3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2021; 18(11):2381-2388. doi:10.7150/ijms.57489 This issue Cite
Research Paper
Effects of neuromuscular blocking agents on the clinical performance of i-gel® and surgical condition in elderly patients undergoing hand surgery: a prospective randomized controlled trial
Department of Anaesthesiology and Pain medicine, Konyang University Hospital, Myunggok Medical Research Center, Konyang University College of Medicine, Daejeon, Korea.
Received 2020-12-23; Accepted 2021-4-2; Published 2021-4-16
Abstract
Background: The effects of neuromuscular blocking agents on the clinical performance of supraglottic airway devices and surgical condition in elderly patients undergoing hand surgery have not been established. We evaluated the effects of rocuronium on the clinical performance of an i-gel® supraglottic device and surgical condition in elderly patients undergoing orthopedic hand surgery.
Methods: Patients aged 65-85 years were randomized to receive either rocuronium (rocuronium group) or saline (control group). We compared the rates of successful insertion of the i-gel on the first attempt as a primary outcome and also assessed the adequacy of i-gel maintenance during controlled ventilation, anesthetic requirement, surgical condition, and recovery time.
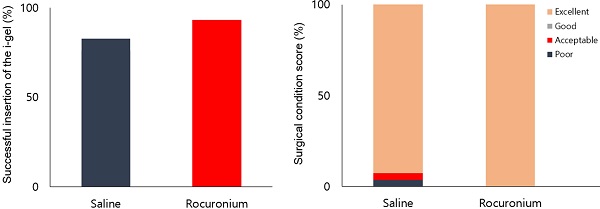
Results: The rates of successful insertion of the i-gel on a first attempt were 93.1% in the rocuronium group versus 82.1% in the control group (P = 0.423). Peak inspiratory pressure (PIP) was lower in the rocuronium group than in the control group (15.2 vs. 17.9 cmH2O, respectively, P = 0.028). Spontaneous breathing was less common in the rocuronium group (24.1% vs. 57.1%, respectively, P = 0.011). The requirement of additional fentanyl to suppress spontaneous breathing or patient movement was less in the rocuronium group than in the control group (24.1% vs. 50.0%, respectively, P = 0.043). Surgical condition did not differ between the two groups. Recovery time was shorter in the rocuronium group than in the control group (8.4 vs. 9.9 min, respectively, P = 0.030).
Conclusions: Rocuronium did not enhance the success rate of inserting the i-gel® or the surgical condition in elderly patients. However, using rocuronium reduced PIP, the frequency of spontaneous breathing, the requirement for additional fentanyl and patients' recovery time.
Keywords: neuromuscular blocking agents, surgery, aged, rocuronium
Introduction
Neuromuscular blocking agents (NMBAs), drugs that interrupt neuromuscular transmission at neuromuscular junctions via an acetylcholine receptor blockade, are used to paralyze skeletal muscles [1]. The use of NMBAs during general anesthesia has the advantages of facilitating endotracheal intubation during induction of anesthesia, providing sufficient surgical muscle relaxation, assisting with controlled ventilation, and reducing the anesthetic requirement during surgery [2,3]. However, NMBAs are the most common cause of perioperative anaphylaxis [4], and their use is a risk factor for accidental intraoperative awareness [5]. Furthermore, using intraoperative NMBAs may result in postoperative residual neuromuscular block, which can increase postoperative pulmonary complications [6]. Although there have been conflicting results regarding the association between age and postoperative residual neuromuscular block [7-9], some studies have found that the incidence of postoperative residual neuromuscular block increases with age [8,9], occurring more frequently in older adults than in younger patients [6].
Advances in supraglottic airway devices (SADs) have reduced the need for NMBAs during general anesthesia as an alternative to conventional airway management using an endotracheal tube [2]. However, the need for NMBAs when inserting and maintaining SADs is controversial, and studies have reported varying results depending on the proficiency of the person who inserted the SAD, the type of surgery, the kind of SAD, and the characteristics of the patient, such as obesity and age [10-13]. Therefore, to avoid adverse events related to the use of NMBAs, their use in patients undergoing surgery under general anesthesia using SADs should be individualized and confined to surgeries where it is mandatory [11,14].
The pharmacokinetics and pharmacodynamics of NMBAs may change in the elderly due to age-related changes in physiology [3]. In addition, the clinical efficacy of SADs is not the same as that in younger patients due to structural changes in the pharyngeal airway with age [15]. Nevertheless, few studies have determined the effects of NMBAs on the clinical performance of SADs in elderly patients [16]. Moreover, it is unclear whether not using an NMBA affects the surgical condition of elderly patients undergoing hand surgery with SADs [10,17]. Therefore, we designed this study to evaluate the effects of an NMBA (rocuronium) on the clinical performance of the i-gel® supraglottic device (i-gel) and surgical condition in elderly patients undergoing orthopedic hand surgery.
