Impact Factor
ISSN: 1449-1907
Int J Med Sci 2018; 15(11):1092-1097. doi:10.7150/ijms.26972 This issue Cite
Research Paper
Study on the classification of Descemet membrane detachment after cataract surgery with AS-OCT
1. Shenzhen Eye Hospital, School of Optometry & Ophthalmology of Shenzhen University, Shenzhen Key Laboratory of Department of Ophthalmology, Shenzhen, 518000, China
2. Tissue Tech, Inc., Ocular Surface Center, and Ocular Surface Research & Education Foundation, Miami, FL 33173, USA
Received 2018-4-30; Accepted 2018-6-5; Published 2018-6-23
Abstract
In this article, the significance of anterior segment optical coherence tomography (AS-OCT) to aid the clinical diagnosis and treatment of Descemet membrane (DM) detachment after phacoemulsification combined with intraocular lens implantation was retrospectively analyzed using 26 patients (26 eyes). The location and scope of DM detachment, its causative factors and the percentage of each detachment type are considered for clinical treatments. Based on the location and scope, the detachment can be divided into three types: (1) simple, (2) symmetrical and (3) complete DM detachment. Simple detachment, confined to the area of surgical incision (detachment range <1/4 corneal area), occurred in 69.20 % of cases (18/26), in which the DM detachment in the anterior lip accounted for 42.30% (11/26) and in the posterior lip accounted for 26.90% (7/26). Symmetrical DM detachment, referring to detachment (1/4 cornea area < detached area <1/2 corneal area) that appeared symmetrically on the surgical incision and the opposite site, accounted for 19.20% (5/26). Complete DM detachment (>1/2 of the corneal area), accounted for 11.50% (3/26). Interestingly, our findings suggest that the DM detachment after phacoemulsification is closely related to the location (simple and symmetrical DM detachment) and the skillfulness (complete DM detachment) of the surgical incision. Therefore, appropriate classification of DM detachment by AS-OCT and wise selection of surgical location can better guide cataract surgery in the future.
Keywords: anterior segment optical coherence tomography (AS-OCT), corneal descension, cataract, phacoemulsification, Descemet membrane detachment
Introduction
Cataract is one of the major causes of blindness worldwide [1]. In China, more than half of the 500 million cases of blindness will be due to cataract failure by 2020 [2]. Up till now, surgery is the only effective treatment for cataract-related blindness [3]. Manual small incision cataract surgery and phacoemulsification are the most common cataract surgery methods [4]. This operation has its advantages of smaller intraoperative incision, shorter operative time, quicker recovery of visual acuity and smaller astigmatism. However, intraoperative and postoperative complications may affect the visual acuity recovery. The detachment of the Descemet membrane (DM) is one of the major post-operative complications of phacoemulsification. It manifests as persistent edema of the cornea after surgery, which can cause corneal endothelial decompensation in severe cases and affect the prognosis of vision in surgical patients.
The purpose of this study is to analyze anterior segment optical coherence tomography (AS-OCT) results of Descemet membrane detachment after phacoemulsification and to classify the detachment in combination with clinical manifestations, for further guidance of its clinical treatment.
Materials and Methods
Patient Information
A total of 26 patients (26 eyes) with persistent corneal edema and DM detachment at Shenzhen Eye Hospital from August 2013 to August 2017 participated in this study. Among the cases, there were 11 females (11 eyes) and 15 males (15 eyes), 12 left eyes (12 eyes) and 14 right eyes (14 eyes), 4 cases (4 eyes) with ocular trauma, 3 cases (3 eyes) with glaucoma, 2 cases (2 eyes) with uveitis and 1 case (1 eye) with Fuchs corneal dystrophy.
Surgery
The surgeries were performed by the same surgeon, Ping Guo with the assistance of her team.
