3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2019; 16(2):247-252. doi:10.7150/ijms.28730 This issue Cite
Research Paper
Reliability of Preoperative Inguinal Sonography for Evaluating Patency of Processus Vaginalis in Pediatric Inguinal Hernia Patients
1. Department of Surgery, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Republic of Korea
2. Department of Surgery, Konkuk University Chungju Hospital, Chungju, Republic of Korea
Received 2018-7-24; Accepted 2018-12-4; Published 2019-1-1
Abstract
Background: Among childhood illnesses requiring surgery, inguinal hernia is the most common entity. Pediatric inguinal hernia has been traditionally operated through a small incision in the inguinal region. Contralateral metachronous inguinal hernia has been the topic of discussion in pediatric surgeon's domain for a long time. Many studies have been conducted to prevent it from occurring. Although patency of processus vaginalis is known to be the cause of metachronous inguinal hernia, it is difficult to know the status of contralateral processus vaginalis preoperatively when the patient is non-symptomatic. Recently, the introduction of laparoscopic surgery has facilitated the observation and surgery of contralateral inguinal hernia during scheduled surgery of unilateral hernia repair while the processus vaginalis is intact. The standard treatment for inguinal hernia is herniotomy. Laparoscopic inguinal hernia repair has not been widely applied in Korea. The objective of this study was to analyze the accuracy of preoperative sonography results of inguinal lesion on the contralateral side in patients that needed laparoscopic operation of inguinal hernia.
Methods: Data of 107 patients who received laparoscopic inguinal hernia repair and evaluation by preoperative ultrasonography at Dongguk University Ilsan Hospital from 2011 to 2015 were analyzed.
Results: Preoperative sonography for inguinal lesion had a sensitivity of 20.5%, a specificity of 95.2%, a positive predictive value of 75%, and a negative predictive value of 63.2%. Its accuracy was 64.5%. A total of 107 patients had no inguinal hernia recurrence or metachronous contralateral inguinal hernia.
Conclusion: Ultrasonography performed prior to traditional pediatric herniotomy is not enough for accurate diagnosis of patency of processus vaginalis in our retrospective study. Multicenter prospective study is needed to estimate accuracy of sonographic diagnosis for patency of processus vaginalis.
Keywords: processus vaginalis, pediatric inguinal hernia, contralateral metachronous hernia, sonography
Introduction
Inguinal hernia is one of the most common diseases that require surgery in children. Pediatric inguinal hernia surgery has been traditionally treated with herniotomy and high ligation of the hernia sac. Development of metachronous hernia after inguinal hernia surgery has been discussed in the field of pediatric surgery. Reported incidence of contralateral side metachronous inguinal hernia ranged from 3.0% to 14.7% [1, 2]. The incidence of contralateral side metachronous inguinal hernia is higher in children than that in adults. Patency of processus vaginalis (PPV) is known to be the cause of pediatric inguinal hernia. The causes of contralateral side metachronous inguinal hernia is also assumed to be PPV [1, 2]. However, it is difficult to evaluate processus vaginalis on the contralateral side when it is asymptomatic. To prevent metachronous inguinal hernia, contralateral inguinal herniotomy, pneumoperitoneal examination, herniography, and laparoscopic examination through hernia sac have been performed [3-7].
Some surgeons have performed bilateral herniotomy in patients with high risk of bilateral inguinal hernia. However, there might be complications such as testicular atrophy and infertility [8-11]. Prophylactic surgery of PPV is also controversial because the lesion is not a true hernia [12].
It is currently unclear whether PPV will develop to true hernia. It is difficult to determine the accuracy of sonography for diagnosing PPV using metachronous hernia recurrence. Recent advances in laparoscopic inguinal hernia surgery have led to a reduction in incidence of metachronous hernia by suturing contralateral PPV [13-15].
The purpose of this study was to compare results of preoperative ultrasonography and laparoscopic findings to evaluate the accuracy of preoperative ultrasonography for predicting inguinal hernia on the contralateral side in patients with unilateral inguinal hernia.
Patients and methods
From 2011 to 2015, 211 patients who underwent surgery for pediatric inguinal hernia at Dongguk University Ilsan Hospital were enrolled. Of these 211 patients, 96 who did not undergo ultrasonography, 4 who had been previously operated for contralateral hernia, and 4 who had bilateral inguinal hernia were excluded. Finally, data of 107 patients who underwent ultrasonography for the uninvolved site were retrospectively analyzed.
