Impact Factor
ISSN: 1449-1907
Int J Med Sci 2022; 19(7):1118-1121. doi:10.7150/ijms.72772 This issue Cite
Review
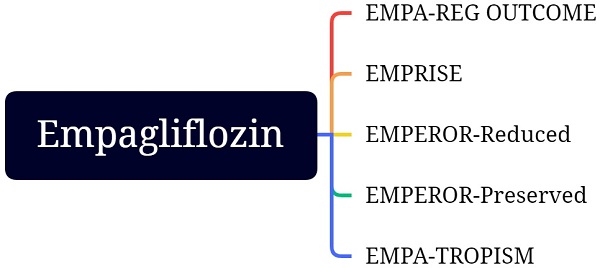
Empagliflozin in the treatment of heart failure and type 2 diabetes mellitus: Evidence from several large clinical trials
1. Nanjing University of Chinese Medicine, Nanjing, China.
2. Department of Cardiology, The Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China.
3. Nanjing Hospital of Chinese Medicine Affiliated to Nanjing University of Chinese Medicine, Nanjing, China.
Received 2022-3-10; Accepted 2022-6-7; Published 2022-6-21
Abstract
Heart failure coexists with type 2 diabetes mellitus, which seriously affects the clinical treatment and prognosis. At present, the treatment for patients with established heart failure and type 2 diabetes mellitus is usually combined with two treatment strategies for heart failure and type 2 diabetes mellitus. Recently, increasing studies showed that empagliflozin, a sodium-glucose co-transporter-2 inhibitor, has a positive effect on the treatment of patients with established heart failure and type 2 diabetes mellitus. Here, we summarize the latest and current understanding of the management for patients with established heart failure and type 2 diabetes mellitus and further present contemporary treatment options, sodium-glucose co-transporter-2 inhibitor, for these particular populations.
Keywords: empagliflozin, SGLT2i, heart failure, type 2 diabetes mellitus
Introduction
Heart failure (HF) and type 2 diabetes mellitus (T2DM) are common medical diseases [1, 2], especially among the elderly. Two diseases are usually diagnosed in the same patient at the same time, which undoubtedly increases the difficulty of clinical management and worsens the prognosis of patients [3, 4]. The clinical condition of patients with T2DM complicated with HF, both HF with reduced ejection fraction (HFrEF) and HF with preserved ejection fraction (HFpEF), is worse than that of patients with HF without T2DM, and all-cause mortality and cardiovascular mortality are higher [5-7]. In another word, T2DM exacerbates the prognosis of HF. Moreover, studies show that HF is an independent predictor of clinical prognosis, whether fatal or nonfatal, in diabetic patients [8-11]. The interaction between HF and T2DM makes the prognosis of patients more unsatisfactory.
When a patient is diagnosed with HF and T2DM at the same time, our current understanding is that, in general, all HF treatments are similarly effective irrespective of T2DM. In recent years, many hypoglycemic drugs, such as sodium-glucose co-transporter-2 inhibitors (SGLT-2is), have emerged in the treatment of HF. Although the potential benefits and risks of SGLT-2is are unclear [12], SGLT-2is significantly reduce cardiovascular events, including hospitalization for HF and all-cause hospitalization or death [13-17]. Scandinavian register-based cohort study indicated that SGLT-2i lowers HF risk compared with dipeptidyl peptidase-4 inhibitor [18], another glucose-lowering drug. This benefit from SGLT-2i may contribute to the upregulation of the renin-angiotensin-aldosterone system [19]. Empagliflozin, an SGLT2i, significantly reduces hospitalization for HF in patients with established cardiovascular disease or at risk of cardiovascular disease and improves cardiac function in HFrEF independent of loading conditions [20]. The latest guideline recommended that empagliflozin should be considered in patients with T2DM and either established cardiovascular disease or at high cardiovascular risk to delay or prevent the onset of HF or prolong life [21]. A meta-analysis also indicated that compared with placebo, empagliflozin reduced all-cause and cardiovascular mortality independent of baseline risk [22]. Of note, few trials supported the recommendation where the presence of HF at baseline was well-characterized or phenotyped, indicating that evidence supporting empagliflozin for patients with HF and T2DM is still insufficient. Here, we critically review and distill contemporary evidence of empagliflozin for treating established HF and T2DM, with a view to provide a more systematic, comprehensive and rational understanding of this treatment option.