Methods
This prospective, randomized, controlled study was approved by the Konyang University Hospital Institutional Review Board (KYUH 2018-01-001-001) and was registered at the Korea Clinical Research Information Service (https://cris.nih.go.kr/, permit number: KCT 0003616). Written informed consent was obtained from the patients and/or from a legal representative. This study adhered to Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Patients aged 65-85 years old of American Society of Anesthesiologist Physical Status classification I-III and undergoing elective orthopedic hand surgery with an expected surgical duration < 2 h were included in the study. The exclusion criteria were morbid obesity (body mass index > 35 kg/m2), pharyngeal pathology, gastroesophageal reflux disease, a recent history of upper respiratory infection, loose teeth, psychiatric disease, or cognitive disorder.
Patients were randomly allocated to the rocuronium group or the control group in a 1:1 ratio using online randomization software (Researcher Randomizer; www.randomizer.org). Immediately before anesthesia was induced, a trained researcher who prepared the study drugs (rocuronium or normal saline) opened an opaque envelope containing the group allocations. The trained researcher was not involved in collecting the study data or inpatient care. Intra- and postoperative anesthetic management, assessments of outcome variables, and surgery in this study were conducted by two anesthesiologists and one surgeon, who were blinded to the patient allocation.
All patients fasted for at least 8 hours and entered the operating room without premedication. Before preparation for routine monitoring, each patient's dental status and modified Mallampati classification (class 1 = soft palate, fauces, uvula, and pillars visible; 2 = soft palate, fauces, uvula visible; 3 = soft palate, base of uvula visible; 4 = none of the soft palate visible) [18] were assessed by the anesthesiologist. Thereafter, pulse oximetry, electrocardiography, noninvasive blood pressure, and bispectral index (BIS) monitoring were applied. Patients were preoxygenated with 100% O2 at 8 L/min fresh gas flow for at least 3 min. Anesthesia was induced with 1 mg/kg lidocaine, 1-2 mg/kg propofol, and 1 μg/kg fentanyl. After confirming loss of consciousness and loss of the eyelid reflex, facemask ventilation was initiated with 3%-5% sevoflurane. The rocuronium group received 0.6 mg/kg intravenous rocuronium, while the control group received the same volume of normal saline. To ensure sufficient neuromuscular blockade in the rocuronium group [19] and adequate depth of anesthesia in the control group, there was a pause of at least 2 min after injecting the rocuronium or normal saline. The i-gel (Intersurgical Ltd., Wokingham, Berkshire, UK) was inserted if the BIS was < 60 in either group. The i-gel was inserted in both groups by the same anesthesiologist, who had clinical experience of more than 200 insertions of the i-gel.
The size of the i-gel was chosen based on the patient's body weight according to the manufacturer's instructions [20]. The posterior and lateral sides of the device were lubricated with water-soluble gel before the first insertion attempt. The primary outcome of this study was the rate of successful insertion of the i-gel on the first attempt. The i-gel was considered successfully inserted when normal square-wave capnography traces appeared, there was no audible leakage from the mouth of the patient at a peak inspiratory pressure (PIP) ≤ 20 cmH2O, and bilateral chest wall movements were observed [21]. Up to three insertion attempts were allowed, and each trial allowed manipulations for proper placement of the i-gel, such as neck extension or flexion, adjustment of the inserted depth by pushing or pulling on the device, and jaw thrust. If the third insertion attempt was unsuccessful, it was recorded as a failed i-gel insertion. In the case of a failure, endotracheal intubation was performed and the case was excluded from further evaluation. The ease of insertion was evaluated using a visual analog scale (VAS, 0 = extremely easy, 100 = extremely difficult) by the anesthesiologist who attempted the insertion [13]. Insertion time, which was defined as the time from picking up the device to successful insertion, was measured by the other anesthesiologist.
After successful insertion of the device, volume-controlled mechanical ventilation was started at a tidal volume of 7 mL/kg and a respiratory rate of 12 breaths/min. Then, the respiratory rate was adjusted to maintain end-tidal CO2 at 35-40 mmHg. The position of the i-gel was assessed using fiberoptic bronchoscopy and graded with the Brimacombe score (grade 1 = vocal cords not visible; 2 = vocal cords and anterior epiglottis visible; 3 = vocal cords and posterior epiglottis visible; 4 = only vocal cords visible) [22]. Oropharyngeal leak pressure (OLP) and gastric insufflation were evaluated after grading the fiberoptic view. OLP was measured by detecting an audible leak over the patient's mouth upon closing the expiratory valve of the anesthesia breathing system to 40 cmH2O at a fixed fresh gas flow of 3 L/min [21]. The presence of a sound in the epigastrium via stethoscope was considered gastric insufflation when the OLP was measured [21].
