3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2021; 18(15):3565-3573. doi:10.7150/ijms.63246 This issue Cite
Research Paper
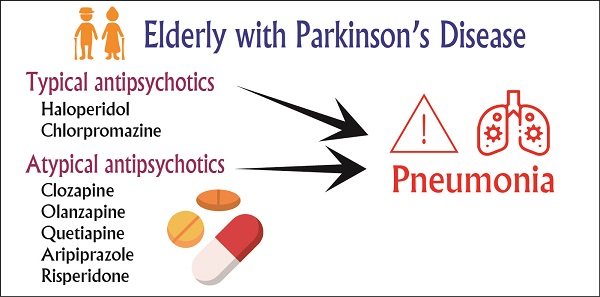
Risk of Pneumonia is associated with Antipsychotic Drug Use among older patients with Parkinson's Disease: A Case-control Study
1. Department of Health Services Administration, China Medical University, Taichung, Taiwan.
2. Department of Pharmacology, Chung Shan Medical University, Taichung, Taiwan.
3. Department of Pharmacy, Chung Shan Medical University Hospital, Taichung, Taiwan.
4. Department of Healthcare Administration, Asia University, Taichung, Taiwan.
5. Department of Long Term Care, National Quemoy University, Kinmen, Taiwan.
* These authors contributed equally to this work.
Abstract
Objective: To investigate the risk of pneumonia associated with the use of antipsychotic drugs in older-adult patients with Parkinson's disease (PD) in Taiwan.
Methods: This case-control study was based on data from the longitudinal health insurance database in Taiwan. We analyzed the data of 51,158 older patients with PD for the period between 2001 and 2016. To reduce the potential confounding caused by unbalanced covariates in nonexperimental settings, we used propensity score matching to include older patients without pneumonia to serve as the control group.
Results: Compared with patients who had never taken antipsychotics, current (adjusted odds ratios [aOR] =1.63, 95% confidence interval [CI] = 1.51-1.75), recent (aOR = 1.63, 95% CI = 1.52-1.74), and past (aOR = 1.89, 95% CI = 1.80-2.00) users of antipsychotics had a higher risk of incident pneumonia. Among typical and atypical antipsychotics, haloperidol and clozapine were associated with higher risks of incident pneumonia, respectively. By contrast, aripiprazole was not associated with a higher risk of pneumonia.
Conclusion: Older patients with PD receiving typical antipsychotics or atypical antipsychotics had a higher risk of pneumonia. Among these antipsychotics, clozapine had the highest risk of pneumonia. Clinicians should pay attention to the risk of pneumonia in older patients with PD who receive typical antipsychotics and atypical antipsychotics.
Keywords: pneumonia, antipsychotics, Parkinson's disease, pharmacoepidemiology

 Global reach, higher impact
Global reach, higher impact