3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(4):765-774. doi:10.7150/ijms.92993 This issue Cite
Research Paper
Proteomics-based Model for Predicting the Risk of Brain Metastasis in Patients with Resected Lung Adenocarcinoma carrying the EGFR Mutation
1. Department of Clinical Laboratory, the First Affiliated Hospital of Guangzhou Medical University, National Center for Respiratory Medicine, Guangzhou 510120, China.
2. Department of Thoracic Oncology, the First Affiliated Hospital of Guangzhou Medical University, State Key Laboratory of Respiratory Diseases, National Clinical Research Center of Respiratory Disease, Guangzhou 510120, China.
3. Tianjin Key Laboratory of Clinical Multi-Omics, Tianjin 300308, China.
* These authors contributed equally to this work.
Abstract
Introduction: Epidermal growth factor receptor (EGFR) mutation is common in Chinese patients with lung adenocarcinoma (LUAD). Brain metastases (BMs) is high and associated with poor prognosis. Identification of EGFR-mutant patients at high risk of developing BMs is important to reduce or delay the incidence of BMs. Currently, there is no literature on the prediction and modeling of EGFR brain metastasis at the proteinomics level.
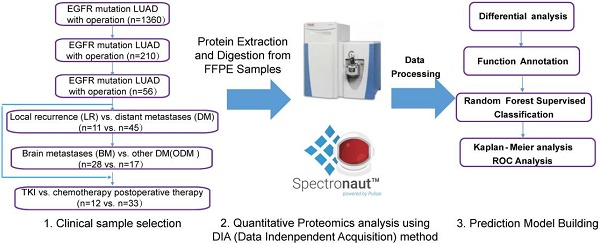
Methods: We conducted a retrospective study of BMs in postoperative recurrent LUAD with EGFR mutation in the First Affiliated Hospital of Guangzhou Medical University. Tissue proteomic analysis was applied in the primary tumors of resected LUAD in this study using liquid chromatography-mass spectrometry (LC-MS/MS). To identify potential markers for predicting LUAD BM, comparative analyses were performed on different groups to evaluate proteins associated with high risk of BMs.
Results: A combination of three potential marker proteins was found to discriminate well between distal metastasis (DM) and local recurrence (LR) of postoperative LUAD with EGFR mutation. Gene Ontology (GO) analysis of significantly altered proteins between BM and non-BM (NBM) indicated that lipid metabolism and cell cycle-related pathways were involved in BMs of LUAD. And the enriched pathways correlated with BMs were found to be quite different in the comparison groups of postoperative adjuvant therapy, tyrosine kinase inhibitor (TKI), and chemotherapy groups. Finally, we developed a random forest algorithm model with eight proteins (RRS1, CPT1A, DNM1, SRCAP, MLYCD, PCID2, IMPAD1 and FILIP1), which showed excellent predictive value (AUC: 0.9401) of BM in patients with LUAD harboring EGFR mutation.
Conclusions: A predictive model based on protein markers was developed to accurately predict postoperative BM in operable LUAD harboring EGFR mutation.
Keywords: Lung adenocarcinoma, brain metastasis, proteome, EGFR mutation, risk prediction

 Global reach, higher impact
Global reach, higher impact