can be applied upon admission and was developed using factors associated with fall injuries [12]. Among the six constituent factors, the odds ratios for Bedriddenness Rank were remarkably higher than those for other factors [12]. In addition, age [14,15], sex [16], history of falls [17], and Bedriddenness Rank A [18] are known risk factors for fall injuries. In contrast, the absence of emergency transport, presence of a medical referral letter, and Bedriddenness Ranks J, B, and C were newly identified predictive factors for fall injuries. However, after our prior research, the associations between these new predictive factors and fall injuries have not been adequately verified, and the reproducibility of this finding has not been confirmed.
This prospective study conducted in two hospitals, an acute and a chronic care hospital, aimed to externally validate the SFIRM. Furthermore, we aimed to verify whether the constituent factors of the model are reproducible for fall injuries.
Methods
Study design
This was a two-center, prospective, observational study. We recruited inpatients aged 20 years or older, admitted to two hospitals with different backgrounds, namely Yuai-Kai Foundation and Oda Hospital (an acute care hospital) and Saga City Fuji-Yamato Spa Hospital (provides both acute and chronic care), from October 2018 to September 2019 (Table S1). This study targeted patients of the same age group as in the previous study [12].
Data collection and definitions
All data, including admission date, patient age at admission [14,15], sex [12,16], department [19], presence of emergency transport [12], presence of a medical referral letter written by a primary physician outside of the two hospitals who saw a patient before admission [12], the Ministry of Health, Labour and Welfare's Activities of Daily Living scale (Bedriddenness Rank and Cognitive Function Score) [12], Barthel Index, Katz Index, Mini-Mental State Examination (MMSE) [20], ABC-dementia scale [21], use of hypnotic medication [22], presence of permanent residual damage from previous stroke [23], history of falls [12], visual impairment [18], surgery during hospital stay [24,25], rehabilitation [26], occurrence of in-hospital falls, and discharge date, were extracted from the electronic medical records of each hospital. We collected the data of factors related to falls or fall injuries. Detailed definitions of each item are provided in the Supplement 1. The number of falls, which were documented when the falls were reported by the patient or discovered by the attending nurse, was aggregated from incident and accident reports. Falls were defined as unexpected falls from any height or position regardless of injury, such as falls on stairs, chairs, or beds while standing, walking, sitting, or in a supine position. Fall-related injuries were defined as falls resulting in severity 1 or higher, according to the “Reasons for Falls and Falls and Injury Severity Input Criteria” developed from the Maryland Hospital Association Center for Performance Sciences' Quality Indicator Project [12,27]. Severity 1 indicates that although an injury has occurred, there are no sequelae or extension of hospital stay. We divided the patients into two groups: the “with fall injury” group, which included those who fell and had an injury with a severity of 1 or higher, and the “without fall injury” group, which included both those who did not fall and those who fell but did not have any fall injuries. We judged that all those who suffered injuries related to falls were considered to have fall injuries.
Assessment and prevention of falls during the study period
The predictive results generated from the SFIRM were not disclosed to attending nurses or physicians. Instead, the usual assessment of fall risk for hospitalized patients was implemented using each hospital's proprietary assessment tools and subsequent fall prevention measures based on those assessments. Depending on the patient's risk and circumstances, interventions such as guidance on appropriate footwear; use of sensors, cameras, impact-absorbing mats, low-height beds, belts, and bed rails; and assistance with toilet transfers were provided.
Statistical analysis
Statistical analysis of the survey variables was performed for the entire group, the group with fall injuries, and the group without fall injuries. Continuous and categorical variables were presented as median values (interquartile range) and absolute numbers (percentages), respectively. The standardized mean differences of each patient were analyzed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [28]. More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics [28]. This exploratory analysis did not consider multiplicity. We evaluated the predictive performance of the SFIRM by calculating the AUC, 95% CI, and shrinkage coefficient for all patients. In addition, for outcomes related to fall injuries, univariate analysis was conducted for variables that showed significance, and potential confounders such as age and sex were included as covariables in a logistic regression analysis. Analyses were performed using IBM SPSS Statistics, version 25 (IBM Corp., Armonk, NY, USA), with the significance level set at p less than 0.05.
