3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(5):958-964. doi:10.7150/ijms.94432 This issue Cite
Research Paper
Establishment of an Animal Model of Dog Bite Injuries
State Key Laboratory of Oral Diseases & National Clinical Research Center for Oral Diseases & Department of Oral and Maxillofacial Surgery, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, Sichuan Province, China.
Received 2024-1-18; Accepted 2024-3-20; Published 2024-3-31
Abstract
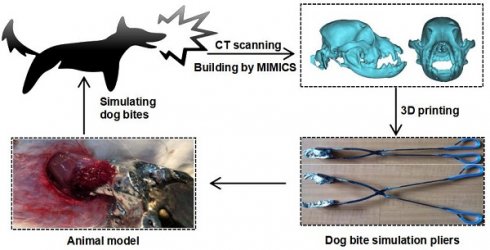
Nowadays dog bite is becoming a world public health problem. Therefore, the study aimed to develop a dog bite animal model that is helpful to solve these problems. In this study, the skull of an adult dog was scanned. The three-dimensional model of the dog maxillofacial bones and dentition was built by MIMICS. Next, the model was printed with Co-Cr alloy by using selective laser sintering technology to develop the dog bite simulation pliers. Then, to simulate dog bite to most, the maximum bite force of the pliers was measured and actions contained in dog bite process was analyzed. Afterwards, according to action analysis results, rabbits were bitten by the prepared instrument in actions that simulate dog's bite. Finally, the reproducibility and controllability of this animal model of dog bite injuries was validated in an in vivo study. The results showed a reliable animal model of dog bite injuries has been developed in this study. The sites and severities of the injuries could be adjusted as the operator wishes and the animal model of dog bite injuries was highly repeatable. This study also indicates the feasibility of using digital technology in establishing animal bite models.
Keywords: bites, dog, animal models, wounds and Injuries, sutures
Introduction
With the increasing number of dogs in modern society, the occurrence of dog bite injuries has become more frequent [1-3]. According to the World Health Organization [4], dog bites are among the top 12 causes of non-fatal injuries worldwide. A dog bite can result in a severe laceration, avulsed tissue, and even bone fractures due to the dog's powerful occlusal force and sharp teeth [5-7]. Furthermore, a dog's mouth is a source of pathogenic bacteria, which carries a risk of infection and rabies [8-10]. In addition, the dog may hold on for a long duration of time to tear the victim's tissue. Damage caused by such prolonged bites raises the possibility of local tissue necrosis and avulsion, eventually resulting in tissue defects that severely impair patients' quality of life [11,12].
The current basic therapeutic principles of dog bite injuries have been established after long clinical practice [13,14]. However, the specific treatments of dog bite injuries remain controversial [15-17]. The reason lies in the complexity of the lesions in dog bite injuries, which often vary greatly in extent and depth, presents significant challenges in their treatment, such as the need for plastic sutures and the consideration of flap surgeries [18-19]. Notably, all previous studies on dog bite injuries were clinical studies, and most of these were case reports or summaries of clinical experience; therefore, they lack adequate reliability [20-30]. The main reason for this situation is that dog bite injuries range widely in severity and there are great individual differences among patients. Hence, a reproducible and comparable animal model is very meaningful and demanded.
The objective of this study was to establish an animal model of dog bite injuries by utilizing computer image processing and selective laser sintering technologies. We hypothesized that the dog bite simulation pliers could accurately replicate jaws with correct occlusal contact. The specific aims of the study were to develop the dog bite simulation pliers and to validate the efficacy in producing dog bite injuries.
Materials and Methods
Ethics statement
All animal experiment protocols were prospectively approved by the Research Ethics Committee for Laboratory Animal Science of West China Hospital of Stomatology, Sichuan University (Protocol Number: WCHSIRB-D-2017-251). This study was conducted in strict accordance with the recommendations of the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. Animals were housed in a temperature-, humidity-, and air renewal-controlled room. Animals were fed standard dried diet and water. All surgeries were performed under pentobarbital sodium anesthesia (30 mg/kg), and all efforts were made to minimize suffering.