Methods
(1) Technical Parameters of AS-OCT: AS-OCT instrument was obtained from Modin Corporation (Erie, PA). Its components included OCT mainframe, computer, monitor, lifting table, host by the internal power supply, the light source, two-dimensional removable chin support and the eye probe. Light source was super-luminescent light-emitting diode with the scanning mode of 1310 mm. Anterior segment scan mode included single, reticle and four-line scan and adjustable eight-line scan. Scan angle could be adjusted as needed, 256A-scans / B-scans. Collection time was 0.65s for obtaining the regional maximum, minimum and average corneal thickness and anterior eye image. The resulting image had a vertical resolution of 15 μm and a lateral resolution of 20 μm.
(2) AS-OCT examination method: The operator inputed the patient's personal information in the device control interface first. Then the examinee's head rested on the support to keep it motionless. The examiner adjusted the chin left and right and up and down until the measured eye was aligned to the probe. The front and the rear of the probe was adjusted to achieve optimal focus and then the capture button was pushed on the device to automatically capture and record images with different resolutions through intuitive display of various layers of cornea morphology, anterior chamber, iris, lens and other structures.
(3) The data of the patients with phacoemulsification and subsequent persistent corneal edema in Shenzhen Ophthalmic Hospital from August 2013 to August 2017 were collected. The final diagnosis of the detachment from those patients are confirmed by clinical manifestations and AS-OCT examination. According to the location and the scope of the detachment, the percentage of each type was classified and its causative relationship was analyzed.
Results
1. Patient age: The patient ages were between 65 and 86, with an average of 77.04 ± 5.51 years old. Among them, 3 cases aged from 65 to 69 years old, 6 cases from 70 to 74 years old, 9 cases from 75 to 79 years old, 6 cases from 80 to 84 years old, and 2 cases from >85 years old. Patients over the age of 70 accounted for 88.50% (23/26).
2. Clinical manifestation and classification: According to the degree of visual acuity and corneal edema one week after surgery, three types of DM detachment after cataract surgery were identified: (1) simple detachment, (2) symmetrical detachment, and (3) complete detachment.
Simple detachment of Descemet membrane. A. Corneal stromal edema a week after cataract removed by phacoemulsification and IOL implanted after surgery temporal side-cut out. B. Corneal stromal edema after cataract surgery. The detachment of DM was difficult to see under the slit lamp.
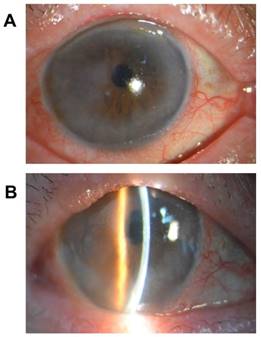
(1) Simple DM detachment: The local corneal edema in the main incision area (lesion area < 1/4 cornea) and the DM folds were observed. Under this situation, it was difficult to distinguish the existence of the DM detachment and the extent of detachment under the slit lamp (Figure 1). The corneas were transparent in the central area of these patients, with mild anterior chamber reaction. The average postoperative visual acuity was 0.60 ± 0.25 (Table 1).
(2) Symmetrical DM detachment: symmetrical corneal stroma edema (corneal thickness 2CT ~ 2.5CT) was accompanied by focal corneal epithelial small blisters or obvious folds of DM. However, it was difficult to see aqueous flare [the floating debris under a slit lamp (Figure 2)]. The aqueous flare was + ~ + +, and the average postoperative visual acuity was 0.40 ± 0.16 (Table 1).
Different types of DM detachment
| Simple detachment | Symmetric detachment | Complete detachment | |
|---|---|---|---|
| Case | 18 | 5 | 3 |
| Edema Site | The main part of incision | The main part of incision and the opposite site | Virtually the whole cornea |
| Epithelial blister | No | Local small blisters | The diffused blisters |
| Thickness of the cornea | >2 CT | 2 to 2.5 CT | > 2.5 CT |
| Aqueous flare | + | + to ++ | ++ to +++ |
| The average post-operative Vision | 0.6 ± 0.25 | 0.4 ± 0.16 | 0.1 ± 0.04 |
| Percentage | 69.20% | 19.20% | 11.50% |
Symmetrical detachment of Descemet membrane. A. Corneal stromal edema (++) one week after cataract surgery. The temporal side of the corneal epithelial layer was visible for small blisters. B. Corneal stromal edema (++) after cataract surgery. It was difficult to determine the accurate range of detachment of DM.