EMPA-REG OUTCOME
EMPA-REG OUTCOME was conducted to assess the effect of empagliflozin on cardiovascular events in adults with T2DM at high cardiovascular risk [23]. The primary outcome was cardiovascular mortality, nonfatal myocardial infarction, or nonfatal stroke, and the key secondary composite outcome was the primary outcome plus hospitalization for unstable angina. After a median observation time of 3.1 years, patients in the empagliflozin group reduced the primary outcome and the key secondary composite outcome compared with those in the placebo group. Moreover, empagliflozin significantly lowered hospitalization for HF, cardiovascular mortality, and all-cause mortality than placebo, whereas reduced nonfatal myocardial infarction and nonfatal stroke with no significance to placebo. In short, EMPA-REG OUTCOME demonstrated that empagliflozin reduced hospitalization for HF risk on top of the standard of care in patients with T2DM and established cardiovascular disease [24]. The post hoc evaluation showed that the changes in hematocrit and hemoglobin were the most important mediators of the reduction in hospitalization for HF and death from HF [25].
EMPRISE
EMPRISE used real-world data from three databases in the USA to evaluate the effectiveness, safety, and impact on healthcare utilization of empagliflozin [26]. The interim analysis of EMPRISE evaluated the impact of empagliflozin on hospitalization for HF and compared it with sitagliptin, a dipeptidyl peptidase-4 inhibitor, which has proven to have a neutral impact on hospitalization for HF [27]. Among included patients, only approximately 5% had existing HF. Over a mean follow-up of 5.3 months, the initiation of empagliflozin decreased hospitalization for HF compared with the initiation of sitagliptin. Moreover, some patients with no history of HF developed HF during the follow-up, and empagliflozin reduced hospitalization for HF regardless of the history of HF [26].
EMPEROR-Reduced
EMPEROR-Reduced determined whether empagliflozin significantly increased the clinical benefit of HFrEF patients [28]. EMPEROR-Reduced indicated that empagliflozin significantly lowered hospitalization for HF and cardiovascular mortality than placebo, with or without T2DM [29].
EMPEROR-Preserved
EMPEROR-Preserved enrolled 5988 patients with HFpEF, with and without T2DM. EMPEROR-Preserved indicated that empagliflozin reduced hospitalization for HF and cardiovascular mortality [30].
EMPA-TROPISM
EMPA-TROPISM compared the efficacy of and safety of empagliflozin in non-diabetic HFrEF (left ventricular ejection fraction < 50%) patients [31]. Empagliflozin significantly improved left ventricular end-diastolic and end-systolic volumes decreased left ventricular mass, increased left ventricular ejection fraction, enhanced functional capacity as per peak O2 consumption oxygen uptake efficiency slope, and 6-min walk test, and improved quality of life as per the Kansas City Cardiomyopathy Questionnaire-12 when compared with placebo [32]. EMPA-TROPISM also demonstrated that empagliflozin regressed left ventricular interstitial fibrosis, improved aortic stiffness, regressed epicardial adipose tissue, and exerted an anti-inflammatory effect [33], which provides a new clue for the mechanism of empagliflozin.
Discussion
EMPA-REG OUTCOME, EMPRISE, EMPEROR-Reduced, and EMPEROR-Preserved all showed that empagliflozin reduces the risk of hospitalization for HF among specific individuals. EMPA-TROPISM provides something new about the mechanism of empagliflozin. Nevertheless, these patients included in the trials did not have an established HF combined with T2DM or the degree of HF combined with T2DM was low at baseline, indicating the evidence of the clinical benefits of empagliflozin on HF patients combined with T2DM are still not sufficient, therefore, long-term clinical exploration including both HF with T2DM patients is needed.