Method of ultrasonography
Ultrasonography was performed by one professor specialized in urogenital radiology using a 10 MHz detector. Negative ultrasonography finding was considered as normal inguinal finding. Positive finding was defined as abnormal shading. The size of the internal inguinal ring was not checked.
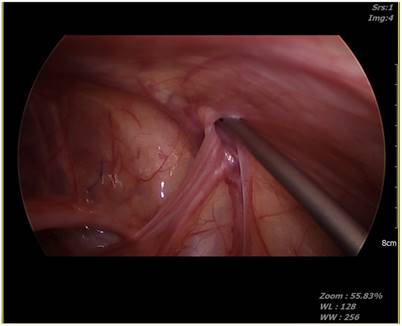
Inguinal hernia laparoscopic surgery method
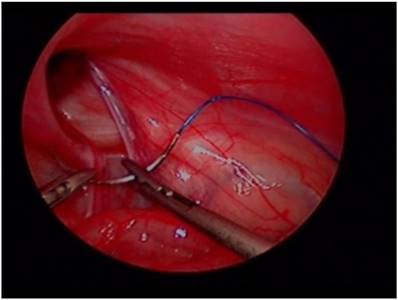
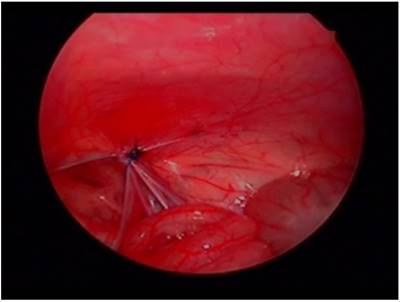
Patients underwent surgery with pelvis slightly elevated in supine position. A 5 mm, 30° angled laparoscope was inserted above or through the umbilicus. We maintained an 8mmHg pressure for pneumoperitoneum, confirmed unilateral hernia, and evaluated contralateral side processus vaginalis opening. Two 2.7 mm laparoscopic needle holders were inserted into both abdominal sides at the level of umbilicus. The internal opening of inguinal hernia was then ligated using a purse string suture method. In the case of the opposite-side PPV, it was sutured using the same method (Fig. 1, Fig. 2). Contralateral PPV repair indication was: depth of PPV > 1 cm, no relation with diameter of PPV or shape.
Laparoscopic view of hernia site.
Laparoscopic view of purse-string repair.
Statistics
All statistical analyses were performed using SPSS 15.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was defined at p < 0.05.
Results
A total of 107 patients were included in our study, including 75 males and 32 females (male to female ratio of 2.3:1). Their mean age was 4.1 years (range, 39 days to 15 years). All inguinal hernias were indirect hernias. Opened PPV was found in 44 (41.1%) unilateral inguinal hernia patients. The patients with opened PPV were younger about thirty months than the other group (p = 0.03). Rate of opened PPV in unilateral inguinal hernia patients was 38.5% in the left side vs. 44% in the right side (p =0.69), and 41.3% in males vs. 40.6% in females (p = 0.541) (Table 1).
Characteristics of patients (N = 107)
| Contralateral PPV* (-) | Contralateral PPV* (+) | Total cases | p-value | |
|---|---|---|---|---|
| Age (months) | 60.1 ± 47.0 | 31.0 ± 30.6 | 49.4 ± 43.6 | 0.03 |
| Gender (male: female) | 44:19 | 31:13 | 75:32 | 0.94 |
| Body weight (kg) | 19.2 ± 14.0 | 12.2 ± 8.4 | 16.3 ± 12.4 | 0.004 |
| Prematurity (<36weeks) | 8 | 9 | 17 | 0.29 |
| Hernia site (right: left) | 35:28 | 22:22 | 57:50 | 0.69 |
PPV*(-): no patent processus vaginalis; PPV*(+): patent processus vaginalis.