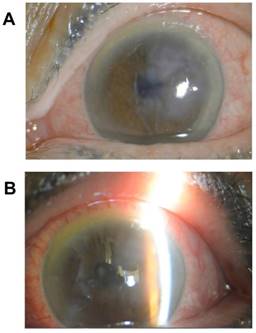
Complete detachment of Descemet membrane. The corneal stromal edema (++) and foam-like spots after cataract surgery. Corneal endothelial cells lost function permanently.
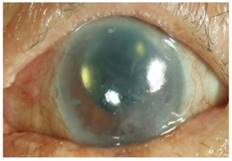
(3) Complete DM detachment: A large area of cornea (> 1/2 cornea) matrix suffered from full-thickness edema and opacity. The corneal thickness was > 2.5CT, accompanied by corneal epithelial diffuse blisters. It was clear to see aqueous flare [the floating debris under a slit lamp (Figure 3)]. The aqueous flare is + +~ + ++, and the average postoperative visual acuity was 0.10 ± 0.04 (Table 1).
3. AS-OCT examination: AS-OCT examination showed that the above three types of detachment after cataract surgery were closely related with the surgical incision, in their locations and scope.
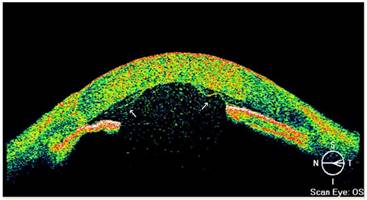
(1) Simple detachment: The Descemet membrane showed local detachment (<1/4 corneal area) at the surgical incision site, which accounted for 69.20% (18/26) of the total number of cases (Table 1). Among them, the local detachment of DM below the anterior incision site accounted for 42.30% (11/26). AS-OCT showed significant stromal edema at the incision site, separation of the DM and corneal stromal layer at the anterior incision site, detached DM floating in the anterior chamber, and the DM and the stromal layer opened an angle toward the central area of the cornea (Figure 4A). In addition, the posterior lip under the incision posteriorly accounted for 26.90% (7/26). AS-OCT showed thickening of the stromal edema at the corneal incision site and separation of the DM from the corneal stroma after incision. The separated DM floated in the anterior chamber and the opening of the DM and the stromal layer was toward the central corneal area (Figure 4B, Figure 4C).
AS-OCT results of simple detachment of Descemet membrane. A. Edema and thickening at the temporal side of the right eye shown by AS-OCT. Simple detachment of the DM was present at the anterior incision site (arrow). B. AS-OCT showed mild edema at the corneal stroma layer at the nose site of the left eye. The simple detachment of DM was seen at the anterior incision site (arrow). C. AS-OCT showed stromal edema at the nosal site of the left eye, visible large corneal epithelial blisters and simple detachment of the DM (arrow).
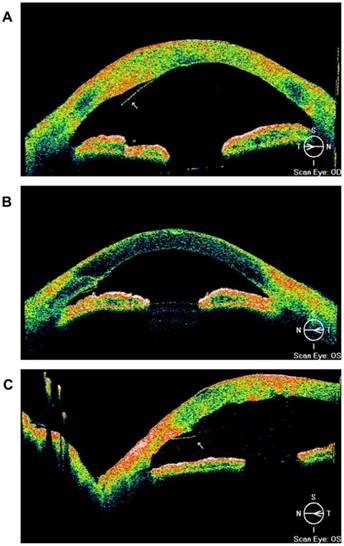
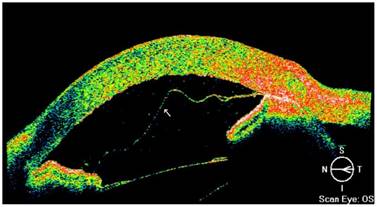
(2) Symmetrical detachment: The detachment was in the limbal area (1/4 cornea area <detached area <1/2 corneal area) that appeared symmetrically on the surgical incision and the opposite sites, which accounted for 19.20% of the total number of cases (5/26, Table 1). AS-OCT examination revealed the local stromal edema at the corneal incision site, separation of the DM and corneal stroma layer, detached DM floating in the anterior chamber and thickening of the corneal stromal layer due to edema at the opposite of the incision site. At the same time the DM and the stromal layer were detached. The detached DM floated in the anterior chamber, and many fine granular exudates were in the anterior chamber (Figure 5).