Ethical considerations
This study adhered to the “Ethical Guidelines for Medical and Health Research Involving Human Subjects” provided by the Ministry of Health, Labour and Welfare and the Ministry of Education, Culture, Sports, Science and Technology in Japan. Ethical approval for this research was obtained from the Ethics Committee of Yuai-Kai Foundation and Oda Hospital (Approval No. 20230904). Informed consent was obtained from all patients using a comprehensive hospital agreement method, and patient anonymity was ensured.
Sample size
We calculated a minimum sample size of 2,235 patients for this study based on an effect size of 0.20 (predicted AUC of 0.70 and null hypothesis AUC of 0.50), a fall injury rate of 0.7%, an alpha error of 0.05, and a beta error of 0.20, using an estimated AUC of 0.794, as reported in a previous study [12].
Results
Of the 3,647 cases admitted during the study period, we excluded 96 cases with suspected input errors (e.g., Bedriddenness Rank of normal but Barthel Index < 10, Cognitive Function Score of normal but MMSE was evaluated, Cognitive Function Score of normal but ABC-dementia scale score < 10), and 34 cases with missing data, resulting in a total of 3,549 cases for analysis (Figure S2). The median age of the entire population was 78 years, and the proportion of men was 47.9%. The median length of hospital stay was 10 days. Among the cases, 35 (0.99%) had fall injuries. In the group with fall injuries, the median age was 86 years, 37.1% were men, and the median length of hospital stay was 37 days. The 34 cases with missing data had a median age of 60 years, 61.8% were men, 73.5% were scheduled for hospitalization, 41.2% had surgery, 2.9% had rehabilitation, and the median length of stay was 5 days.
The results of the univariate analysis are presented in Table 1. Age was significantly higher (86 years vs. 78 years) and the length of hospital stay was significantly longer (37 days vs. 9 days) in the group with fall injuries than in the group without fall injuries. Regarding admission type, emergency admissions (80% vs. 38.3%), the use of hypnotic medications (25.7% vs. 9.7%), history of falls (34.3% vs. 9.3%), visual impairment (60.7% vs. 34.0%), and rehabilitation (65.7% vs. 36.6%) were significantly more common in the fall injury group than in the without fall injury group. In contrast, the incidence of surgery was significantly lower in the fall injury group than in the without fall injury group (11.4% vs. 28.1%). Higher proportions of fall injuries were observed in the groups with Bedriddenness Ranks J, B, and C, as well as in the groups with Cognitive Function Scores I to IV, and these distributions differed significantly between the fall injury and without fall injury groups. The Barthel Index (55 vs. 100) and ABC-dementia scale (85 vs. 117) scores were significantly lower in the group with fall injuries than in the group without fall injuries. No significant differences were observed between the fall and without fall injury groups regarding sex, emergency transport, medical referral letters, permanent residual damage from previous stroke, or MMSE scores.
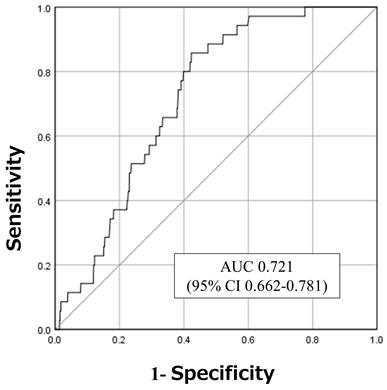
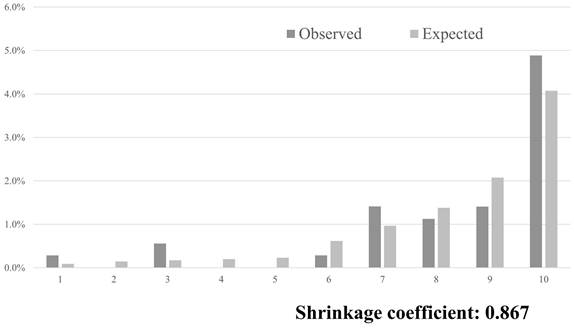
The AUC, which was used to assess the performance of the SFIRM, was 0.721 (95% CI: 0.662-0.781; Figure 1). The observed incidence of falls was consistent with the predicted incidence calculated using the SFIRM, with a shrinkage coefficient of 0.867 (Figure 2). The cutoff values for the model with 91% sensitivity and 48% specificity points was -5.80, and with the 14% sensitivity and 90% specificity points was -3.73. The cutoff value according to Youden's Index was -5.09, with sensitivity of 86% and specificity of 58% (Table 2).