Preoperative sonographic examination confirmed opened PPV in 12 patients. In 44 patients who were confirmed during laparoscopic surgery, 9 out of 44 patients with opened PPV had sonographic results. Thus, the sensitivity of sonographic examination for detecting PPV was 20.5% (9/44). Of 63 patients with negative PPV findings during laparoscopic surgery, 60 were diagnosed as having negative PPV by sonography. Thus, the specificity of sonography was 95.2% (sensitivity: 20.5%; accuracy: 64.5%). Of the 12 patients diagnosed as having positive PPV by sonography, 9 patients had positive PPV in laparoscopy. The positive predictive value of sonography was 75.0% and the negative predictive value was 63.2% (Table 2). Laparoscopic findings and sonographic findings were identical in 69 patients. The accuracy of sonography was 64.5%.
Results of sonographic findings (N = 107)
| sonoǂ | opߙ | ||
|---|---|---|---|
| Contralateral PPV*(-) | Contralateral PPV*(+) | Total cases | |
| Contralateral PPV*(-) | 60(56.1%) | 35(32.7%) | 95(88.8%) |
| Contralateral PPV*(+) | 3(2.8%) | 9(9.4%) | 12(11.2%) |
| Total cases | 63(58.9%) | 44(41.1%) | 107 |
opߙ: operative finding; sonoǂ: sonography finding; Positive predictive value: 75.0%;
Negative predictive value: 63.2%.
Postoperative complications occurred in 3 patients. Two cases of hydrocele developed at 1 week postoperatively and resolved in 3 months. One wound infection occurred 1 week after surgery. It was improved after 1 week. The mean follow-up period was 57.6 months for 63 unilateral hernia repair patients and 56.0 months for 44 patients who underwent bilateral repair due to positive PPV. There was no recurrence or metachronous hernia of the inguinal hernia during the follow-up period in unilateral inguinal hernia patients (Table 3).
Results of postoperative follow-up (N = 107)
| Contralateral PPV*(-) N=63 | Contralateral PPV*(+) N=44 | |
|---|---|---|
| Follow-up(month) | 57.6±13.9 | 56.0±14.4 |
| Post-operative complications | 1(0.9%) | 2(1.9%) |
| Recurrence | 0 | 0 |
| Metachronous hernia | 0 | 0 |
Discussion
Inguinal hernia has a higher incidence of metachronous hernia in pediatric patients than that in adults. The incidence of contra-lateral inguinal hernia in children is reported to be 3.0~14.7% [1, 2]. There is no conclusion as to which PPV may develop to be clinical hernia. However, a PPV is accepted as a cause of metachronous hernia. Recently, laparoscopic surgery has been popularized in pediatric patients because it is easy to observe the contralateral internal ring during laparoscopy. It is particularly advantageous when simultaneous repair of the opened PPV is needed [14, 15]. Time for bilateral hernia surgery does not show much difference from time for unilateral surgery. Becmeur et al. [16] have reported that a surgeon who is familiar with laparoscopic surgery can overcome 20 scheduled road learning curve. Since 1955, Rothenberg et al. [3-7] have conducted various studies on the contralateral inguinal area with examination, herniography, and laparoscopic examination through hernia sac. Klin et al. [18] have reported that laparoscopic examination of the hernia sac is simple and accurate. It can reduce contralateral side negative herniotomy. Antonoff et al. [19] reported that the rate of laparoscopic examination of the hernia sac for pediatric surgeons was 2% in 1996, 24% in 2002, and 37% in 2005.
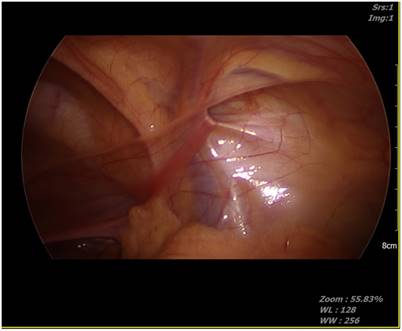
There are two methods to observe the contralateral side internal inguinal area: laparoscopic examination through the inguinal hernia sac and laparoscopic examination through the umbilicus. Laparoscopic examination through the hernia sac is more commonly applied after it was first reported by Lobe et al. [20]. Sozubir et al. [8] have performed laparoscopic inguinal internal ring examination through hernia sac in 497 patients and reported that the rate of opening is 19.4% with positive predictive value of 100%. However, 6 patients did not undergo laparoscopic examination due to anatomical problems [8]. Laparoscopic inguinal examination through hernia sac cannot be performed when the hernia sac is too weak. In some cases, the peritoneal veil can result in false negative finding (Fig. 3). The failure rate of laparoscopic inguinal examination through hernia sac due to peritoneal veil is 3-8% [21].