At present, the evidence for empagliflozin in the treatment of HFpEF is still sparse [34]. The prevalence of HFpEF increases with age [35]. The increased risk of hospitalization for HF might be explained by the occurrence of multiple comorbidities in older adults with HFpEF [36]. However, EMPEROR-Preserved did not include the total comorbidity burden as a covariate in their analysis [37]. A prospective study was designed to assess the cognitive and physical function in consecutive frail older adults with diabetes and HFpEF, indicating empagliflozin improved Montreal cognitive assessment scores and physical impairment assessed by the 5-m gait speed test [38]. EMPEROR-Preserved also confirmed that health status, as measured by the Kansas City Cardiomyopathy Questionnaire, improved at all time points when assessed (3, 8, and 12 months) for all domains (total symptom score, clinical summary score, and overall summary score[39]. Despite this, the benefits of empagliflozin were observed early and consistently. The nominal statistical significance was achieved for separation between the empagliflozin and the placebo arms by day 18 for time to cardiovascular death or hospitalization for HF, and this significance was sustained from there to the trial period [40]. A similar pattern of early and sustained benefit was seen for health-related quality of life scores, the Kansas City Cardiomyopathy Questionnaire (total symptom score, clinical summary score, and overall summary score), and New York Heart Association functional class as well [41]. Similarly, in EMPA-REG OUTCOME, the benefit of empagliflozin in reducing the risk of hospitalization for HF and cardiovascular death emerged within weeks after treatment initiation [42]. The simplest explanation for such fast and short-term effects of empagliflozin in HFpEF is its diuretic effect [43]. However, the diuretic effect of empagliflozin is different from loop diuretics in that empagliflozin caused a significant increase in 24-hour urine volume without an increase in urinary sodium and electrolyte-free water clearance [44] and a significant decrease in estimated plasma volume calculated by the Straus formula and estimated the extracellular volume determined by the body surface area [45]. A pooled analysis of both the EMPEROR-Reduced and EMPEROR-Preserved trials indicated that the magnitude of the effect of empagliflozin on HF outcomes and health status was similar in patients with ejection fractions < 25% to < 65%, but it was attenuated in patients with an ejection fraction ≥ 65% [46], which may herald the recognition of a new phenotype characterized by supra-normal left ventricular ejection fraction [47].
We critically review several large clinical trials about empagliflozin, however, empagliflozin was not originally developed for HF and T2DM, the inclusion population is not particularly targeted in these trials, and any recommendation for the treatment of established HF and T2DM will be necessarily cautious. Additionally, well-designed clinical trials with long follow-ups may provide us with more valuable information.
Abbreviations
Heart failure: HF; type 2 diabetes mellitus: T2DM; heart failure with reduced ejection fraction: HFrEF; heart failure with preserved ejection fraction: HFpEF; sodium-glucose co-transporter-2 inhibitor: SGLT-2i.
Acknowledgements
We thank all scientists and participants involved in empagliflozin and HF. This study was partly funded by National Natural Science Foundation of China [81774229], Jiangsu Leading Talent Project of Traditional Chinese Medicine [Jiangsu TCM 2018 No. 4], and Nanjing Municipal Health Science and Technology Development Special Fund [ZKX21060].