Variables with significance in the univariate analysis, including age, history of falls, Bedriddenness Rank, and sex, were entered as covariables in a forced logistic regression analysis. Age (p = 0.958), sex (p = 0.488), and Bedriddenness Rank A (p = 0.075) were not significantly associated with fall injuries. Bedriddenness Ranks J, B, and C had odds ratios of 8.0 (95% CI: 1.71-37.07, p = 0.008), 13.5 (95% CI: 3.36-54.69, p < 0.001), and 6.1 (95% CI: 1.38-27.44, p = 0.017), respectively, all of which were significantly associated with fall injuries (Table 3).
Characteristics of patients and results of univariable analysis.
| Variable, Category | All patients n = 3549 | With Fall injury | Without Fall injury | SMD |
|---|---|---|---|---|
| n = 35 | n = 3514 | |||
| Age, years | 78 (65-87) | 86 (78-90) | 78 (65-87) | 0.602 |
| Sex, Men | 1700 (47.9) | 13 (37.1) | 1687 (48.0) | 0.221 |
| Department, Internal Medicine | 1998 (56.3) | 27 (77.1) | 1971 (56.1) | 0.584 |
| Department, Neurosurgery | 68 (1.9) | 2 (5.7) | 66 (1.9) | |
| Emergency admission, Yes | 1372 (38.7) | 28 (80.0) | 1344 (38.3) | 0.938 |
| Transported by ambulance, Yes | 474 (13.4) | 6 (17.1) | 468 (13.3) | 0.107 |
| Referral letter, Presence | 1065 (30.0) | 7 (20.0) | 1058 (30.1) | 0.234 |
| Hypnotic medications, Using | 344 (9.9) | 9 (25.7) | 335 (9.7) | 0.428 |
| Permanent residual damage from previous stroke, Presence | 218 (6.3) | 3 (8.6) | 215 (6.3) | 0.088 |
| History of falls, Presence | 338 (9.5) | 12 (34.3) | 326 (9.3) | 0.629 |
| Visual impairment, Presence | 1135 (34.2) | 17 (60.7) | 1118 (34.0) | 0.555 |
| Bedriddenness rank,a Normal | 1788 (50.4) | 3 (8.6) | 1785 (50.8) | 1.134 |
| Bedriddenness rank,a J | 317 (8.9) | 5 (14.3) | 312 (8.9) | |
| Bedriddenness rank,a A | 410 (11.6) | 4 (11.4) | 406 (11.6) | |
| Bedriddenness rank,a B | 517 (14.6) | 16 (45.7) | 501 (14.3) | |
| Bedriddenness rank,a C | 517 (14.6) | 7 (20.0) | 510 (14.5) | |
| Cognitive function score,b Normal | 2185 (61.8) | 5 (14.7) | 2180 (62.2) | 1.150 |
| Cognitive function score,b I | 423 (12.0) | 8 (23.5) | 415 (11.8) | |
| Cognitive function score,b II | 341 (9.6) | 10 (29.4) | 331 (9.4) | |
| Cognitive function score,b III | 453 (12.8) | 8 (23.5) | 445 (12.7) | |
| Cognitive function score,b IV | 119 (3.4) | 3 (8.8) | 116 (3.3) | |
| Cognitive function score,b M | 16 (0.5) | 0 (0.0) | 16 (0.5) | |
| Barthel index | 100 (52-100) | 55 (25-75) | 100 (55-100) | 0.680 |
| ABC-dementia Scale | 117 (91-117) | 85 (68-106) | 117 (91-117) | 0.580 |
| Mini-Mental State Examinationc | 13 (0-21) | 16 (9-20) | 13 (0-21) | 0.224 |
| Surgery, Undergone | 991 (27.9) | 4 (11.4) | 987 (28.1) | 0.428 |
| Rehabilitation, Undergone | 1309 (36.9) | 23 (65.7) | 1286 (36.6) | 0.609 |
| Length of hospital stay (days) | 10 (5-18) | 37 (22-61) | 9 (5-18) | 1.103 |
Continuous and categorical variables are shown as median (interquartile range) and frequency (percent).