Data collection and analysis
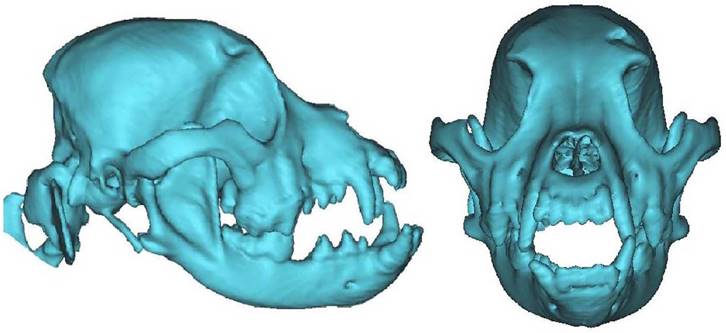
A Chinese male rural dog with a correct bite and full dentition (age, 34 months; weight, 18 kg) was anesthetized with 30 mg/kg of pentobarbital sodium. The skull of the dog was then scanned by spiral computed tomography (CT) (Philips, the Netherlands). A three-dimensional model of the dog's maxillofacial bones and dentition was built from the spiral CT data by MIMICS software, version 16.0.0 (Materialise NV, Leuven, Belgium) and stored in standard template library format after modification.
Preparation of dog bite simulation instrument
Cobalt-chromium (Co-Cr) alloy (Concept Laser, Lichtenfels, Germany) was used as the printing material [31]. Through selective laser sintering technology, a direct metal laser sintering machine (EOSINT M 270; EOS, Krailling, Germany) was used to reconstruct a metallic model of the dog's maxillofacial bones and dentition. The model was welded on the end of the short handle of a pair of pliers to simulate jaws after correct occlusal contact had been established. The jaws were then sharpened to imitate the dog's teeth. The finished instrument was termed dog bite simulation pliers.
Maximum bite force measurements of dog bite simulation instrument
The dog bite simulation instrument was used to bite a piezoelectric isometric Kistler force transducer (9311B, range ± 5000 N; Kistler Instrument Corp, Winterthur, Switzerland) with as much force as possible. The trial was repeated three times. Bite force data were recorded.
Video analysis of dog bite action
To simulate a dog bite as accurately as possible, a hunk of flesh was used to induce a dog bite. The process was recorded by a video camera. Video camera captured views of the dog bite movements. Frame-by-frame video analysis was then used to document the timing and magnitude of behavioral events.
Establishment of the new animal model of dog bite injuries
Four adult New Zealand white rabbits of either gender (age, 20-22 weeks; weight, 2-3 kg) were anesthetized with 30 mg/kg of pentobarbital sodium injected into the external ear vein. To simulate actual dog oral environment, the dog's saliva was collected by setting food before an adult dog to stimulate the production of saliva in this study. The collected saliva was about 10 ml and stored in a clean container. In order to ensure the quality of the saliva and avoid the overdue failure, the saliva was then coated to the jaws of dog bite simulation pliers as soon as possible before the in vivo experiment starts [32]. One researcher simulated the process of a dog biting a rabbit with the dog bite simulation pliers according to the action analysis results. The type and severity of wounds caused by the dog bite simulation pliers were evaluated by the observation. Euthanasia of rabbits was induced by pentobarbital lethal injection.