Peritoneal veil.

In 2001, after laparoscopic hernia repair was performed, laparoscopic findings of the PPV through the umbilicus were reported by Schier et al. [22]. In 2010, Niyogi et al. [23] reported that laparoscopic inguinal examination through the umbilicus was more accurate than laparoscopic inguinal examination through hernia sac because of the higher positive PPV rate of contralateral inguinal hernia and the lower incidence of metachronous inguinal hernia. In 2014, Zhong et al. [24] reported that the incidence of metachronous hernia was 0.85% in laparoscopic examination through the umbilicus and 1.78% in laparoscopic examination through the hernia sac.
The most popular method for preventing metachronous inguinal hernia is ultrasonography before herniotomy. Laparoscopic examination through the umbilicus is the most accurate method for observation of contralateral PPV. Thus, we sought to evaluate the accuracy of ultrasonography by comparing results between laparoscopic examination and sonographic finding. The low accuracy rate of sonography (64.5%) suggests that sonography has limited ability to reduce incidence of metachronous inguinal hernia.
In 1994, Lawrenz et al. performed preoperative sonography in 23 patients and bilateral herniotomy for all cases. Sonographic positive PPV was observed in 15 of 23 patients and bilateral herniotomy was confirmed in 18 of 23 patients. Four false positives and 4 false-negative were observed. They reported that sonography had a sensitivity of 78%, a specificity of 20%, and an accuracy of 65% [25]. In 2004, Hata et al. [26] performed sonography in 348 patients with unilateral inguinal hernia and bilateral herniotomy in sonographically positive PPV patients. In 78 patients, bilateral herniotomy was performed and results were compared with sonographic results. The patency was confirmed in 74 of 78 patients. The accuracy of sonography was 94.9% [26]. In 2011, Hasanuzzaman et al. [27] performed sonography for 30 cases of unilateral inguinal hernia to observe contralateral side PPV. They found 12 opened PPV and performed bilateral herniotomy. The accuracy of sonography was 91.7%.
In 2015, Kaneda et al. [28] evaluated 105 cases of unilateral inguinal hernia to determine the usefulness of sonography for PPV. The internal diameter of the PPV was observed by sonography before the herniotomy. It was observed for 36 months. Of 105 patients with unilateral inguinal hernia, 11 patients had metachronous hernia. Sonographic results showed that the incidence of metachronous hernia was higher when the size of the inner inguinal ring of PPV was 2 mm or more (p = 0.001). The incidence of metachronous hernia showed no correlation with gender (p = 0.350), age (p = 0.185), birth weight (p = 0.939), or site of inguinal hernia (p = 0.350) [28]. They suggested that sonography could reduce the incidence of metachronous hernia by preoperative check. However, in our study, sonography did not directly detect contralateral PPV in all patients.
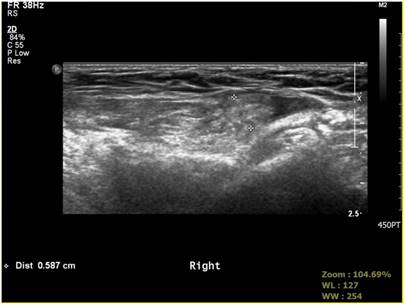
The accuracy of sonography from well-known studies was of a similar figure to the accuracy of 64.5% resulted in our study. The accuracy of sonography can be affected by ultrasound resolution, diagnostic criteria, and skillfulness of the operator. In our study, sonography was performed by one genitourinary radiologist. The measurement of the inner ring size was not performed on PPV. We set abnormal shading on sonography as a positive finding. By comparing sonography results with findings of laparoscopy, we were able to better understand the sonographic accuracy of contralateral PPV (Fig. 4, Fig. 5).
Positive sonographic finding of processus vaginalis.
Positive operative finding of processus vaginalis.
According to a recent meta-analysis by Dreuning et al. [29], preoperative sonography is useful because of its high sensitivity and specificity. However, the authors suggested the need to clarify diagnostic criteria of contralateral PPV and the need of follow-up observation for patients who were negative on sonography [29]. Sumida et al. [30] reported that sonographic examination accuracy for contralateral PPV showed a decrease with increasing age. However, laparoscopic findings suggested that the frequency of contralateral PPV increased with increasing age [30]. The authors also reported the difference between sonographic and operative findings [30]. We considered preoperative sonographic PPV prediction as sonographic accuracy by comparing preoperative sonographic finding to intraoperative laparoscopic finding.