SMD, standardized mean difference.
a Bedriddenness Ranks: J, independence/autonomy; A, house-bound; B, chair-bound; C, bed-bound.
b Cognitive Function Scores: I, almost independent in daily living with only slight cognitive impairment; II, independent with slight difficulty in daily living or communication under careful overseeing; III, dependent in daily living or communication; IV, dependent in daily living or communication, and requires constant care; M, severe psychological symptoms, troubled behaviors or severe physical disorders requiring specialized medical service.
c Mini-Mental State Examination was assessed within 72 h of admission, for those determined to have an abnormal Cognitive Function Score.
Discussion
This study prospectively validated the SFIRM that was developed in a previous study on in-hospital fall injuries among inpatients [12]. The SFIRM showed good discrimination, with an AUC of 0.721, and both calibration and discrimination were satisfactory. Furthermore, the results of the logistic regression analysis demonstrated a significant association between fall history and Bedriddenness Ranks J, B, and C.
Validation of the predictive model with the cutoff points determined in the present study.
| Statistics for 3 cutoff points | Overall | Overall With the cutoff points set in the development study |
|---|---|---|
| Cutoff value for scores | -5.80 | -5.27 |
| Probability a | 0.3 | 0.5 |
| Sensitivity | 91 | 86 |
| Specificity | 48 | 55 |
| Positive predictive value | 1.7 | 1.9 |
| Negative predictive value | 99.8 | 99.7 |
| Cutoff value for scores | -5.09 | -5.08 |
| Probability a | 0.6 | 0.6 |
| Sensitivity | 86 | 83 |
| Specificity | 58 | 58 |
| Positive predictive value | 2.0 | 1.9 |
| Negative predictive value | 99.8 | 99.7 |
| Cutoff value for scores | -3.73 | -3.80 |
| Probability a | 2.3 | 2.2 |
| Sensitivity | 14 | 14 |
| Specificity | 90 | 88 |
| Positive predictive value | 1.4 | 1.2 |
| Negative predictive value | 99 | 99 |
a The value was calculated as the probability of a fall for patients with defined score.
Probability=100×Exp(score)/(1+Exp(score))
Results of multivariable logistic regression analysis.
| Variable, Category (Reference) | OR | 95% CI | p valuea |
|---|---|---|---|
| Age | 1.0 | 0.97-1.03 | 0.958 |
| Sex, Female (Male) | 1.3 | 0.63-2.60 | 0.488 |
| History of falls, Presence (Absence) | 2.8 | 1.32-5.72 | 0.007 |
| Bedriddenness rank, J (Normal) | 8.0 | 1.71-37.07 | 0.008 |
| Bedriddenness rank, A (Normal) | 4.4 | 0.86-22.00 | 0.075 |
| Bedriddenness rank, B (Normal) | 13.5 | 3.36-54.69 | < 0.001 |
| Bedriddenness rank, C (Normal) | 6.1 | 1.38-27.44 | 0.017 |
OR: odds ratio; 95% CI: 95% confidence interval
a p values for Wald test.
Receiver operating characteristics and areas under the curves. AUC: area under the curve; 95% CI: 95% confidence interval.
Predicted and observed rates of falls in 10 groups, divided into 10 deciles by score using the predictive model.
In contrast to the previous development study, the present study conducted an external validation using prospectively collected data. The SFIRM utilizes data from an acute care hospital where the model was initially developed and included data from a different background, namely, a chronic care hospital. Despite this diverse setting, the model demonstrated good accuracy, which was similar to that of the previous study [12], confirming the utility of our SFIRM. Furthermore, the SFIRM can be applied at the time of admission without requiring special additional tests such as blood examinations or physical performance assessments because it is simple and comprises only six factors [12]. Moreover, this model incorporated the Bedriddenness Ranks, which is widely used in Japanese healthcare and long-term care settings [29,30]. By identifying patients at risk of fall injuries using the convenient and valuable SFIRM, severe fall injuries that tend to result in high inpatient medical expenses can be prevented [31], thereby contributing to cost containment. Therefore, the SFIRM is a socially beneficial and suitable fall injury prediction model for healthcare and long-term care settings.