In vivo study
Twenty adult New Zealand white rabbits of either gender (age, 20-22 weeks; weight, 2-3 kg) were used to validate the reproducibility of the animal model of dog bite injuries. The rabbits were anesthetized with 30 mg/kg of pentobarbital sodium (Nembutal; Bayer, Leverkusen, Germany) injected into the external ear vein and then bit with the dog bite simulation pliers based the above method. Avulsed wounds about 3cm in length and deep to muscles were created on both hind limbs of rabbits. The wounds on the left limb received plastic surgery repair technique by suturing wounds in layers with 4-0 absorbable sutures, and then skin suturing with 5-0 silk sutures in the needle distance of 0.3-0.5cm. The wounds on the right limb received traditional repair technique by suturing wounds directly with 3-0 silk sutures in the needle distance of 1cm. A rubber drainage was put in the wounds and removed at 24 hours after operation. After surgery, the rabbits were given cefaclor (HuaBei Pharma, Hebei, China) at a dose of 20 mg/kg for 3 days. For analgesia, animals were dosed with subcutaneous injection of buprenorphine hydrochloride (0.03 mg/kg; Institute of Pharmaceutical Research, Tianjin, China) once a day for three days. After surgery, animals were housed at suitable room temperature and relative humidity. The wounds were examined daily for 7 days before the sutures were removed. The presence of infection in both groups was recorded. At the end of the fourth week after sutures out, the morphology of the scars was observed. The pigmentation, pliability, and height of the scars were recorded and assessed by a Modified Vancouver Scar Scale (MVSS) [33]. Euthanasia of rabbits was induced by pentobarbital lethal injection.
Statistical Analysis
All quantitative data was expressed as the mean ± standard deviation. For comparison of two groups, statistical analyses were performed using Fisher exact probability test and Kruskal-Wallis test in SPSS 22.0 software (Chicago, Illinois, United States) for Windows (version 18.0.0). A value of P<0.05 was considered to be statistically significant.
Results
Design and production of dog bite simulation pliers
The three-dimensional model of the dog's maxillofacial bones and dentition was reconstructed by MIMICS software (Figure 1). The metallic model was printed with Co-Cr alloy as the jaws of the dog bite simulation pliers. The jaws were consistent with the structure and size of the dog's maxillofacial bones and dentition and exhibited a normal occlusal relationship (Figure 2). The finished dog bite simulation pliers were able to simulate the opening and closing of the dog's mouth (Figure 3).
Three-dimensional digital model of maxillofacial bones and dentition. The images of the maxillofacial bones and dentition of Chinese rural dog were obtained with Mimics16.0.
The jaws of the dog bite simulation pliers. Co-Cr alloy jaw model obtained by 3D printing.

The dog bite simulation pliers. The model was welded on the end of the short handle of a pair of pliers to simulate jaws with correct occlusal contact.

Bite force measurement results of the dog bite simulation pliers
The bite force measured in the study was found to range from 1549 to 1601 Newtons (N), with a mean value of 1579 N (trial 1: 1587N, trial 2:1601 N, trial 3: 1549N).
Dog bite action analysis
Using the video camera evidence, we found that the dog bite was a prolonged and complicated process starting with the dog's sharp teeth puncturing the flesh. Occlusal pressure was then applied as the dog held the flesh in its mouth. The dog shook its head and stepped back while biting to twist, tear, and drag the flesh.
Establishment of the new animal model of dog bite injuries
The tissues of the four rabbits, including the skin, blood vessels, and muscles, were easily punctured or ripped by the dog bite simulation pliers (Figure 4). Different types of injuries, including penetration, laceration and avulsion, were made on the rabbits in actions that simulated a dog bite. All the injuries caused by the pliers were similar to dog bite injures [34]. All potential sites, particularly the craniofacial region which is the most frequently affected area [35], could be selected randomly. The severities of the injuries could be adjusted as the executor wishes.