(3) Complete detachment: The detachment referred to the total detachment of the Descemet membrane (more than 1/2 of the corneal area), which accounted for 11.50% of total cases (3/26, Table 1). AS-OCT showed corneal stroma thickening with obvious edema. The DM was almost completely separated from the corneal stroma layer. The detached DM floated in the anterior chamber partially touching the iris surface, and in the severe case, corneal endothelial dysfunction was observed (Figure 6).
AS-OCT results of symmetric detachment of Descemet membrane. AS-OCT showed corneal stromal edema and thickening, symmetric detachment of DM at the incision and opposite of the incision sites (arrow).
AS-OCT results of complete detachment of Descemet membrane. AS-OCT showed corneal stroma edema and thickening in the left eye, with complete detachment of the DM and the stromal layer, and the DM floated in the anterior chamber (arrow).
Discussion
Due to the increasing popularity of cataract surgery, postoperative reports of corneal Descemet membrane detachment are common. The rate of post-cystectomy conjunctival detachment was 2.6%, while the incidence of phacoemulsification was about 0.5% [5]. Most of detachment of mild to moderate corneal DM could be self-healing. However, some detachment is complicated with folding, curly or complete detachment of the DM causing refractory corneal stromal edema or even corneal endothelial dysfunction with severe decrease of visual acuity. The etiology for the detachment of the corneal DM mainly includes the following aspects: (1) losing attachment between the DM and the anterior stromal layer anatomically. The two layers can be easily separated under external force. Because of their termination on the Schwalbe line, the location of phacoemulsification cataract autograft incision in the clear cornea, and the tendency of corneal intraoperative incisions into the anterior chamber, these forces may create lateral traction and cause separation of loosely attached DM [6]. (2) For the surgical instruments, if the disposable and reusable tools are not sharp, the inappropriate force to penetrate the corneal inner tissue easily leads to separation of the DM from the stromal layer or enlargement of the gap between the two layers, a hidden danger for detachment. In addition, if the microscope depth of field is too small, the detached DM may be mistakenly identified as the anterior capsule and thus sucked out, causing a wide range of DM detachment. (3) For the surgical skills, if the surgeon is less skilled or if the surgery is too difficult, the surgical device may be repeatedly placed into and out of the anterior chamber causing liquid infiltration between the two layers. All these factors may increase the risk of detachment of the DM [7], however (4) patients themselves may also increase the risk of the detachment. In this study, 88.5% (23/26) of patients were over 70 years of age, indicating that the older patients are prone to detachment of the DM. In the case of Fuchs corneal endothelial dystrophy, the adhesion between the two layers are decreased. They are prone to detachment under the impact of high water flow. In the case of poor patient cooperation or light anesthesia, the patients may move their eyes suddenly to cause damage of the corneal DM, causing postoperative detachment. Even some ocular trauma after surgery can lead to delayed DM detachment [8, 9].
