3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2013; 10(3):243-249. doi:10.7150/ijms.3971 This issue Cite
Research Paper
Comparison of Natural Course, Intravitreal Triamcinolone and Macular laser photocoagulation for Treatment of Mild Diabetic Macular Edema
Department of Ophthalmology, Hallym University Sacred Heart Hospital, Anyang, Korea.
Received 2012-10-23; Accepted 2013-1-9; Published 2013-1-21
Abstract
Purpose: To assess the natural course of the mild diabetic macular edema(DME) and to compare the visual outcomes with the patients with receiving either macular laser photocoagulation or intravitreal injection of triamcinolone acetonide(IVTA).
Methods: 28 eyes with central macular thickness (CMT) of between 250 to 300µm were followed without treatment and 48 eyes with CMT between 300 to 500µm had been divided into 3 subgroups according to treatment. We evaluated the best corrected visual acuity (BCVA) and CMT of natural course group and compared the BCVA and CMT of the patients who had been treated with IVTA or macular laser treatment.
Results: The eyes with DME between 250 to 300µm showed no significant change in BCVA and CMT at 6 month. Among the eyes with DME between 300 to 500µm, all 3 subgroups showed no statistically significant change of BCVA at any follow up period and no significant difference was revealed among the subgroups. All subgroups showed significant reduction of CMT after 1 month and maintained until final follow-up and there was no significant difference among subgroups.
Conclusions: Mild DME between 250 to 500µm did not show significant worsening of BCVA or macular edema without any specific treatment.
Keywords: Diabetic Macular Edema, Intravitreal triamcinolone, Macular laser photocoagulation.
Introduction
Diabetic macular edema (DME) is one of the common causes of visual loss in patients with diabetes [1]. In the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) [2], the 10-year cumulative incidence of macular edema was 20.1 % and 25.4% among those with type 1 diabetes and type 2 diabetes treated with insulin, respectively. The Early Treatment Diabetic Retinopathy Study (ETDRS) defined DME as retinal thickening or presence of hard exudates within 1 disk diameter of the center of the macula [3]. To characterize the severity of macular edema and for treatment guidelines, the term clinically significant macular edema (CSME) is used. ETDRS recommended prompt photocoagulation for CSME, but defer for eyes with edema that is more remote from macular center. However, ETDRS diagnosed retinal thickening using fundus contact lens biomicroscopy which is subjective and relatively insensitive to subtle changes in mild macular edema [4].
Optical coherence tomography (OCT) generates cross-sectional or three-dimensional images. It is a noninvasive, noncontact imaging modality that allows quantitative measurements of retinal volume. Compared to clinical examination, OCT is a more sensitive and specific method for objective evaluation of macular edema. The retinal thickness at the central fovea with DME is 250 to more than 1000 μm, whereas normally the retinal thickness is approximately 180~210 μm [5].
Though macular laser photocoagulation has been the mainstay for treating DME, several alternative treatments have emerged over the last few years. Intravitreal injection of triamcinolone acetonide (IVTA) has been suggested by several authors for the treatment of DME [6-8].
ETDRS reported that DME tended to be a chronic disease and spontaneous visual recovery was unusual. If untreated, 29% of eyes with DME and subfoveal involvement experience moderate visual loss after 3 years and visual recovery with improvement of 3 ETDRS lines occurred in 5% of cases. However, the clinical courses of DME in ETDRS were lumped together from 250 μm to 1000 μm due to the subjective clinical diagnosis. Moreover, one study reported that mild DME showed worse response than moderate DME to laser treatment [9].
We assumed that the mild DME would show different clinical course from severe DME and that the management of DME should be different according to degree of macular edema.
Therefore, it was the purpose of the present investigation to assess the natural course of the mild to moderate DME under 500 μm using OCT and to compare the visual outcomes with the patients with receiving either macular laser photocoagulation or intravitreal triamcinolone.
Subjects and Methods
The medical records of 76 eyes of 76 patients with DME who visited Hallym University Sacred Heart hospital between January 2004 and December 2009 were analyzed retrospectively. Only patients with baseline central macular thickness (CMT) of between 250 μm and 500 μm measured by Optical coherence tomography (Stratus OCT, Carl Zeiss Meditec, Dublin, CA, USA), follow-up period ≥ 6 months were included in this study. The patients who already had treated with vitrectomy, macular laser photocoagulation or other intravitreal injections were excluded. Eyes with other diseases affecting best corrected visual acuity (BCVA), presence of neovascularization or macular ischemia on the basis of fluorescein angiography were also excluded. Mild macular edema case usually showed minimal increase of thickness under 300 μm, so we divided the patients based on the baseline CMT into 2 groups: 1) Group 1 with CMT of between 250 μm to 300 μm; 2) Group 2 with CMT of between 300 μm to 500 μm.
The patients with group 1 were followed without any treatment, and all patients in group 2 were recommended to be treated with either intravitreal triamcinolone or macular laser photocoagulation after informed consent and received the treatment that the patient chose within 1 week, but some of the patients refused treatment against the medical advice because of the risk of complications, financial difficulty, uncertainty of treatment, private reasons and so on. Therefore, the patients with group 2 could be divided into 3 subgroups according to their choices: 1) treatment with intravitreal triamcinolone (IVTA group), 2) treatment with focal or grid laser photocoagulation (laser group), 3) observation without specific treatment (natural course group).