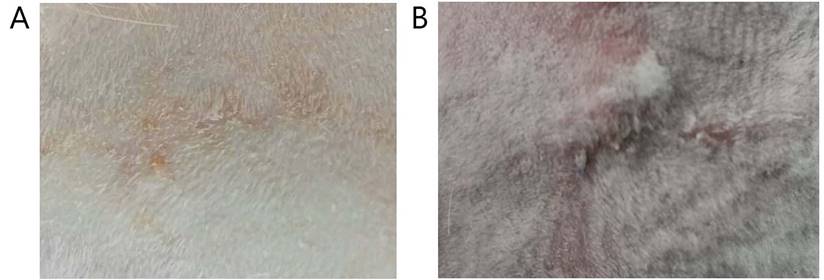
In vivo study
The avulsed wounds were successfully established on nineteen of the twenty rabbits except one rabbit died during induction of anaesthesia. The results showed that all the wounds were made in same type and severity as requested, 3cm in length and deep to muscles. The infection rate of plastic surgery repair technique group was lower than that of traditional repair technique group, but without significant difference (P>0.05) (Table 1). The observation on scar appearance showed that scar tissues in plastic surgery repair technique group were generally smaller and paler compared with that in traditional repair technique group (Figure 5). According to the assessment results of MVSS, the score of scars in plastic surgery repair technique group was lower than that in traditional repair technique group. The difference was statistically significant (P<0.05) (Table 1).
Discussion
Nowadays, dog bites have become a global public health issue [11,12,36,37]. However, the specific treatments of dog bite injuries remain controversial [15-17]. Animal experiments can provide important references for clinical research and practice, and establishment of an animal model is the first key step in performing an animal experiment. Therefore, this study was designed to establish an animal model of dog bite injuries.
In some previous work, the authors proposed using experimental dogs to bite laboratory animals to create an animal model of dog bite injuries. However, it is difficult to control the severity, site, and type of injuries in such animals, in turn making it difficult to conduct a randomized controlled trial in this manner. Moreover, this method leads to high mortality among the animals bitten by the dogs, hindering the establishment of an animal model. Therefore, we designed a new type of instrument that simulates the dog bite process, expecting that this instrument would be helpful in the establishment of an animal model of dog bite injuries. A challenging aspect of this idea is that it is difficult to reconstruct a dog's complicated dentition and maxillofacial bone structure as a model. Fortunately, with the development of computer image processing and selective laser sintering technologies [37,38], it has become possible to reconstruct an accurate simulation model of the dog's maxillofacial bones and dentition.
Infection rate and MVSS score of wounds with two different sutures.
| Plastic surgery repair technique | Traditional repair technique | P values | |
|---|---|---|---|
| Infection (n, %) | 3(15.78%) | 4 (21.05%) | p > 0.05 |
| No infection (n,%) | 16(84.22%) | 15 (78.95%) | |
| MVSS-Sum (means ± standard) | 5.26 ± 1.12 | 8.32 ± 1.84 | p < 0.05 |
Note: MVSS-Sum: Sum of means of MVSS parameters.
The wounds made with the dog bite simulation pliers. The skin and subcutaneous fascia and the muscle tissue of the four rabbits were torn off by the dog bite simulation pliers.

The morphology of the scars. Nineteen of the twenty rabbits were involved. (A) Scar of wound sutured by plastic surgery repair technique. (B) Scar of wound sutured by traditional repair technique.
In this study, the dog involved was a Chinese rural dog. According to the publications, Chinese rural dogs have been blamed for many dog bite cases every year [39]. The data of the dog's skull was obtained by spiral CT scans. A three-dimensional model of the maxillofacial bones and dentition was then built by MIMICS software. The metallic model was printed with Co-Cr alloy by selective laser sintering technology. Therefore, the dog bite simulation pliers developed in the study had highly similarities with the dog's oral and maxillofacial structure. Then, the bite forces of the dog bite simulation pliers were measured. It was found that the bite force of the pliers was strong enough compared to the jaw force that a dog normally had, which was found to range from 13 to 3417 N in previous studies [40,41]. The results suggested that forces provided by the dog bite simulation pliers could match dog bites in strength.
The actions involved in the dog bite process were analyzed and simulated during use of the dog bite simulation pliers. Due to the fact that a large variety of bacteria can be found in a dog's mouth, dog saliva was collected and coated onto the jaws of the new instrument to simulate the actual oral environment of a dog as accurately as possible. Based on these, the animal model of dog bite injuries was established on rabbits with the use of the dog bite simulation pliers. The results showed that the jaws of the pliers were strong and sharp enough to tear rabbits' tissues. As a result, these dog bite simulation pliers could easily be used to create injuries of various severities in rabbits. Additionally, the animal model of dog bite injuries established in this study was highly controllable and totally determined by the controller. More importantly, the injuries were quite similar to dog bites. Finally, the reproducibility of this animal model was validated in the in vivo study. It was found that all the wounds were made in same type and severity on different individual rabbits, indicating that this animal model could be replicated well. Consequently, a new reliable and controllable animal model of dog bite injuries was developed in this study.