Author contributions
BL and NG conceived, designed, or planned the idea. All authors collected and read the literature. BL drafted the manuscript. NG revised the manuscript. All authors read and approved the final manuscript.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Lehrke M, Marx N. Diabetes Mellitus and Heart Failure. The American Journal of Medicine. 2017;130:S40-S50
2. Jankauskas SS, Kansakar U, Varzideh F, Wilson S, Mone P, Lombardi A. et al. Heart failure in diabetes. Metabolism. 2021;125:154910
3. Seferović PM, Petrie MC, Filippatos GS, Anker SD, Rosano G, Bauersachs J. et al. Type 2 diabetes mellitus and heart failure: a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018;20:853-72
4. Liang B, Zhao Y-X, Zhang X-X, Liao H-L, Gu N. Reappraisal on pharmacological and mechanical treatments of heart failure. Cardiovasc Diabetol. 2020;19:55
5. MacDonald MR, Petrie MC, Varyani F, Ostergren J, Michelson EL, Young JB. et al. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur Heart J. 2008;29:1377-85
6. Seferović PM, Coats AJS, Ponikowski P, Filippatos G, Huelsmann M, Jhund PS. et al. European Society of Cardiology/Heart Failure Association position paper on the role and safety of new glucose-lowering drugs in patients with heart failure. Eur J Heart Fail. 2020;22:196-213
7. McHugh K, DeVore AD, Wu J, Matsouaka RA, Fonarow GC, Heidenreich PA. et al. Heart Failure With Preserved Ejection Fraction and Diabetes: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73:602-11
8. MacDonald MR, Petrie MC, Hawkins NM, Petrie JR, Fisher M, McKelvie R. et al. Diabetes, left ventricular systolic dysfunction, and chronic heart failure. Eur Heart J. 2008;29:1224-40
9. Seong J-M, Kim JJ, Kim HJ, Sohn HS. Comparison of heart failure risk and medical costs between patients with type 2 diabetes mellitus treated with dapagliflozin and dipeptidyl peptidase-4 inhibitors: a nationwide population-based cohort study. Cardiovasc Diabetol. 2020;19:95
10. Vaur L, Gueret P, Lievre M, Chabaud S, Passa P. Development of congestive heart failure in type 2 diabetic patients with microalbuminuria or proteinuria: observations from the DIABHYCAR (type 2 DIABetes, Hypertension, CArdiovascular Events and Ramipril) study. Diabetes Care. 2003;26:855-60
11. Tanaka H, Tatsumi K, Matsuzoe H, Matsumoto K, Hirata K-I. Impact of diabetes mellitus on left ventricular longitudinal function of patients with non-ischemic dilated cardiomyopathy. Cardiovasc Diabetol. 2020;19:84
12. Udell JA, Yuan Z, Rush T, Sicignano NM, Galitz M, Rosenthal N. Cardiovascular Outcomes and Risks After Initiation of a Sodium Glucose Cotransporter 2 Inhibitor: Results From the EASEL Population-Based Cohort Study (Evidence for Cardiovascular Outcomes With Sodium Glucose Cotransporter 2 Inhibitors in the Real World). Circulation. 2018;137:1450-9
13. Kosiborod M, Lam CSP, Kohsaka S, Kim DJ, Karasik A, Shaw J. et al. Cardiovascular Events Associated With SGLT-2 Inhibitors Versus Other Glucose-Lowering Drugs: The CVD-REAL 2 Study. J Am Coll Cardiol. 2018;71:2628-39
14. Kosiborod M, Cavender MA, Fu AZ, Wilding JP, Khunti K, Holl RW. et al. Lower Risk of Heart Failure and Death in Patients Initiated on Sodium-Glucose Cotransporter-2 Inhibitors Versus Other Glucose-Lowering Drugs: The CVD-REAL Study (Comparative Effectiveness of Cardiovascular Outcomes in New Users of Sodium-Glucose Cotransporter-2 Inhibitors). Circulation. 2017;136:249-59
15. Giugliano D, Longo M, Scappaticcio L, Bellastella G, Maiorino MI, Esposito K. SGLT-2 inhibitors and cardiorenal outcomes in patients with or without type 2 diabetes: a meta-analysis of 11 CVOTs. Cardiovasc Diabetol. 2021;20:236
16. Real J, Vlacho B, Ortega E, Vallés JA, Mata-Cases M, Castelblanco E. et al. Cardiovascular and mortality benefits of sodium-glucose co-transporter-2 inhibitors in patients with type 2 diabetes mellitus: CVD-Real Catalonia. Cardiovasc Diabetol. 2021;20:139