Among the six factors of the SFIRM, the univariate analysis showed that age, history of falls, and Bedriddenness Rank were significantly different between the fall and without fall injury groups. In the logistic regression analysis, history of falls and Bedriddenness Ranks J, B, and C showed significant associations with fall injuries. These factors may be useful factors for predicting fall injuries. History of falls is widely recognized as a contributing factor, and previous studies have reported that patients with history of a fall are at a higher risk of sustaining injuries during subsequent falls [17]. Bedriddenness Rank is a well-established activities of daily living scale used in Japanese long-term care and healthcare settings, showing good criterion-related validity with existing measures such as the Barthel Index and Katz Index [13]. Bedriddenness Rank J represents individuals with some form of impairment but are mostly independent in their daily lives [18]. Consequently, factors such as reduced balance capabilities due to physical impairments [32] and decreased muscle strength [33] might contribute to increased risk of fall injuries in such individuals compared with those in healthy individuals. In addition, cognitive impairment may lead to delirium [34] upon admission, thereby increasing the risk of falls [35]. Factors associated with fall injuries, such as lower limb muscle weakness and the presence of caregivers, have been reported [5], and the judgment criteria for Bedriddenness Rank B include the necessity of indoor assistance [18], which may also contribute to fall injuries. Furthermore, the criterion for Bedriddenness Rank C, that is, whether the patient can turn over in bed independently [18], is predicted to be associated with physical function decline and muscle weakness. Given the significant relationship between physical function decline and injuries, such as fractures or trauma resulting from falls [10], a potential association with fall injuries may exist. In addition, patients who are bedridden are at higher risk of osteoporosis, which increases the risk of fractures [36], potentially contributing to fall injuries.
Limitations
This study was an external validation of SFIRM developed in previous research. Therefore, it was necessary to evaluate the population with the same condition as in the previous study, and the validation was performed in groups with fall injuries and without fall or fall injuries. This was a prospective study; however, owing to the limited number of fall injury events, we could not conduct a multivariable analysis with sufficient covariables. In addition, no adjustments for interventions aimed at preventing falls were made. Additionally, there could be fall or fall injury risk factors that were not collected in this study; therefore, we could not adjust for all confounding factors. Furthermore, we could not evaluate the inter-rater reliability for each item. The group with missing data may have included more younger patients with short-term planned hospitalizations than did the group analyzed in the present study, which could have potentially influenced the results.
Conclusion
The external validation of the SFIRM, which was prospectively conducted in two hospitals in the population with the same condition as in the previous study, showed good discrimination and calibration in this study. The SFIRM can be easily applied upon admission and is valuable for fall injury prediction. Moreover, history of a fall and Bedriddenness Rank were associated with fall injuries, potentially contributing to the prediction of such injuries. Therefore, further studies validating the model in a larger or a different population are necessary.
Abbreviations
AUC: area under the curve; CI: confidence interval; MMSE: Mini-Mental State Examination; SFIRM: Saga Fall Injury Risk Model.
Supplementary Material
Supplementary figures, table and information.
Acknowledgements
We thank Kenta Yamaguchi, Mayumi Harasaki, Fujiko Eguchi, Chieko Nagaike, Osamu Kojiro, Toshinobu Eguchi, Yasuhiro Chibu, Midori Moriyama, Kazumi Ukon, Tomoko Tokuda, Yoichi Onaka, Hiroyuki Fujiki, Akira Kubo, Minoru Minamisato, Akiko Ogushi, Yoko Itoyama, Mitsuko Umeno, Eriko Oka, Miho Hayashida, Chihiro Saito, Dr. Akiko Dogomori, Dr. Kazumi Mori, Dr. Masahiko Nakamura, Dr. Yuka Hirakawa, Dr. Yoshinori Tokushima, and Dr. Shun Yamashita for the assistance with data acquisition. We also thank the Translational Research Center for Medical Innovation and Dr. Masanori Fukushima from the Learning Health Society Institute for research support and assistance with analysis. We would like to thank Editage (www.editage.jp) for English language editing.