The results of the in vivo study also showed that plastic surgery repair technique successfully minimized scarring without increasing the risk of infection, compared to traditional repair technique. These results suggested that plastic surgery repair technique may be a better option in the treatment of dog bite injuries.
In this study, computer image processing technology was used in combination with selective laser sintering technology to develop dog bite simulation pliers for the first time. The use of these digital technologies achieves highly accurate simulation, good controllability, and high convenience required in an animal model of dog bite injuries. This study demonstrated that digital technologies can assist in the establishment of animal models of dog bite injuries, indicating that the method has the potential to be applied to similar research, especially studies involving animal bite models. Although the current study design might be imperfect, it presents an important first step towards such further researches. It will stimulate the interest of other researchers to focus on modification of the animal model of dog bite injuries, and optimal treatment plans.
Conclusions
In conclusion, we have established a new and reliable animal model that may help in further studies on dog bite injuries.
Acknowledgements
Thanks to Dr. Cheng Yang for valuable discussion. Thanks to a dog named Five Million for the production of saliva. This research was funded by National Natural Science Foundation of China, grant number 81670951; and Applied and Basic Research Programs of Sichuan Science and Technology Commission, grant number 2020YJ0278.
Ethics statement
All animal experiment protocols were prospectively approved by the Research Ethics Committee for Laboratory Animal Science of West China Hospital of Stomatology, Sichuan University (Protocol Number: WCHSIRB-D-2017-251). This study was conducted in strict accordance with the recommendations of the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. Animals were housed in a temperature-, humidity-, and air renewal-controlled room. Animals were fed standard dried diet and water. All surgeries were performed under pentobarbital sodium anesthesia (30 mg/kg), and all efforts were made to minimize suffering.
Author contributions
Conceptualization, D.H., W.J. and L.L.; methodology, D.H., W.J., K.L. and Z.L.; software, D.H. and W.J.; validation, D.H., W.J. and K.L.; formal analysis, D.H., W.J., K.L. and Z.L.; investigation, D.H., W.J. and K.L.; resources, L.L.; Data curation, D.H., W.J.; writing—original draft preparation, D.H. and W.J.; writing—review and editing, K.L., Z.L. and L.L.; visualization, D.H., W.J. and L.L.; supervision, L.L.; funding acquisition, L.L.; project administration, L.L. All authors have read and agreed to the published version of the manuscript.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Bula-Rudas FJ, Olcott JL. Human and animal bites. Pediatr Rev. 2018;39(10):490-500 doi: 10.1542/pir.2017-0212
2. Erickson BP, Feng PW, Liao SD. et al. Dog bite injuries of the eye and ocular adnexa. Orbit. 2019;38(1):43-50 doi: 10.1080/01676830.2018.1470190
3. Cook JA, Sasor SE, Soleimani T. et al. An epidemiological analysis of pediatric dog bite injuries over a decade. J Surg Res. 2020;246:231-235 doi: 10.1016/j.jss.2019.09.013