AS-OCT is an optical, non-contact, ophthalmic imaging device that enables tomographic and quantitative measurement of the entire anterior segment structure [10]. The principle is based on the optical scattering of different ocular tissue structures, using interferometry for two-dimensional imaging and quantitative analysis. AS-OCT examination is an optical penetrating examination not affected by corneal edema, and can easily be used to find DM detachment while the conventional slit lamp cannot [11]. AS-OCT is of high resolution, accurate to the micron level, which can clearly distinguish the layers of the corneal tissue structure. At the same time due its non-invasiveness, AS-OCT can minimize the incidence of eye surgery infection, especially in early postoperative patients, which can intuitively be used for determination of the probable causes and proposal of the appropriate treatments. In this study, the location and scope of the detachment of the DM can be clearly distinguished by AS-OCT. The simple DM detachment, referring to the detachment at the surgical incision (Figure 1), can be divided into detachments in the anterior and posterior incision sites. In symmetrical DM detachment, the detachment was present in the corneal incision site and the site opposite of incision (Figure 2). Symmetrical DM detachment was most likely caused by preexisting intrinsic abnormality in stromal adherence to the Descemet membrane or long-term shear force caused by aqueous humor entrance to the periphery that never reached complete detachment due to positive pressure [12, 13]. The detachment ranged from 1/4 to 1/2 of the corneal area. The complete detachment of DM refers to the detachment of more than 1/2 of the cornea (Figure 3). In the past, the grading standards for the detachment were created by Liu Zuguo in 1990 [14]. That is, detachments were divided into five grades: the detachment range less than 1/8 cornea was local, the detachment range greater than 1/8 but less than 1/4 cornea was mild, the detachment range greater than 1/4 but less than 1/2 was moderate, the detachment range equal to or greater than 1/2 was severe, and the complete detachment was full. Due to limitation of the equipment at that time, the previous classification was based on rough estimation of the extent of corneal edema and the range of detachment of DM. Therefore, it is difficult to determine the precise location of DM detachment. In contrast, the current AS-OCT [15] can accurately distinguish the location and the extent of the DM detachment (Figure 4-Figure 6), and suggest a close relationship between the detachment and the incision of DM. Therefore, our classification, combined with the site and the range of the detachment, helps analyze the cause and severity of DM detachment. Such a method is beneficial for guidance of the clinical diagnosis and the treatment of DM detachment.
Corneal persistent edema and its progressive increase after cataract surgery should be an indicator of possible detachment of the Descemet membrane after exclusion of intraocular pressure and other factors. AS-OCT examination can be clearly used for observation of the position and the range of DM detachment. Simple detachment and more complicated detachment of DM can be treated successfully by strengthening the nutrition of the cornea and adopting symptomatic treatment of edema. In such cases, most patients with DM detachment can gradually repair themselves. If the detachment is combined with DM curls, folds or the detachment is complete, surgery is recommended as soon as possible to avoid excessive loss of endothelial cells and thus the occurrence of bullous keratopathy [16]. Sterile air or C3F8 can be injected into the corneal anterior chamber during surgery [17-19]. According to the orientation of the detachment, the patients should take a semi-recumbent or lateral position to rest. At the same time, 200g / L mannitol or oral methazolamide can be used to reduce the intraocular pressure. Such a combination can be adopted to achieve good therapeutic effect [20].
In summary, DM detachment after phacoemulsification is associated with a variety of factors. AS-OCT examination can be used to find clear detachment of the DM. The position of detachment and surgical incision were found to be closely related. The location and the scope of detachment can be used to guide clinical treatments and improve prognosis of patients.
Acknowledgements
Supported by Grant 2015A030313774, Natural Science Fund of Guangdong Province, China.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Oliva MS, Schottman T, Gulati M. Turning the tide of corneal blindness. Indian J Ophthalmol. 2012;60:423-7