Competing Interests
Masaki Tago is supported by grants from the Japan Society for the Promotion of Science, JSPS KAKENHI (Grant Number JP18K17322 and JP21H03166). Naoko E. Katsuki is supported by grants from the Japan Society for the Promotion of Science, JSPS KAKENHI (Grant Number JP23K16257). The sponsor of the study had no role in the preparation of the manuscript.
References
1. Tang CTL, Sing CW, Kwok TCY, Li GHY, Cheung CL. Secular trends in fall-related hospitalizations in adolescents, youth and adults: a population-based study. Lancet Reg Health West Pac. 2021;12:100183
2. Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37:19-24
3. Miyamoto M, Hara M, Shoji H, Etoh R. The recognition by nurses and care-workers of the burden of caring for fall prevention and continence for patients with dementia during night shifts. Bulletin Shimane Univ Faculty Med. 2016;38:11-7
4. Kobayashi K, Kido N, Wakabayashi S. et al. Association between fall-related serious injury and activity during fall in an acute care hospital. PLoS One. 2023;18:e0288320
5. Kim MS, Jung HM, Lee HY, Kim J. Risk factors for fall-related serious injury among Korean adults: A cross-sectional retrospective analysis. Int J Environ Res Public Health. 2021;18:1239
6. Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res. 2016;58:99-103
7. Haines TP, Bell RA, Varghese PN. Pragmatic, cluster randomized trial of a policy to introduce low-low beds to hospital wards for the prevention of falls and fall injuries. J Am Geriatr Soc. 2010;58:435-41
8. Harada A, Mizuno M, Takemura M. et al. Hip fracture prevention trial using hip protectors in Japanese nursing homes. Osteoporos Int. 2001;12:215-21
9. Tricco AC, Thomas SM, Veroniki AA. et al. Quality improvement strategies to prevent falls in older adults: a systematic review and network meta-analysis. Age Ageing. 2019;48:337-46
10. Hars M, Audet MC, Herrmann F. et al. Functional performances on admission predict in-hospital falls, injurious falls, and fractures in older patients: A prospective study. J Bone Miner Res. 2018;33:852-9
11. Zhao M, Li S, Xu Y, Su X, Jiang H. Developing a scoring model to predict the risk of injurious falls in elderly patients: A retrospective case-control study in multicenter acute hospitals. Clin Interv Aging. 2020;15:1767-78
12. Yaita S, Tago M, Katsuki NE. et al. A simple and accurate model for predicting fall injuries in hospitalized patients: Insights from a retrospective observational study in Japan. Med Sci Monit. 2023;29:e941252
13. Tago M, Katsuki NE, Yaita S. et al. High inter-rater reliability of Japanese bedriddenness ranks and cognitive function scores: a hospital-based prospective observational study. BMC Geriatr. 2021;21:1-10
14. Kannus P, Niemi S, Sievänen H, Parkkari J. Fall-induced wounds and lacerations in older Finns between 1970 and 2014. Aging Clin Exp Res. 2018;30:71-5
15. Verma SK, Willetts JL, Corns HL, Marucci-Wellman HR, Lombardi DA, Courtney TK. Falls and fall-related injuries among community-dwelling adults in the United States. PLoS One. 2016;11:e0150939
16. Ghosh M, O'Connell B, Afrifa-Yamoah E, Kitchen S, Coventry L. A retrospective cohort study of factors associated with severity of falls in hospital patients. Sci Rep. 2022;12:12266
17. Aryee E, James SL, Hunt GM, Ryder HF. Identifying protective and risk factors for injurious falls in patients hospitalized for acute care: a retrospective case-control study. BMC Geriatr. 2017;17:260
18. Aihara H, Tago M, Oishi T, Katsuki NE, Yamashita SI. Visual impairment, partially dependent ADL and extremely old age could be predictors for severe fall injuries in acute care settings. Int J Gerontol. 2018;12:175-9