4. Jarvis S. Aiming for elimination of dog-mediated human rabies cases by 2030. Vet Rec. 2016;178(4):86-87 doi: 10.1136/vr.i51
5. Gurunluoglu R, Glasgow M, Arton J. et al. Retrospective analysis of facial dog bite injuries at a Level I trauma center in the Denver metro area. J Trauma Acute Care Surg. 2014;76(5):1294-1300 doi: 10.1097/TA.0000000000000185
6. Monroy A, Behar P, Nagy M. et al. Head and neck dog bites in children. Otolaryngol Head Neck Surg. 2009;140(3):354-357 doi: 10.1016/j.otohns.2008.11.026
7. Overall KL, Love M. Dog bites to humans-demography, epidemiology, injury, and risk. J Am Vet Med Assoc. 2001;218(12):1923-1934 doi: 10.2460/javma.2001.218.1923
8. Abrahamian FM. Dog bites: bacteriology, management, and prevention. Curr Infect Dis Rep. 2000;2(5):446-453 doi: 10.1007/s11908-000-0075-z
9. Rhea S, Weber DJ, Poole C. et al. Risk factors for hospitalization after dog bite injury: a case-cohort study of emergency department visits. Acad Emerg Med. 2014;21(2):196-203 doi: 10.1111/acem.12312
10. Rupprecht CE, Salahuddin N. Current status of human rabies prevention: remaining barriers to global biologics accessibility and disease elimination. Expert Rev Vaccines. 2019;18(6):629-640 doi: 10.1080/14760584.2019.1627205
11. Lin W, Patil PM. Facial dog attack injuries. Indian J Surg. 2015;77(1):55-58 doi: 10.1007/s12262-013-0964-7
12. Oginni FO, Fagade OO, Akinwande JA. et al. Pattern of soft tissue injuries to the oro-facial region in Nigerian children attending a teaching hospital. Int J Paediatr Dent. 2002;12(3):201-206 doi: 10.1046/j.1365-263x.2002.00353
13. Ambro BT, Wright RJ, Heffelfinger RN. Management of bite wounds in the head and neck. Facial Plast Surg. 2010;26(6):456-463 doi: 10.1055/s-0030-1267720
14. Żyluk A. Bite wounds to the hand - a review. Pol Przegl Chir. 2022;94(5):54-59 doi: 10.5604/01.3001.0015.7673
15. Jaindl M, Grünauer J, Platzer P. et al. The management of bite wounds in children-a retrospective analysis at a level I trauma centre. Injury. 2012;43(12):2117-2121 doi: 10.1016/j.injury.2012.04.016
16. Morgan M. Hospital management of animal and human bites. J Hosp Infect. 2005;61(1):1-10 doi: 10.1016/j.jhin.2005.02.007
17. Stevens DL, Bisno AL, Chambers HF. et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):e10-e52 doi: 10.1093/cid/ciu444
18. Hurt JB, Maday KR. Management and treatment of animal bites. JAAPA. 2018;31(4):27-31 doi: 10.1097/01.JAA.0000531049.59137.cd
19. Greene SE, Fritz SA. Infectious complications of bite injuries. Infect Dis Clin North Am. 2021;35(1):219-236 doi: 10.1016/j.idc.2020.10.005
20. Chu AS, Harkness J. Alcaligenes faecalis cellulitis after a dog bite: case report and literature review. Pediatr Emerg Care. 2017;33(7):497-498 doi: 10.1097/PEC.0000000000000645
21. Di Bari S, Gavaruzzi F, De Meo D. et al. Candida parapsilosis osteomyelitis following dog bite: a case report and review of the literature. J Mycol Med. 2022;32(1):101208 doi: 10.1016/j.mycmed.2021.101208
22. Aziz H, Rhee P, Pandit V. et al. The current concepts in management of animal (dog, cat, snake, scorpion) and human bite wounds. J Trauma Acute Care Surg. 2015;78(3):641-648 doi: 10.1097/TA.0000000000000531
23. Minato S, Sukegawa K, Onuma K. et al. Polymicrobial extensor tenosynovitis including mycobacterium chelonae caused by a dog bite: a case report. JBJS Case Connect. 2021;11(1):e20.00608 doi: 10.2106/JBJS.CC.20.00608