Anesthesia was maintained during surgery with 1%-3% sevoflurane in 50% nitrous oxide. The concentration of end-tidal sevoflurane was adjusted to maintain a BIS of 40-60, and the minimum end-tidal sevoflurane concentration to maintain the BIS < 60 was recorded. PIP was measured in the absence of spontaneous breathing or patient movement, and the highest PIP during surgery was recorded. Intraoperative spontaneous breathing and patient movement were recorded, and both were treated with an increase in sevoflurane concentration and/or a bolus injection of additional fentanyl (0.5-1 μg/kg) at the discretion of the anesthesiologist. Nevertheless, additional rocuronium (5-10 mg) was administered if these problems were not resolved or the surgeon required additional neuromuscular block.
After completing the surgery, surgical condition scores using a four-point scale (1 = poor, surgery cannot proceed because of muscle contractions or gross patient movement; 2 = acceptable, muscle contractions causing some interference in the surgical procedure; 3 = good, only a few muscle contractions that do not affect the surgical procedure; and 4 = excellent, no muscle contractions.) [10] were assessed by a single (board-certified) surgeon who performed the surgery. Sevoflurane and nitrous oxide were stopped and manual ventilation with 100% O2 at 6 L/min fresh gas was commenced. To reverse the neuromuscular blockade, the rocuronium group received 40 μg/kg neostigmine and 10 μg/kg glycopyrrolate, while the control group received the same volume of saline. The i-gel was removed after confirming that the patient obeyed verbal commands (e.g., “open your eyes”), spontaneously respired (respiratory rate 10-20 breaths/min), and the BIS was ≥80. The time from turning off the sevoflurane to removing the i-gel was defined as recovery time and was recorded. During emergence and removal of the i-gel, any adverse events, such as desaturation (peripheral oxygen saturation < 95%), coughing, bronchospasm, tongue/lip/teeth injury, or a blood-tinged tip of the i-gel were recorded. Postoperative pain and sore throat were evaluated in the post-anesthetic care unit (PACU) using a numerical rating scale (NRS) score (0 = no pain/sore throat, 10 = worst pain/sore throat imaginable). If the patient asked for an analgesic due to pain or the anesthesiologist judged that analgesic administration was necessary based on the NRS score, 0.5-1 μg/kg fentanyl was administered. If the patient complained of nausea or vomiting, 10 mg metoclopramide was given.
Statistical analyses
In previous studies of adult patients, the differences in the rate of successful insertion of the i-gel and LMA-ProSeal® on the first attempt between control and rocuronium groups were reported as 37% and 25%, respectively [12,13]. In addition, the rate of successful insertion of i-gel on the first attempt with rocuronium was reported as 94.7% in elderly patients [21]. Based on these previous reports [12,13,21], to detect a 30% difference in this rate between control and rocuronium groups with a power of 0.8 and a two-sided α-value of 0.05, 27 patients were required per group. Considering a dropout rate of 5%, 29 patients per group were recruited.
The statistical analyses were performed using PASW Statistics version 18 (IBM SPSS Inc., Chicago, IL, USA). After assessing the data distribution using the Kolmogorov-Smirnov test, continuous variables were analyzed using the Student's t-test or the Mann-Whitney U-test and are presented as mean ± standard deviation or median (interquartile range) values. Categorical variables were analyzed using the χ2 test, χ2 test for trends (linear-by-linear association), or Fisher's exact test, where appropriate, and are presented as a number or percentage (%). A two-sided P < 0.05 was considered significant.
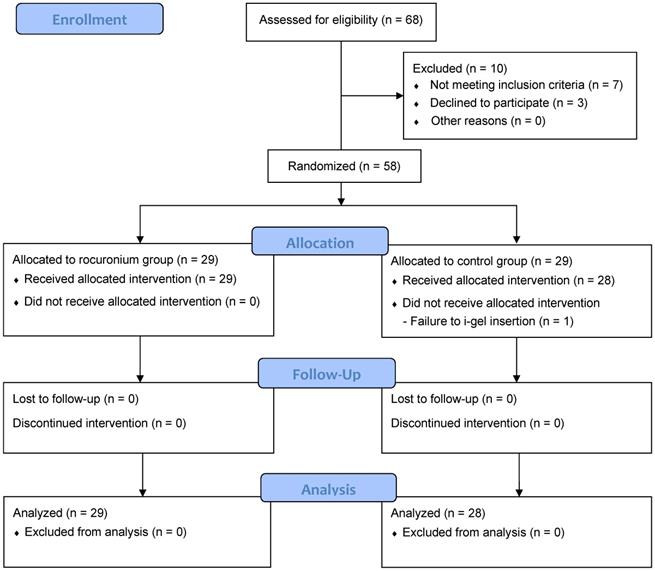
Flow diagram of patient enrollment.