19. Tago M, Katsuki NE, Oda Y, Nakatani E, Sugioka T, Yamashita SI. New predictive models for falls among inpatients using public ADL scale in Japan: A retrospective observational study of 7,858 patients in acute care setting. PLoS One. 2020;15:e0236130
20. Jensen J, Nyberg L, Gustafson Y, Lundin-Olsson L. Fall and injury prevention in residential care-effects in residents with higher and lower levels of cognition. J Am Geriatr Soc. 2003;51:627-35
21. Mori T, Kikuchi T, Umeda-Kameyama Y. et al. ABC Dementia Scale: A quick assessment tool for determining Alzheimer's disease severity. Dement Geriatr Cogn Dis Extra. 2018;8:85-97
22. Kobayashi K, Ando K, Nakashima H, Suzuki Y, Nagao Y, Imagama S. Relationship between use of sleep medication and accidental falls during hospitalization. Nagoya J Med Sci. 2021;83:851-60
23. Willig R, Luukinen H, Jalovaara P. Factors related to occurrence of hip fracture during a fall on the hip. Public Health. 2003;117:25-30
24. Miller KL, Richter HE, Graybill CS, Neumayer LA. Fall risk and function in older women after gynecologic surgery. Arch Gerontol Geriatr. 2017;73:37-42
25. Kronzer VL, Wildes TM, Stark SL, Avidan MS. Review of perioperative falls. Br J Anaesth. 2016;117:720-32
26. Hayashi S, Takenaka T, Iwamoto C. et al. A cross-sectional study on falls in a convalescent rehabilitation ward. Jpn J Fall Prev. 2016;2:33-9
27. Kazandjian VA, Lawthers J, Cernak CM, Pipesh FC. Relating outcomes to processes of care: the Maryland Hospital Association's Quality Indicator Project (QI Project). Jt Comm J Qual Improv. 1993;19:530-8
28. Kanda Y. Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transplant. 2013;48:452-8
29. Yokobayashi K, Matsushima M, Watanabe T, Fujinuma Y, Tazuma S. Prospective cohort study of fever incidence and risk in elderly persons living at home. BMJ Open. 2014;4:e004998
30. General Affairs Division, Health, Welfare Bureau for the Elderly Ministry of Health, Labour, Welfare, Japan. The long-term care insurance system in: Long-term care insurance in Japan. January, 2002. Accessed November 24. 2023 https://www.mhlw.go.jp/english/topics/elderly/care/2.html
31. van der Vlegel M, Haagsma JA, Geraerds AJLM, de Munter L, de Jongh MAC, Polinder S. Health care costs of injury in the older population: a prospective multicentre cohort study in the Netherlands. BMC Geriatr. 2020;20:417
32. Zhao R, Bu W, Chen X. The efficacy and safety of exercise for prevention of fall-related injuries in older people with different health conditions, and differing intervention protocols: a meta-analysis of randomized controlled trials. BMC Geriatr. 2019;19:341
33. Petrella JK, Kim JS, Tuggle SC, Hall SR, Bamman MM. Age differences in knee extension power, contractile velocity, and fatigability. J Appl Physiol (1985). 2005;98:211-20
34. Mazur K, Wilczyński K, Szewieczek J. Geriatric falls in the context of a hospital fall prevention program: delirium, low body mass index, and other risk factors. Clin Interv Aging. 2016;11:1253-61
35. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383:911-22
36. Eimori K, Endo N, Uchiyama S, Takahashi Y, Kawashima H, Watanabe K. Disrupted bone metabolism in long-term bedridden patients. PLoS One. 2016;11:e0156991
Author contact
![]() Corresponding author: Masaki Tago, Department of General Medicine, Saga University Hospital, Saga, Japan. Address: 5-1-1 Nabeshima, Saga, 849-8501 Japan. TEL: +81-952-34-3238. FAX: +81-952-34-2029. E-mail: tagomassaga-u.ac.jp.
Corresponding author: Masaki Tago, Department of General Medicine, Saga University Hospital, Saga, Japan. Address: 5-1-1 Nabeshima, Saga, 849-8501 Japan. TEL: +81-952-34-3238. FAX: +81-952-34-2029. E-mail: tagomassaga-u.ac.jp.

 Global reach, higher impact
Global reach, higher impact