24. Senturk E, Dagistanli N, Calim OF. et al. Nasal reconstruction following a dog bite. J Craniofac Surg. 2019;30(7):2233-2235 doi: 10.1097/SCS.0000000000005965
25. Hwang K, Ma SH. A nasal bone fracture caused by a dog bite in an adult. J Craniofac Surg. 2021;32(7):e630-e632.doi 10.1097/SCS.0000000000007604
26. Zangari A, Cerigioni E, Nino F. et al. Dog bite injuries in a tertiary care children's hospital: a seven-year review. Pediatr Int. 2021;63(5):575-580 doi: 10.1111/ped.14484
27. Rothe K, Tsokos M, Handrick W. Animal and human bite wounds. Dtsch Arztebl Int. 2015;112(25):433-442 doi: 10.3238/arztebl.2015.0433
28. Duncan-Sutherland N, Lissaman AC, Shepherd M. et al. Systematic review of dog bite prevention strategies. Inj Prev. 2022;28(3):288-297 doi: 10.1136/injuryprev-2021-044477
29. Lee CJ, Tiourin E, Schuljak S. et al. Surgical treatment of pediatric dog-bite wounds: a 5-year retrospective review. West J Emerg Med. 2021;22(6):1301-1310 doi: 10.5811/westjem.2021.9.52235
30. Mendoza JM, Chi JJ. Reconstruction of animal bite injuries to the head and neck. Curr Opin Otolaryngol Head Neck Surg. 2019;27(5):407-412 doi: 10.1097/MOO.0000000000000564
31. Reclaru L, Ardelean L, Rusu LC. et al. Co-Cr material selection in prosthetic restoration: laser sintering technology. Solid State Phenom. 2012;188:412-415 doi: 10.4028/www.scientific.net/SSP.188.412
32. Talan DA, Citron DM, Abrahamian FM. et al. Bacteriologic analysis of infected dog and cat bites. Emergency Medicine Animal Bite Infection Study Group. N Engl J Med. 1999;340(2):85-92 doi: 10.1056/NEJM199901143400202
33. Baryza MJ, Baryza GA. The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil. 1995;16(5):535-538 doi: 10.1097/00004630-199509000-00013
34. Means O, Fernstrum C, Lucich E. et al. Management of dog bite injuries: procedural sedation, infection, and operative indications at a single-institution Level I pediatric trauma hospital. Ann Plast Surg. 2023;90(1):71-75 doi: 10.1097/SAP.0000000000003362
35. Copana-Olmos R, Calderón-López ME, Jove-Veizaga A. et al. Dog bite injuries in children seen at a tertiary care hospital in Bolivia. Arch Argent Pediatr. 2023;121(6):e202202928 doi: 10.5546/aap.2022-02928
36. Gottlieb M, Peksa GD. Prophylactic antibiotics are not routinely indicated for dog bites. Ann Emerg Med. 2020;76(1):86-87 doi: 10.1016/j.annemergmed.2020.01.030
37. Ghosh U, Ning S, Wang Y. et al. Addressing unmet clinical needs with 3D printing technologies. Adv Healthc Mater. 2018;7(17):e1800417 doi: 10.1002/adhm.201800417
38. Charoo NA, Barakh Ali SF, Mohamed EM. et al. Selective laser sintering 3D printing - an overview of the technology and pharmaceutical applications. Drug Dev Ind Pharm. 2020;46(6):869-877 doi: 10.1080/03639045.2020.1764027
39. Shen J, Pang S, Schwebel DC. A randomized trial evaluating child dog-bite prevention in rural China through video-based testimonials. Health Psychol. 2016;35(5):454-464 doi: 10.1037/hea0000273
40. Kim SE, Arzi B, Garcia TC. et al. Bite forces and their measurement in dogs and cats. Front Vet Sci. 2018;5:76 doi: 10.3389/fvets.2018.00076
41. Brassard C, Merlin M, Guintard C. et al. Bite force and its relationship to jaw shape in domestic dogs. J Exp Biol. 2020;223(16):jeb224352 doi: 10.1242/jeb.224352
Author contact
![]() Corresponding author: Prof. Lei Liu, E-mail: liuleiedu.cn
Corresponding author: Prof. Lei Liu, E-mail: liuleiedu.cn

 Global reach, higher impact
Global reach, higher impact