Results
A total of 68 patients were assessed for eligibility, and 10 were excluded; thus, 58 were randomly allocated either to the rocuronium group or the control group. Thereafter, there was one insertion failure in the control group. Consequently, outcome variables measured during maintenance of anesthesia and recovery were analyzed in the remaining 29 patients in the rocuronium group and 28 patients in the control group (Fig. 1).
The patient characteristics of the two groups were similar (Table 1).
The outcome variables related to inserting the i-gel are presented in Table 2. Although the rates of successful insertion on the first attempt showed a mean difference of 10.3%, the difference was not significant (93.1% in the rocuronium group vs. 82.8% in the control group, 95% confidence interval [CI]: 7.5% to 28.3%, P = 0.423). The numbers of attempts to achieve successful insertion, insertion times, and ease of insertion were also not significantly different between the groups.
Patient characteristics
| Rocuronium (n = 29) | Control (n = 29) | P | |
|---|---|---|---|
| Age, year | 71.6 ± 5.1 | 70.5 ± 4.2 | 0.299 |
| Sex, male/female | 6/23 | 8/21 | 0.698 |
| Body mass index, kg/m2 | 24.5 ± 3.3 | 23.5 ± 5.3 | 0.334 |
| ASA classification, I/II/III | 1/23/3 | 3/22/4 | 0.775 |
| Modified Mallampati classification, 1/2/3/4 | 1/10/17/1 | 3/13/13/0 | 0.086 |
| Dental status, total/partial/edentulous | 21/6/2 | 19/8/2 | 0.769 |
| Duration of surgery, min | 51.1 ± 23.1 | 44.5 ± 18.7 | 0.235 |
| Duration of anesthesia, min | 69.1 ± 24.5 | 62.1 ± 19.1 | 0.230 |
| i-gel size, 3/4 | 22/7 | 20/9 | 0.704 |
Values are mean ± standard deviation or numbers;
ASA: American Society of Anesthesiologists.
The outcome variables measured during maintenance of anesthesia are shown in Table 3. PIP was significantly lower in the rocuronium group than in the control group (15.2 vs. 17.9 cmH2O, respectively; mean difference -2.65; 95% CI: 5.0-0.3; effect size 0.604; P = 0.028). The frequency of spontaneous breathing was significantly lower in the rocuronium group than in the control group (24.1% [7/29] vs. 57.1% [16/28], respectively; mean difference -33.0%; 95% CI: 53.2-7.5%, P = 0.011), but intraoperative patient movement did not differ between the two groups. Fewer patients in the rocuronium group required additional fentanyl during the surgery than in the control group (24.1% [7/29] vs. 50.0% [14/28], respectively; mean difference -25.9%; 95% CI: 46.9-0.9%; P = 0.043). OLP, gastric insufflation, fiberoptic view, patients requiring additional rocuronium, and the minimum end-tidal sevoflurane concentrations to keep the BIS < 60 were not significantly different between the two groups.
Comparison of outcome variables related to inserting the i-gel
| Rocuronium (n = 29) | Control (n = 29) | P | |
|---|---|---|---|
| Successful insertion at first attempt | 27 (93.1%) | 24 (82.8%) | 0.423† |
| Number of attempts for successful insertion (1/2/3/fail) | 27/1/1/0 | 24/3/1/1 | 0.254‡ |
| Insertion time, s | 17.0 (14.0-20.5) | 20.0 (16.3-24.8)* | 0.069§ |
| Ease of insertion, VAS | 20.0 (10.0-30.0) | 25.0 (15.0-33.8) | 0.148‡ |
Values are numbers (%), numbers, or the median (interquartile range);
VAS: visual analog scale (0 = extremely easy, 100 = extremely difficult).
*n = 28. †Fisher's exact test, ‡χ2 test for trends (linear-by-linear association), §Mann-Whitney U-test.
Comparison of outcome variables measured during maintenance of anesthesia
| Rocuronium (n = 29) | Control (n = 28) | P | |
|---|---|---|---|
| Fiberoptic view, 1/2/3/4 | 1/17/11/0 | 1/18/7/2 | 0.939* |
| Oropharyngeal leak pressure, cmH2O | 22.2 ± 4.4 | 22.6 ± 2.6 | 0.677† |
| Gastric insufflation | 3 (10.3%) | 9 (32.1%) | 0.056‡ |
| Peak inspiratory pressure, cmH2O | 15.2 ± 4.0 | 17.9 ± 4.9 | 0.028† |
| Spontaneous breathing | 7 (24.1%) | 16 (57.1%) | 0.011§ |
| Patient movement | 0 (0%) | 3 (10.7%) | 0.112‡ |
| Sevoflurane, vol% | 2 (1.8-2.2) | 2 (2-2.3) | 0.427 ΙΙ |
| Additional fentanyl | 7 (24.1%) | 14 (50.0%) | 0.043§ |
| Additional rocuronium | 0 (0%) | 0 (0%) | NA |
Values are mean ± standard deviation, numbers (%), number, or median (interquartile range).
