3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(7):1280-1291. doi:10.7150/ijms.96575 This issue Cite
Research Paper
Clinical effects of traditional Chinese herbal medicine management in patients with COVID-19 sequelae: A hospital-based retrospective cohort study in Taiwan
1. Department of Chinese Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan.
2. School of Post-Baccalaureate Chinese Medicine, Tzu Chi University, Hualien, Taiwan.
3. Department of Research, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan.
4. Department of Nursing, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan.
5. Division of Pulmonary Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan.
6. School of Medicine, Tzu-Chi University, Hualien, Taiwan.
7. Department of Internal Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan.
# Prof. You-Chen Chao and Chou-Chin Lan contribute equally to this work.
Abstract
Introduction: An estimated 43% of COVID-19 patients showed sequelae, including fatigue, neurocognitive impairment, respiratory symptoms, and smell or taste disorders. These sequelae significantly affect an individual's health, work capacity, healthcare systems, and socioeconomic aspects. Traditional Chinese herbal medicine (TCHM) management showed clinical benefits in treating patients with COVID-19 sequelae. This study aimed to analyze the effects of personalized TCHM management in patients with COVID-19 sequelae.
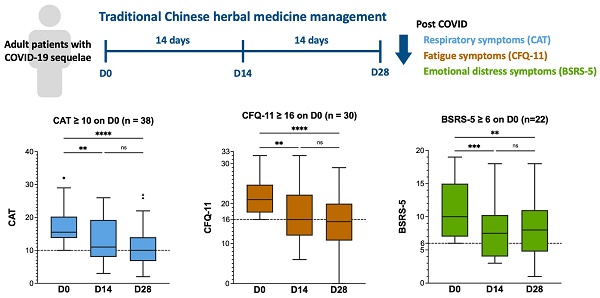
Methods: After the COVID-19 outbreak in Taiwan, we recorded Chronic Obstructive Pulmonary Disease Assessment Tool (CAT), Chalder Fatigue Questionnaire (CFQ-11), and Brief Symptom Rating Scale (BSRS-5) to assess post-COVID respiratory, fatigue, and emotional distress symptoms, respectively. In this study, we retrospectively reviewed the medical records between July 2022 and March 2023. We analyzed the effects of TCHM administration after 14- and 28-days of treatment.
Results: 47 patients were included in this study. The results demonstrated that personalized TCHM treatment significantly improved the CAT, CFQ-11, and BSRS-5 scores after 14 and 28 days. TCHM alleviated physical and psychological fatigue. In logistic regression analysis, there was no statistically significant differences in the severity of the baseline symptoms and TCHM administration effects concerning the duration since the initial confirmation of COVID-19, sex, age, or dietary preference (non-vegetarian or vegetarian).
Conclusions: Our study suggested that personalized TCHM treatment notably reduced fatigue, respiratory and emotional distress symptoms after 14- and 28-days of treatment in patients with COVID-19 sequelae. We propose that TCHM should be considered as an effective intervention for patients with COVID-19 sequelae.
Keywords: COVID-19 sequelae, traditional Chinese herbal medicine, CAT, CFQ-11, BSRS-5

 Global reach, higher impact
Global reach, higher impact