17. Thomsen RW, Knudsen JS, Kahlert J, Baggesen LM, Lajer M, Holmgaard PH. et al. Cardiovascular Events, Acute Hospitalizations, and Mortality in Patients With Type 2 Diabetes Mellitus Who Initiate Empagliflozin Versus Liraglutide: A Comparative Effectiveness Study. Journal of the American Heart Association. 2021;10:e019356
18. Pasternak B, Ueda P, Eliasson B, Svensson A-M, Franzén S, Gudbjörnsdottir S. et al. Use of sodium glucose cotransporter 2 inhibitors and risk of major cardiovascular events and heart failure: Scandinavian register based cohort study. BMJ. 2019;366:l4772
19. Schork A, Saynisch J, Vosseler A, Jaghutriz BA, Heyne N, Peter A. et al. Effect of SGLT2 inhibitors on body composition, fluid status and renin-angiotensin-aldosterone system in type 2 diabetes: a prospective study using bioimpedance spectroscopy. Cardiovasc Diabetol. 2019;18:46
20. Liang B, Zhao Y-X, Gu N. Empagliflozin improves cardiac function in heart failure with reduced ejection fraction independent of loading conditions. Cardiovasc Diabetol. 2020;19:29
21. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM. et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:1757-80
22. Odutayo A, da Costa BR, Pereira TV, Garg V, Iskander S, Roble F. et al. Sodium-Glucose Cotransporter 2 Inhibitors, All-Cause Mortality, and Cardiovascular Outcomes in Adults with Type 2 Diabetes: A Bayesian Meta-Analysis and Meta-Regression. Journal of the American Heart Association. 2021;10:e019918-e
23. Zinman B, Inzucchi SE, Lachin JM, Wanner C, Ferrari R, Fitchett D. et al. Rationale, design, and baseline characteristics of a randomized, placebo-controlled cardiovascular outcome trial of empagliflozin (EMPA-REG OUTCOME™). Cardiovasc Diabetol. 2014;13:102
24. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S. et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. The New England journal of medicine. 2015;373:2117-28
25. Fitchett D, Inzucchi SE, Zinman B, Wanner C, Schumacher M, Schmoor C. et al. Mediators of the improvement in heart failure outcomes with empagliflozin in the EMPA-REG OUTCOME trial. ESC Heart Fail. 2021;8:4517-27
26. Patorno E, Pawar A, Franklin JM, Najafzadeh M, Déruaz-Luyet A, Brodovicz KG. et al. Empagliflozin and the Risk of Heart Failure Hospitalization in Routine Clinical Care. Circulation. 2019;139:2822-30
27. Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J. et al. Effect of Sitagliptin on Cardiovascular Outcomes in Type 2 Diabetes. The New England journal of medicine. 2015;373:232-42
28. Packer M, Butler J, Filippatos GS, Jamal W, Salsali A, Schnee J. et al. Evaluation of the effect of sodium-glucose co-transporter 2 inhibition with empagliflozin on morbidity and mortality of patients with chronic heart failure and a reduced ejection fraction: rationale for and design of the EMPEROR-Reduced trial. Eur J Heart Fail. 2019;21:1270-8
29. Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P. et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. The New England journal of medicine. 2020;383:1413-24
30. Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M. et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. The New England journal of medicine. 2021;385:1451-61
31. Santos-Gallego CG, Garcia-Ropero A, Mancini D, Pinney SP, Contreras JP, Fergus I. et al. Rationale and Design of the EMPA-TROPISM Trial (ATRU-4): Are the "Cardiac Benefits" of Empagliflozin Independent of its Hypoglycemic Activity? Cardiovasc Drugs Ther. 2019;33:87-95
32. Santos-Gallego CG, Vargas-Delgado AP, Requena-Ibanez JA, Garcia-Ropero A, Mancini D, Pinney S. et al. Randomized Trial of Empagliflozin in Nondiabetic Patients With Heart Failure and Reduced Ejection Fraction. J Am Coll Cardiol. 2021;77:243-55