Fiberoptic view: 1 = vocal cords not visible; 2 = vocal cords and anterior epiglottis visible; 3 = vocal cords and posterior epiglottis visible; 4 = only vocal cords visible, Sevoflurane: minimum end-tidal sevoflurane concentrations to keep BIS < 60, NA: not applicable. *χ2 test for trends (linear-by-linear association), †Student's t-test, ‡Fisher's exact test, §χ2 test, ΙΙMann-Whitney U-test.
The surgical condition scores and recovery data are shown in Table 4. The surgical condition scores were rated as excellent in all patients in the rocuronium group, while 92.9% (26/28) of patients were excellent, one was good, and the other was poor in the control group (P = 0.196). Recovery time was significantly shorter in the rocuronium group than in the control group (8.4 vs. 9.9 min, respectively; mean difference -1.41; 95% CI for the difference -2.68 to -0.14; effect size 0.627; P = 0.030). Adverse events during emergence, NRS for pain/sore throat, and the number of patients requiring a postoperative analgesic or antiemetic in the PACU did not differ between the groups.
Surgical condition scores and recovery data
| Rocuronium (n = 29) | Control (n = 28) | P | |
|---|---|---|---|
| In operating room | |||
| Surgical condition score | 0.196* | ||
| 1. Poor | 0 (0%) | 1 (3.6%) | |
| 2. Acceptable | 0 (0%) | 0 (0%) | |
| 3. Good | 0 (0%) | 1 (3.6%) | |
| 4. Excellent | 29 (100%) | 26 (92.9%) | |
| Recovery time, min | 8.4 ± 1.9 | 9.9 ± 2.8 | 0.030† |
| Adverse events during emergence | |||
| Coughing | 1 (3.4%) | 1 (3.6%) | > 0.999‡ |
| In PACU | |||
| NRS for pain | 3 (1.3-6.0) | 3 (2.0-7.0) | 0.248§ |
| NRS for sore throat | 0 (0-0.5) | 0 (0-0) | 0.545§ |
| Analgesics (fentanyl) | 9 (31.0%) | 8 (28.6%) | 0.839 ΙΙ |
| Antiemetics (metoclopramide) | 1 (3.4%) | 0 (0%) | > 0.999‡ |
Values are mean ± standard deviation, numbers (%), or median (interquartile range).
Recovery time: Time from stopping sevoflurane administration to removal of the i-gel, PACU: post-anesthetic care unit, NRS: numerical rating scale (0 = no sense of pain/ sore throat, 10 = worst imaginable sense of pain/sore throat). *χ2 test for trends (linear-by-linear association), †Student's t-test, ‡Fisher's exact test, §Mann-Whitney U-test, ΙΙχ2 test.
Discussion
This study demonstrated that an NMBA had no significant effect on inserting the i-gel in elderly patients, as assessed by the rate of successful insertion on the first attempt, number of attempts for successful insertion, insertion time, and ease of insertion. In addition, although an NMBA was not administered, 96.4% (27/28) of the elderly patients who underwent orthopedic hand surgery showed good or excellent surgical condition in the control group. However, patients who did not receive the NMBA had a higher PIP, more frequent spontaneous breathing during mechanical ventilation, and an increased requirement for additional fentanyl to suppress spontaneous breathing or movement. Recovery time was delayed in patients who did not receive the NMBA.
Augmented fitting of a SAD in the oral cavity by sufficient relaxation of the pharyngeal muscles and increased upper airway collapsibility has been suggested as an explanation for the increased efficacy of SADs when NMBAs were administered compared to when NMBAs were not used in adult patients [12,13]. However, as age increases, the sensitivity of upper-airway reflexes to stimuli and genioglossus negative pressure reflex, the main mechanism for maintaining pharyngeal patency, decreases, thus upper-airway collapsibility increases in the elderly [23,24]. For these reasons, the facilitating effects of NMBAs on the insertion of SADs may be attenuated in elderly patients. This assumption is supported by the results of this study, indicating that rocuronium did not significantly improve any of the outcome variables associated with inserting the i-gel.
The rates of successful insertion of the i-gel on the first attempt were 94.7% and 94.3% in previous studies performed in paralyzed elderly patients [20,21], which are comparable to the 93.1% in the rocuronium group of this study. In contrast, these rates were 86% and 93.3% in non-paralyzed adult patients [25,26], a slightly higher trend than the 82.8% of the control group in our study. However, considering that a longer insertion time and a lower success rate are achieved in elderly patients than younger adult patients due to structural changes in the pharyngeal airway that occur with aging [15], the results of our study are understandable.