2. WHO. Blindness as a public health problem in China. 2018.
3. Mohamed A, Gilliland KO, Metlapally S, Johnsen S, Costello MJ. Simple fixation and storage protocol for preserving the internal structure of intact human donor lenses and extracted human nuclear cataract specimens. Mol Vis. 2013;19:2352-9
4. Jongsareejit A, Wiriyaluppa C, Kongsap P, Phumipan S. Cost-effectiveness analysis of manual small incision cataract surgery (MSICS) and phacoemulsification (PE). J Med Assoc Thai. 2012;95:212-20
5. Khng CY, Voon LW, Yeo KT. Causes and management of Descemet's membrane detachment associated with cataract surgery-not always a benign problem. Ann Acad Med Singapore. 2001;30:532-5
6. Wang T. Analysis and treatment of detachment of corneal posterior elastic layer during cataract phacoemulsification. International Journal of Ophthalmology. 2014;8:1511-2
7. Cui Y. Clinical observation of phacoemulsification combined with intraocular lens implantation led to the detachment of Descemet membrane. Chinese Journal of Ophthalmology (Electronic Version). 2014;1:1-10
8. Morkin MI, Hussain RM, Young RC, Ravin T, Dubovy SR, Alfonso EC. Unusually delayed presentation of persistent Descemet's membrane tear and detachment after cataract surgery. Clin Ophthalmol. 2014;8:1629-32
9. Shalchi Z, O'Brart DP, Ilari L. Bilateral descemet membrane detachment following cataract surgery. JAMA Ophthalmol. 2013;131:533-5
10. Liu J, Yao X, Li M. Application of panoramic anterior ocular OCT in the occult corneal posterior vitreous detachment after cataract surgery. Chinese Journal of Practical Ophthalmology. 2014;32:732-4
11. Zhou SY, Wang CX, Cai XY, Liu YZ. Anterior segment OCT-based diagnosis and management of Descemet's membrane detachment. Ophthalmologica. 2012;227:215-22
12. Gatzioufas Z, Schirra F, Low U, Walter S, Lang M, Seitz B. Spontaneous bilateral late-onset Descemet membrane detachment after successful cataract surgery. J Cataract Refract Surg. 2009;35:778-81
13. Banitt MR, Malta JB, Shtein RM, Soong HK. Delayed-onset isolated central Descemet membrane blister detachment following phacoemulsification. J Cataract Refract Surg. 2008;34:1601-3
14. Liu Z, Peng HLM, Lin Z. Cataract postoperative removal of corneal Descemet membrane (report of 11 cases). Journal of Practical Ophthalmology. 1990;6:17-21
15. Osman EA. The benefit of ultrasound biomicroscopy (UBM) in management of total Descemet's membrane detachment after deep sclerectomy surgery. Int Ophthalmol. 2011;31:345-8
16. Sukhija J, Ram J, Kaushik S, Gupta A. Descemet's membrane detachment following phacoemulsification. Ophthalmic Surg Lasers Imaging. 2010;41:512-7
17. Datar S, Kelkar A, Jain AK, Kelkar J, Kelkar S, Gandhi P. et al. Repeat Descemetopexy after Descemet's Membrane Detachment following Phacoemulsification. Case Rep Ophthalmol. 2014;5:203-6
18. Fan NW. Outcomes of repeat descemetopexy in post-cataract surgery descemet membrane detachment. Am J Ophthalmol. 2014;157:1330-1
19. Jain R, Murthy SI, Basu S, Ali MH, Sangwan VS. Anatomic and visual outcomes of descemetopexy in post-cataract surgery descemet's membrane detachment. Ophthalmology. 2013;120:1366-72
20. Lin C, Yu C. A large range of elastic membrane after perfusion of perfluoropropane injection of anterior chamber. Ophthalmology and Otolaryngology. 2010;3:174-5
Author contact
![]() Corresponding authors: Xinhua Liu, Shenzhen Eye Hospital, Zetian Road 18, Room 421, Futian District, Shenzhen, 518000, China. Tel 08613728686624; Fax 08675523959500; Email: xhualiucom or Hongbo Cheng, Shenzhen Eye Hospital, Zetian Road 18, Room 421, Futian District, Shenzhen, 518000, China. Tel 08613924659029; Fax 08675523959500; Email: 2607212858com
Corresponding authors: Xinhua Liu, Shenzhen Eye Hospital, Zetian Road 18, Room 421, Futian District, Shenzhen, 518000, China. Tel 08613728686624; Fax 08675523959500; Email: xhualiucom or Hongbo Cheng, Shenzhen Eye Hospital, Zetian Road 18, Room 421, Futian District, Shenzhen, 518000, China. Tel 08613924659029; Fax 08675523959500; Email: 2607212858com

 Global reach, higher impact
Global reach, higher impact