The accuracy of sonography in our study was 64.5%. In our study, 35 out of 95 patients without abnormal findings in the preoperative sonography showed positive PPV. The preoperative sonography had higher false negative rate base on laparoscopic finding for sensitivity. The higher PPV rate in our study than previously reported PPV rate might be due to the sensitivity of laparoscopic examination. Broad multicenter study with more enrolled patients might lead to higher accuracy of preoperative sonography. Also, large scale studies with long-term follow-up are needed to determine the exact incidence of metachronous hernia in pediatric inguinal hernia patients. Expansion of laparoscopic surgery for pediatric inguinal hernia suggests that pediatric surgeons should do long-term follow-up of patients. We also need more studies on natural history of PPV because preoperative sonography alone is insufficient to confirm the status of PPV (Fig. 6, Fig. 7).
Negative sonographic finding of processus vaginalis.

Positive operative finding of processus vaginalis.
Conclusion
Ultrasonography performed prior to the surgery of a traditional pediatric herniotomy is is not enough for accurate diagnosis of patency of processus vaginalis in our retrospective study. Multicenter prospective study is warranted to have precise evaluation of sonographic accuracy for detecting patency of processus vaginalis.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Ron O, Eaton S, Pierro A. Systematic review of the risk of developing a metachronous contralateral inguinal hernia in children. Br J Surg. 2007;94:804-11
2. Yoon YH, Heo CY, Chun YS. Clinical study of inguinal hernia in pediatric patients. J Korean Assoc Pediatr Surg. 2009;15:44-51
3. Ducharme JC, Bertrand R, Chacar R. Is it possible to diagnose inguinal hernia by x-ray? A preliminary report on herniography. J Can Assoc Radiol. 1967;18:448-51
4. Leape LL. Herniograms-a commentary. Surgery. 1978;83:361-2
5. Nagraj S, Sinha S, Grant H, Lakhoo K, Hitchcock R, Johnson P. The incidence of complications following primary inguinal herniotomy in babies weighing 5 kg or less. Pediatr Surg Int. 2006;22:500-2
6. Pedersen J. Prefertile vas lesion as a cause of sperm antibody formation: an experimental and clinical study. Scand J Urol Nephrol Suppl. 1987;106:1-38
7. Powell RW. Intraoperative diagnostic pneumoperitoneum in pediatric patients with unilateral inguinal hernias: the Goldstein test. J Pediatr Surg. 1985;20:418-21
8. Sozubir S, Ekingen G, Senel U, Kahraman H, Guvenc BH. A continuous debate on contralateral processus vaginalis: evaluation technique and approach to patency. Hernia. 2006;10:74-8
9. Burd RS, Heffington SH, Teague JL. The optimal approach for management of metachronous hernias in children: a decision analysis. J Pediatr Surg. 2001;36:1190-5
10. Holcomb GW 3rd, Miller KA, Chaignaud BE, Shew SB, Ostlie DJ. The parental perspective regarding the contralateral inguinal region in a child with a known unilateral inguinal hernia. J Pediatr Surg. 2004;39:480-2 discussion -2
11. Tackett LD, Breuer CK, Luks FI, Caldamone AA, Breuer JG, DeLuca FG. et al. Incidence of contralateral inguinal hernia: a prospective analysis. J Pediatr Surg. 1999;34:684-7 discussion 7-8
12. Zamakhshardy M, Ein A, Ein SH, Wales PW. Predictors of metachronous inguinal hernias in children. Pediatr Surg Int. 2009;25:69-71
13. Chertin B, De Caluwe D, Gajaharan M, Piaseczna-Piotrowska A, Puri P. Is contralateral exploration necessary in girls with unilateral inguinal hernia? J Pediatr Surg. 2003;38:756-7
14. Schier F, Montupet P, Esposito C. Laparoscopic inguinal herniorrhaphy in children: a three-center experience with 933 repairs. J Pediatr Surg. 2002;37:395-7