33. Requena-Ibáñez JA, Santos-Gallego CG, Rodriguez-Cordero A, Vargas-Delgado AP, Mancini D, Sartori S. et al. Mechanistic Insights of Empagliflozin in Nondiabetic Patients With HFrEF: From the EMPA-TROPISM Study. JACC Heart Fail. 2021;9:578-89
34. Liang B, Gu N. Sodium-glucose co-transporter-2 inhibitors in the treatment of diabetes with heart failure. Cardiovasc Diabetol. 2022;21:84
35. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS. et al. Heart Disease and Stroke Statistics—2022 Update: A Report From the American Heart Association. Circulation. 2022;145:e153-e639
36. Tisminetzky M, Gurwitz JH, Fan D, Reynolds K, Smith DH, Magid DJ. et al. Multimorbidity Burden and Adverse Outcomes in a Community-Based Cohort of Adults with Heart Failure. J Am Geriatr Soc. 2018;66:2305-13
37. Hias J, Hellemans L, Walgraeve K, Tournoy J, Van der Linden L. SGLT2 Inhibitors in Older Adults with Heart Failure with Preserved Ejection Fraction. Drugs Aging. 2022;39:185-90
38. Mone P, Lombardi A, Gambardella J, Pansini A, Macina G, Morgante M. et al. Empagliflozin Improves Cognitive Impairment in Frail Older Adults With Type 2 Diabetes and Heart Failure With Preserved Ejection Fraction. Diabetes Care. 2022;45:1247-51
39. Butler J, Filippatos G, Jamal Siddiqi T, Brueckmann M, Böhm M, Chopra VK. et al. Empagliflozin, Health Status, and Quality of Life in Patients With Heart Failure and Preserved Ejection Fraction: The EMPEROR-Preserved Trial. Circulation. 2022;145:184-93
40. Packer M, Butler J, Zannad F, Filippatos G, Ferreira JP, Pocock SJ. et al. Effect of Empagliflozin on Worsening Heart Failure Events in Patients With Heart Failure and Preserved Ejection Fraction: EMPEROR-Preserved Trial. Circulation. 2021;144:1284-94
41. Butler J, Siddiqi TJ, Filippatos G, Ferreira JP, Pocock SJ, Zannad F. et al. Early benefit with empagliflozin in heart failure with preserved ejection fraction: insights from the EMPEROR-Preserved trial. Eur J Heart Fail. 2022;24:245-8
42. Verma S, Leiter LA, Zinman B, Sharma A, Mattheus M, Fitchett D. et al. Time to cardiovascular benefits of empagliflozin: a post hoc observation from the EMPA-REG OUTCOME trial. ESC Heart Fail. 2021;8:2603-7
43. Kokhan E, Kiyakbaev G, Medovchshikov V. Sodium-glucose co-transporter 2 inhibitors: drugs with multiple effects, but which one is relevant to heart failure with preserved ejection fraction? Letter regarding the article 'Early benefit with empagliflozin in heart failure with preserved ejection fraction: insights from the EMPEROR-Preserved trial'. Eur J Heart Fail. 2022 n/a
44. Mordi NA, Mordi IR, Singh JS, McCrimmon RJ, Struthers AD, Lang CC. Renal and Cardiovascular Effects of SGLT2 Inhibition in Combination With Loop Diuretics in Patients With Type 2 Diabetes and Chronic Heart Failure: The RECEDE-CHF Trial. Circulation. 2020;142:1713-24
45. Tanaka A, Shimabukuro M, Teragawa H, Okada Y, Takamura T, Taguchi I. et al. Reduction of estimated fluid volumes following initiation of empagliflozin in patients with type 2 diabetes and cardiovascular disease: a secondary analysis of the placebo-controlled, randomized EMBLEM trial. Cardiovasc Diabetol. 2021;20:105
46. Butler J, Packer M, Filippatos G, Ferreira JP, Zeller C, Schnee J. et al. Effect of empagliflozin in patients with heart failure across the spectrum of left ventricular ejection fraction. Eur Heart J. 2022;43:416-26
47. Wehner GJ, Jing L, Haggerty CM, Suever JD, Leader JB, Hartzel DN. et al. Routinely reported ejection fraction and mortality in clinical practice: where does the nadir of risk lie? Eur Heart J. 2020;41:1249-57
Author contact
![]() Corresponding author: Ning Gu, guningedu.cn
Corresponding author: Ning Gu, guningedu.cn

 Global reach, higher impact
Global reach, higher impact