Only a few studies have compared the effects of an NMBA on SAD sealing pressure [11-13], but the results have been inconsistent; administration of an NMBA increased the sealing pressure of the i-gel [12] and the LMA-ProSeal® [13] in adult patients, while another study found that an NMBA did not change the airway sealing pressure of the LMA-ProSeal® in adult female patients [11]. Nevertheless, none of these studies evaluated the grade of fiberoptic view. In contrast, the grade of fiberoptic view was evaluated in the present study and did not show a group difference. This means that the anatomical position in which the tip of the i-gel was placed was similar in the two groups. Thus, OLP was comparable between the two groups in our study.
During mechanical ventilation, advantages of NMBAs include increased chest-wall compliance, suppressed respiratory movements, prevention of patient-ventilator dyssynchrony, and reduced peak inspiratory and plateau pressures [27]. Similarly, PIP and the number of patients who exhibited spontaneous breathing were significantly lower in the rocuronium group than in the control group. In addition, intraoperative patient movement was not observed in any patient in the rocuronium group. As PIP increases, the risk for gastroesophageal insufflation also increases, which may increase the risk for pulmonary aspiration [28]. Although no significant difference was observed in our study, the rate of gastric insufflation was nearly three times less in the rocuronium group than in the control group (10.3% vs. 32.1%, respectively, P = 0.056). Therefore, an NMBA should be considered when PIP is expected to increase during mechanical ventilation via an i-gel, such as in cases of obesity, laparoscopic surgery, head-down position, or restrictive lung disease [29].
Although NMBAs are commonly used to improve the surgical condition [2,3], the effects of NMBAs on surgical condition are diverse, depending on the depth of the neuromuscular block (i.e., deep vs. moderate), type of surgery (e.g., laparoscopic vs. open surgery), age of the patient (e.g., children vs. adults), and airway management device (e.g., endotracheal tube vs. SAD) [10,11,30]. Therefore, it may be necessary to use NMBAs prudently depending on the characteristics of the surgery and of the patient when SADs are applied for airway management. In this study, patients' surgical condition was comparable regardless of rocuronium administration. However, this result should be interpreted cautiously. This may not mean that NMBAs are unnecessary to improve surgical condition, because all patients in the rocuronium group were rated excellent for surgical condition.
Another remarkable result is that recovery times were shorter in patients who received rocuronium. This is inconsistent with previous findings, as not using an NMBA shortened recovery in children undergoing inguinal herniorrhaphy [10] and in adult women undergoing laparoscopic gynecological surgery [11]. The main reason for this discrepancy appears to be because additional intraoperative fentanyl administration was more frequent in patients who did not receive rocuronium in our study than in a previous study [10]. Fentanyl enhances the sedative effects of inhalation anesthetics, such as sevoflurane [31]. Furthermore, the duration of action of fentanyl is prolonged in the elderly, and fentanyl itself is a cause of delayed recovery [32].
This study had several limitations. First, because the sample size calculation was performed only for the rate of successful insertion on the first attempt, which was the primary outcome, this study may have been underpowered to assess the remaining outcome variables. Second, as all i-gels were inserted by a single experienced anesthesiologist, the findings of this study, particularly the outcome variables related to inserting the i-gel, may not extend to inexperienced users. The rate of successful insertion of an i-gel on the first attempt is only 11.4% without rocuronium and 48.6% with rocuronium when novice personnel insert the i-gel in adult patients [12], which is considerably lower than the rate in this study. Third, in this study, the surgical condition was not measured using an objective evaluation tool [33], but was evaluated subjectively based on the opinion of a single board-certified surgeon. Therefore, depending on the evaluator, the results for the surgical condition may not be consistent. Finally, although sevoflurane was adjusted by the same target BIS value (40-60) in both groups and minimum end-tidal sevoflurane concentrations were adjusted to keep the BIS < 60, which was comparable in the two groups, it was difficult to determine the exact dose of sevoflurane administered during anesthesia. Sevoflurane is associated with dose-dependent suppression of minute ventilation and neuromuscular function [34], which may have affected the results of this study, such as spontaneous breathing, surgical condition, and recovery time. Therefore, future studies require the application of total intravenous anesthesia to rule out the effects of inhalational anesthetics on neuromuscular blockade and to facilitate a comparison of the anesthetic dose administered.
In conclusion, rocuronium did not improve the i-gel insertion success rate or the surgical condition in elderly patients undergoing orthopedic hand surgery. However, anesthesia using the i-gel without rocuronium led to increased PIP and frequency of spontaneous breathing during controlled mechanical ventilation, which may require anesthesiologists to manage the ventilator more carefully intraoperatively. In addition, increases in intraoperative requirements of anesthetics such as fentanyl may lead to delayed recovery. Our findings imply that rocuronium should be administered discreetly to elderly patients undergoing orthopedic hand surgery under general anesthesia using an i-gel to reduce ventilator problems or anesthetics requirements, rather than be routinely administered.
Acknowledgements
Roles of Authors
All of the listed authors were involved in the drafting of the work, approved the final manuscript, and agreed to be accountable for all aspects of this work.
