3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2021; 18(16):3788-3793. doi:10.7150/ijms.61779 This issue Cite
Review
Cytidine deamination-induced perpetual immunity to SAR-CoV-2 infection is a potential new therapeutic target
1. Department of Radiation Oncology, School of Medicine, University of California San Francisco, San Francisco, California, USA.
2. Department of Pediatrics, University of Alberta, Edmonton, Alberta, Canada.
3. Department of Clinical & Diagnostic Sciences, The University of Alabama at Birmingham, Birmingham, AL, USA.
4. Cardiovascular Research Institute, School of Medicine, University of California San Francisco, San Francisco, California, USA.
5. Department of Immunology and Transplantation, School of Medicine, Stanford University, Stanford, California, USA.
Abstract
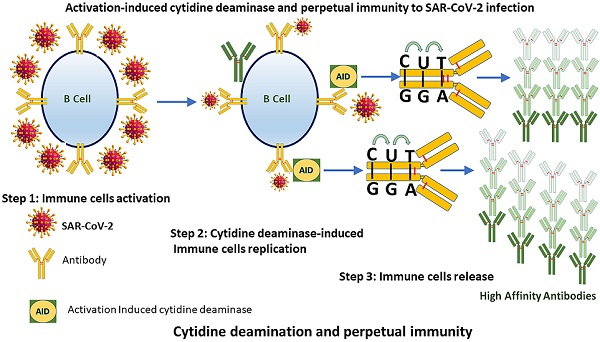
As the world is racing to develop perpetual immunity to the SARS-CoV-2 virus. The emergence of new viral strains, together with vaccination and reinfections, are all contributing to a long-term immunity against the deadly virus that has taken over the world since its introduction to humans in late December 2019. The discovery that more than 95 percent of people who recovered from COVID-19 had long-lasting immunity and that asymptomatic people have a different immune response to SARS-CoV-2 than symptomatic people has shifted attention to how our immune system initiates such diverse responses. These findings have provided reason to believe that SARS-CoV-2 days are numbered. Hundreds of research papers have been published on the causes of long-lasting immune responses and variations in the numbers of different immune cell types in COVID 19 survivors, but the main reason of these differences has still not been adequately identified. In this article, we focus on the activation-induced cytidine deaminase (AID), which initiates molecular processes that allow our immune system to generate antibodies against SARS-CoV-2. To establish lasting immunity to SARS-CoV-2, we suggest that AID could be the key to unlocking it.
Keywords: Perpetual immunity, Cytidine deaminase, SRS-CoV-2, New variants of Coronavirus

 Global reach, higher impact
Global reach, higher impact