Macular laser photocoagulation was underwent by the guideline of ETDRS.3
All leaking microaneurysms in the edematous retina between 500 and 3000 μm from the center of macula were treated. Individual microaneurysm were treated with a spot size of 50 to 100 μm and an exposure time of 0.1 s. The minimal power was applied to obtain either whitening or darkening of microaneurysm. The grid treatment was primarily used for areas of diffuse leakage with no identifiable focal areas of leakage. The grid was composed of light intensity burns, 50 to 100 μm in diameter producing a grid of equally spaced burns more than on burn-width apart.
Intravitreal injections were performed under sterile conditions. Topical anesthetic drops were instilled, cleaning of the injection site with 5% povidone iodide, and a 30-gauge needle was inserted through the pars plana 4mm posterior to limbus. The dose was 4.0mg of triamcinolone acetonide (Shin Poong Pharmaceuticals CO Ltd., Triam®, 40 mg/ml/vial). Following the injection, an antibiotic ointment was administered and the eye was patched overnight. After intravitreal injection, patients were prescribed to administer a topical antibiotic eye drop for three days routinely and monitored for potential injection-related complication at 1, 3 and 7 days after injection.
We evaluated BCVA and CMT of all patients and compared among the groups. For all patients, the follow-up visits were scheduled every month after the day when macular edema was diagnosed and follow-up examinations for comparison of each group were performed 1, 3, 6months after the day of recommendation of treatment such as intravitreal triamcinolone or macular laser photocoagulation. Baseline and follow-up examinations included ophthalmologic examination, BCVA, and an OCT examination Retreatment, when indicated, was performed within four weeks after the follow-up visit (usually on the same day as the follow-up visit). Macular thickness was increased 100 μm more than last examination or persistent despite the treatment were criteria for retreatment.
For statistical analysis, the BCVA were converted to the logarithm of the minimum angle of resolution (log MAR). Baseline demographics were compared using Kruskal-Wallis test and Χ2 test.
Comparisons of differences between baseline and follow-up data within each group were performed using Wilcoxon Matched-Pairs Signed-Ranks test, and comparisons between each group were by repeated measurement analysis. Statistical analysis was performed with SPSS for windows, version 13 (SPSS, Inc., Chicago, IL, USA) and the level of statistical significance was set at p<0.05.
This study was done in adherence to the tenets of the Declaration of Helsinki and informed consent was obtained. Approval for this study was obtained from the Institutional Review Board
Results
Among total of 76 patients, 28 eyes of 28 patients had been allocated to group 1 with CMT of between 250 μm to 300 μm, and 48 eyes of 48 patients had been enrolled in group 2 with CMT between 300 μm to 500 μm. Among 48 eyes of group 2, 15 eyes received intravitreal triamcinolone (IVTA group), 16 eyes underwent macular laser photocoagulation (laser group), and 17 eyes were followed without any treatment (natural course group).
Baseline characteristics of the patients in each group are summarized in Table 1. There was no significant difference concerning age, sex, baseline BCVA and baseline CMT.
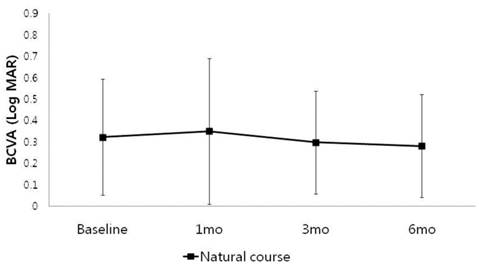
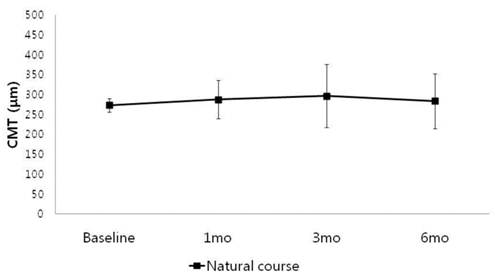
In Group 1(250 to 300 μm), the mean visual acuity improved from 0.32 logMAR to 0.28 logMAR at 6 month, and mean macular thickness slightly increased from 274 μm to 284 μm at 6 month, but they were not statistically significant (p= 0.533, 0.480) (Table 2, Fig 1,2).
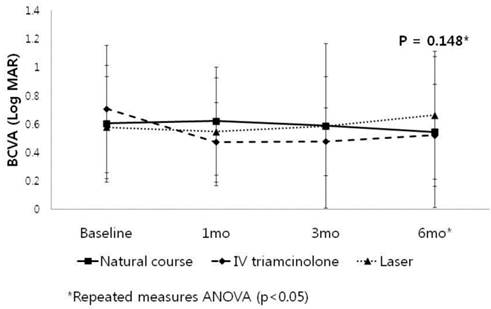
In Group 2(300 to 500 μm), only IVTA group seemed to have improvement of BCVA at 1 and 3 month after injection (p=0.097, 0.089, respectively), but no subgroup showed statistically significant change of BCVA at any follow-up visits (Table 2). In among-group comparison, no significant difference was revealed through the follow-up period (repeated measurement analysis, p=0.148) (Table 2, Fig 3,4).