- Choon-Kyu Cho helped writing the manuscript, analyzing and interpretation of data;
- Choon-Kyu Cho, Minhye Change & Seok-Jin Lee helped the acquisition, analysis, and interpretation of data;
- Tae-Yun Sung helped the conception and design of the study, statistical analysis and writing of the manuscript.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Larijani GE, Gratz I, Silverberg M, Jacobi AG. Clinical pharmacology of the neuromuscular blocking agents. DICP. 1991;25(1):54-64 doi: 10.1177/106002809102500111
2. Meakin GH. Role of muscle relaxants in pediatric anesthesia. Curr Opin Anaesthesiol. 2007;20:227-31 doi: 10.1097/ACO.0b013e328108f430
3. Lee LA, Athanassoglou V, Pandit JJ. Neuromuscular blockade in the elderly patient. J Pain Res. 2016;9:437-44 doi: 10.2147/JPR.S85183
4. Galvao VR1, Giavina-Bianchi P, Castells M. Perioperative anaphylaxis. Curr Allergy Asthma Rep. 2014;14(8):452. doi: 10.1007/s11882-014-0452-6
5. Pandit JJ, Andrade J, Bogod DG, Hitchman JM, Jonker WR, Lucas N. et al. 5th National Audit Project (NAP5) on accidental awareness during general anaesthesia: summary of main findings and risk factors. Br J Anaesth. 2014;113(4):549-59 doi: 10.1093/bja/aeu313
6. Murphy GS, Szokol JW, Avram MJ, Greenberg SB, Shear TD, Vender JS. et al. Residual neuromuscular block in the elderly: Incidence and clinical implications. Anesthesiology. 2015;123:1322-36 doi: 10.1097/ALN.0000000000000865
7. Kaan N, Kocaturk O, Kurt I, Cicek H. The incidence of residual neuromuscular blockade associated with single dose of intermediate-acting neuromuscular blocking drugs. Middle East J Anaesthesiol. 2012;21(4):535-41
8. Yamamoto H, Uchida T, Yamamoto Y, Ito Y, Makita K. Retrospective analysis of spontaneous recovery from neuromuscular blockade produced by empirical use of rocuronium. J Anesth. 2011;25:845-9 doi: 10.1007/s00540-011-1229-x
9. Yazar E, Yılmaz C, Bilgin H, Karasu D, Bayraktar S, Apaydın Y. et al. A comparison of the effect of sugammadex on the recovery period and postoperative residual block in young elderly and middle-aged elderly patients. Balkan Med J. 2016;33(2):181-7
10. Koo BW, Jung KW, Oh AY, Kim EY, Na HS, Choi ES. et al. Is neuromuscular blocker needed in children undergoing inguinal herniorrhaphy? A prospective, randomized, and controlled trial. Medicine (Baltimore). 2017;96(26):e7259. doi: 10.1097/MD.0000000000007259
11. Chen BZ, Tan L, Zhang L, Shang YC. Is muscle relaxant necessary in patients undergoing laparoscopic gynecological surgery with a ProSeal LMA? J Clin Anesth. 2013;25:32-5 doi: 10.1016/j.jclinane.2012.06.004
12. Hattori K, Komasawa N, Miyazaki Y, Kido H, Deguchi S, Minami T. Muscle relaxant facilitates i-gel insertion by novice doctors: A prospective randomized controlled trial. J Clin Anesth. 2016;33:218-22 doi: 10.1016/j.jclinane.2016.03.058
13. Fujiwara A, Komasawa N, Nishihara I, Miyazaki S, Tatsumi S, Nishimura W. et al. Muscle relaxant effects on insertion efficacy of the laryngeal mask ProSeal® in anesthetized patients: A prospective randomized controlled trial. J Anesth. 2015;29:580-4 doi: 10.1007/s00540-015-1982-3
14. Ghoneim MM. Awareness during anesthesia. Anesthesiology. 2000;92(2):597-602 doi: 10.1097/00000542-200002000-00043
15. Kim EM, Kim MS, Koo BN, Lee JR, Lee YS, Lee JH. Clinical efficacy of the classic laryngeal mask airway in elderly patients: A comparison with young adult patients. Korean J Anesthesiol. 2015;68:568-74 doi: 10.4097/kjae.2015.68.6.568
16. Kong M, Li B, Tian Y. Laryngeal mask airway without muscle relaxant in femoral head replacement in elderly patients. Exp Ther Med. 2016;11:65-8 doi: 10.3892/etm.2015.2844
17. King M, Sujirattanawimol N, Danielson DR, Hall BA, Schroeder DR, Warner DO. Requirements for muscle relaxants during radical retropubic prostatectomy. Anesthesiology. 2000;93(6):1392-7 doi: 10.1097/00000542-200012000-00008