15. Tsai YC, Wu CC, Yang SS. Open versus minilaparoscopic herniorrhaphy for children: a prospective comparative trial with midterm follow-up evaluation. Surg Endosc. 2010;24:21-4
16. Becmeur F, Dimitriu C, Lacreuse I, Boeyeldieu L, Moog R, Kauffmann I. et al. Laparoscopic treatment of congenital inguinal hernias in children (212 patients). Arch Pediatr. 2007;14:985-8
17. Rothenberg RE, Barnett T. Bilateral herniotomy in infants and children. Surgery. 1955;37:947-50
18. Klin B, Efrati Y, Abu-Kishk I, Stolero S, Lotan G. The contribution of intraoperative transinguinal laparoscopic examination of the contralateral side to the repair of inguinal hernias in children. World J Pediatr. 2010;6:119-24
19. Antonoff MB, Kreykes NS, Saltzman DA, Acton RD. American academy of pediatrics section on surgery hernia survey revisited. J Pediatr Surg. 2005;40:1009-14
20. Lobe TE, Schropp KP. Inguinal hernias in pediatrics: initial experience with laparoscopic inguinal exploration of the asymptomatic contralateral side. J Laparoendosc Surg. 1992;2:135-40 discussion 41
21. Lotan G, Efrati Y, Stolero S, Klin B. Transinguinal laparoscopic examination: an end to the controversy on repair of inguinal hernia in children. Isr Med Assoc J. 2004;6:339-41
22. Schier F, Danzer E, Bondartschuk M. Incidence of contralateral patent processus vaginalis in children with inguinal hernia. J Pediatr Surg. 2001;36:1561-3
23. Niyogi A, Tahim AS, Sherwood WJ, De Caluwe D, Madden NP, Abel RM. et al. A comparative study examining open inguinal herniotomy with and without hernioscopy to laparoscopic inguinal hernia repair in a pediatric population. Pediatr Surg Int. 2010;26:387-92
24. Zhong H, Wang F. Contralateral metachronous hernia following negative laparoscopic evaluation for contralateral patent processus vaginalis: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2014;24:111-6
25. Lawrenz K, Hollman AS, Carachi R, Cacciaguerra S. Ultrasound assessment of the contralateral groin in infants with unilateral inguinal hernia. Clin Radiol. 1994;49:546-8
26. Hata S, Takahashi Y, Nakamura T, Suzuki R, Kitada M, Shimano T. Preoperative sonographic evaluation is a useful method of detecting contralateral patent processus vaginalis in pediatric patients with unilateral inguinal hernia. J Pediatr Surg. 2004;39:1396-9
27. Hasanuzzaman SM, Chowdhury LH, Sarker RN, Bari MS, Talukder SA, Islam MK. Ultrasonographic evaluation of contralateral exploration of patent processus vaginalis in unilateral inguinal hernia. Mymensingh Med J. 2011;20:192-6
28. Kaneda H, Furuya T, Sugito K, Goto S, Kawashima H, Inoue M. et al. Preoperative ultrasonographic evaluation of the contralateral patent processus vaginalis at the level of the internal inguinal ring is useful for predicting contralateral inguinal hernias in children: a prospective analysis. Hernia. 2015;19:595-8
29. K.M.A. Dreuning, C.E.M. ten Broke, J.W.R. Twisk, S.G.F. Robben, R.R. van Rijn, J.I.M.L. Verbeke, et al. Diagnostic accuracy of preoperative ultrasonography in predicting contralateral inguinal hernia in children: a systematic review and meta-analysis. European Radiology. 2018 published online
30. Wataru S, Yoshio W, Hidemi T, Kazuo O, Naoko K. Incidence of contralateral patent processus vaginalis in relation to age at laparoscopic percutaneous extraperitoneal closure for pediatric inguinal hernia. Surgery Today. 2016;46:466-70
Author contact
![]() Corresponding author: Won Yong Choi, MD, PHD, Department of surgery, KonKuk University Chungju Hospital, 6 Gwangmyeong 1-gil, Chungju-si, Chungcheongbuk-do, Republic of Korea. E-mail: wycoolnet
Corresponding author: Won Yong Choi, MD, PHD, Department of surgery, KonKuk University Chungju Hospital, 6 Gwangmyeong 1-gil, Chungju-si, Chungcheongbuk-do, Republic of Korea. E-mail: wycoolnet

 Global reach, higher impact
Global reach, higher impact