3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2022; 19(11):1660-1671. doi:10.7150/ijms.75824 This issue Cite
Research Paper
Interactive effect of obesity and cognitive function decline on the risk of chronic kidney disease progression in patients with type 2 diabetes mellitus: a 9.1-year cohort study
1. Division of Endocrinology and Metabolism, Department of Internal Medicine, E-Da Hospital, Kaohsiung 82445 Taiwan.
2. School of Medicine for International Students, College of Medicine, I-Shou University, Kaohsiung 82445 Taiwan.
3. Division of Cardiology, Department of Internal Medicine, E-Da Hospital, Kaohsiung 82445 Taiwan.
4. School of Medicine, College of Medicine, I-Shou University, Kaohsiung 82445 Taiwan.
5. Division of Gastroenterology and Hepatology, Department of Internal Medicine, E-Da Hospital, Kaohsiung, 82445 Taiwan.
6. The School of Chinese Medicine for Post Baccalaureate, College of Medicine, I-Shou University, Kaohsiung, 82445 Taiwan.
7. Division of General Surgery, Department of Surgery, E-Da Hospital, Kaohsiung, 82445 Taiwan.
8. Department of Biomedical Engineering, I-Shou University, Kaohsiung, 82445 Taiwan.
9. Department of Electrical Engineering, I-Shou University, Kaohsiung, 82445 Taiwan.
10. Lee's Endocrinologic Clinic, Pingtung 90000 Taiwan.
11. Division of Cardiology, Department of Internal Medicine, Taipei Veterans General Hospital, Yuli Branch, Hualien 98142 Taiwan.
12. Faculty of Medicine, School of Medicine, National Yang Ming Chiao Tung University, Taipei 112304 Taiwan.
*These authors contributed equally to this work.
Abstract
Background: Obesity and cognitive function decline are independent risk factors for chronic kidney disease (CKD). However, few studies have examined the combined effects of obesity status and cognitive function on change in CKD risk. We aimed to evaluate the association between obesity status, cognitive function and CKD risk change in patients with type 2 diabetes mellitus (T2DM).
Methods: Data on 3399 T2DM patients were extracted from a diabetes disease management program between 2006 and 2018. Univariate and multivariate analyses were used to assess the association between obesity, cognitive decline, and CKD risk change. Three indexes, including the relative excess risk of interaction (RERI), attributable proportion of interaction (API), and synergy index (SI), were used to analyze interactions. CKD risk was classified according to the KDIGO 2012 CKD definition.
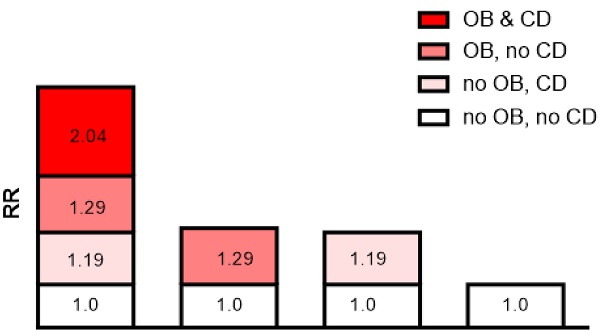
Results: In multivariate analysis, the hazard ratio (HR, 95%Cis) for CKD risk progression was 1.34 (1.12-1.61) times higher in the moderate and severely obese patients compared with the normal weight patients, and 1.34 (1.06-1.67) times higher in the patients with a Mini-Mental State Examination (MMSE) score ≤18 compared to those with an MMSE score ≥24. There was a synergistic interaction between moderate and severe obesity and MMSE score ≤18 on CKD risk progression (SI=4.461; 95% CI: 1.998-9.962), and the proportion of CKD risk progression caused by this interaction was 52.7% (API=0.527; 95% CI: 0.295-0.759). However, normal weight and MMSE score ≥24 were not beneficial on CKD risk improvement in the patients with a moderate risk and very high-risk stage of CKD.
Conclusion: There may be a synergistic interaction between obesity and cognitive function decline, and the synergistic interaction may increase the risk of CKD progression.
Keywords: Chronic kidney disease risk, cognitive function decline, obesity, synergistic interaction, type 2 diabetes mellitus.

 Global reach, higher impact
Global reach, higher impact