18. Tham EJ, Gildersleve CD, Sanders LD, Mapleson WW, Vaughan RS. Effects of posture, phonation and observer on Mallampati classification. Br J Anaesth. 1992;68(1):32-8 doi: 10.1093/bja/68.1.32
19. Naguib M. Neuromuscular effects of rocuronium bromide and mivacurium chloride administered alone and in combination. Anesthesiology. 1994;81(2):388-95 doi: 10.1097/00000542-199408000-00017
20. Kim MH, Lee JH, Choi YS, Park S, Shin S. Comparison of the laryngeal mask airway supreme and the i-gel in paralysed elderly patients: A randomised controlled trial. Eur J Anaesthesiol. 2018;35:598-604 doi: 10.1097/EJA.0000000000000700
21. In CB, Cho SA, Lee SJ, Sung TY, Cho CK. Comparison of the clinical performance of airway management with the i-gel® and laryngeal mask airway SupremeTM in geriatric patients: A prospective and randomized study. Korean J Anesthesiol. 2019;72(1):39-46 doi: 10.4097/kja.d.18.00121
22. Brimacombe J, Berry A. A proposed fiber-optic scoring system to standardize the assessment of laryngeal mask airway position. Anesth Analg. 1993;76:457
23. Erskine RJ, Murphy PJ, Langton JA, Smith G. Effect of age on the sensitivity of upper airway reflexes. Br J Anaesth. 1993;70(5):574-5 doi: 10.1093/bja/70.5.574
24. Eikermann M, Jordan AS, Chamberlin NL, Gautam S, Wellman A, Lo YL. et al. The influence of aging on pharyngeal collapsibility during sleep. Chest. 2007;131(6):1702-9 doi: 10.1378/chest.06-2653
25. Gatward JJ, Cook TM, Seller C, Handel J, Simpson T, Vanek V. et al. Evaluation of the size 4 i-gel airway in 100 non-paralysed patients. Anaesthesia. 2008;63:1124-30 doi: 10.1111/j.1365-2044.2008.05561
26. Chew EE, Hashim NH, Wang CY. Randomised comparison of the LMA Supreme with the I-Gel in spontaneously breathing anaesthetised adult patients. Anaesth Intensive Care. 2010;38(6):1018-22 doi: 10.1177/0310057X1003800609
27. Bennett S, Hurford WE. When should sedation or neuromuscular blockade be used during mechanical ventilation? Respir Care. 2011;56(2):168-76 doi: 10.4187/respcare.01095
28. Cajander P, Edmark L, Ahlstrand R, Magnuson A, de Leon A. Effect of positive end-expiratory pressure on gastric insufflation during induction of anaesthesia when using pressure-controlled ventilation via a face mask: A randomised controlled trial. Eur J Anaesthesiol. 2019;36(9):625-32 doi: 10.1097/EJA.0000000000001016
29. Lopez-Gil M, Brimacombe J. The ProSeal laryngeal mask airway in children. Paediatr Anaesth. 2005;15:229-34 doi: 10.1111/j.1460-9592.2005.01427.x
30. Kopman AF, Naguib M. Is deep neuromuscular block beneficial in laparoscopic surgery? No, probably not. Acta Anaesthesiol Scand. 2016;60(6):717-22 doi: 10.1111/aas.12699
31. Glass PSA, Gan TJ, Howell S, Ginsberg B. Drug interactions: Volatile anesthetics and opioids. J Clin Anesth. 1997;9(6):18S-22S doi: 10.1016/s0952-8180(97)00122-0
32. Sinclair R, Faleiro R. Delayed recovery of consciousness after anaesthesia. Continuing Educ Anaesth Crit Care Pain. 2006;6:114-8
33. Koo BW, Oh AY, Na HS, Lee HJ, Kang SB, Kim DW. et al. Effects of depth of neuromuscular block on surgical conditions during laparoscopic colorectal surgery: a randomised controlled trial. Anaesthesia. 2018;73(9):1090-6 doi: 10.1111/anae.14304
34. Nitahara K, Sugi Y, Higa K, Shono S, Hamada T. Neuromuscular effects of sevoflurane in myasthenia gravis patients. Br J Anaesth. 2007;98(3):337-41 doi: 10.1093/bja/ael368
Author contact
![]() Corresponding author: Tae-Yun Sung, 158 Gwangeodong-ro, Seo-gu, Department of Anesthesiology and Pain Medicine, Konyang University Hospital, Konyang University College of Medicine, Daejeon, 35365, Korea. Tel.: +82-42-600-9316; Fax: +82-42-545-2132; E-mail: unt1231com.
Corresponding author: Tae-Yun Sung, 158 Gwangeodong-ro, Seo-gu, Department of Anesthesiology and Pain Medicine, Konyang University Hospital, Konyang University College of Medicine, Daejeon, 35365, Korea. Tel.: +82-42-600-9316; Fax: +82-42-545-2132; E-mail: unt1231com.

 Global reach, higher impact
Global reach, higher impact