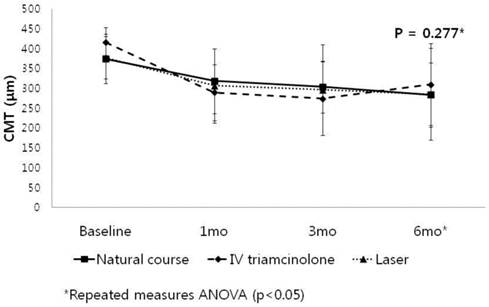
When it comes to central macular thickness, all subgroups showed significant reduction of central macular thickness (p< 0.05) after 1 month and maintained until final follow up. In among-group comparison, there was no statistical significance through all follow-up period (repeated measurement analysis, p=0.277).
The mean intraocular pressure of IVTI group was 14.07±2.31 mmHg on baseline and 14.40±2.85 mmHg, 14.33±2.82 mmHg, 14.20±2.70 mmHg at 1 month, 3 month, 6 month follow-up. There were no significant changes between baseline and each follow-up intraocular pressure (p=0.417, 0.469, 0.737). Until the end of follow-up, elevated intraocular pressure over 21mmHg were seen in 1 eye of IVTA group and controlled by topical therapy. A quick progression of cataract was noted in 1 eye of IVTA group but was not so serious to receive cataract surgery. There was no remarkable complication in laser group.
Baseline characteristics of all patients.
| Subgroups | Natural course | IVTA | Laser | p-value |
|---|---|---|---|---|
| Patients(eyes) | 45(45) | 15(15) | 16(16) | |
| Age(yr) | 59.21±10.37 | 59.40±7.50 | 61.75±11.14 | 0.803* |
| Sex(M:F) | 17: 18 | 5 : 10 | 5 : 11 | 0.914† |
| BCVA(logMAR) | 0.50±0.48 | 0.71±0.45 | 0.58±0.36 | 0.786 |
| CMT(μm) | 313.86±54.25 | 416.80±38.00 | 378±53.62 | 0.093 |
IVTA: intravitreal injection of triamcinolone acetonide; BCVA: best corrected visual acuity; CMT: central macular thickness
*Kruskal-Wallis test (p<0.05)
†Χ2 test (p<0.05)
Changes in BCVA and CMT of each group.
| Baseline CMT | 250μm-300μm | 300μm - 500μm | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Natural course (n=28) | Natural course (n=17) | IVTA (n=15) | Laser (n=16) | p-value* | |||||
| BCVA (logMAR) | p-value† | p-value† | p-value† | p-value† | |||||
| Baseline | 0.32±0.27 | 0.61±0.41 | 0.71±0.45 | 0.58±0.36 | 0.643 | ||||
| 1 month | 0.35±0.34 | 0.741 | 0.62±0.38 | 0.906 | 0.48±0.28 | 0.097 | 0.55±0.38 | 0.817 | 0.508 |
| 3 months | 0.30±0.24 | 0.713 | 0.59±0.56 | 0.924 | 0.48±0.24 | 0.089 | 0.59±0.35 | 0.937 | 0.691 |
| 6 months | 0.28±0.24 | 0.533 | 0.55±0.53 | 0.718 | 0.52±0.36 | 0.218 | 0.67±0.45 | 0.556 | 0.649 |
| CMT (μm) | |||||||||
| Baseline | 274.14±16.95 | 374.94±62.03 | 416.80±38.00 | 378.00±53.62 | 0.058 | ||||
| 1 month | 287.54±47.92 | 0.172 | 318.88±82.17 | 0.032 | 290.40±70.48 | 0.000 | 307.31±93.76 | 0.014 | 0.627 |
| 3 months | 296.79±79.10 | 0.149 | 304.00±65.09 | 0.003 | 275.40±93.24 | 0.000 | 297.00±113.86 | 0.018 | 0.668 |
| 6 months | 283.75±69.03 | 0.480 | 284.18±80.84 | 0.001 | 310.33±103.28 | 0.002 | 285.69±115.76 | 0.009 | 0.720 |
IVTA: intravitreal injection of triamcinolone acetonide; BCVA: best corrected visual acuity; CMT: central macular thickness
*Kruskal-Wallis test (p<0.05)
†Wilcoxon Matched-Pairs Signed-Ranks test (p<0.05)
: baseline - 1 month, baseline - 3 months, baseline - 6 months
Change in best corrected visual acuity (BCVA) in patients with baseline CMT between 250 to 300μm (Group 1).
Change in central macular thickness (CMT) in patients with baseline CMT between 250 to 300μm (Group 1).
Change in best corrected visual acuity (BCVA) in patients with baseline CMT between 300 to 500μm (Group 2).
Change in central macular thickness (CMT) in patients with baseline CMT between 300 to 500μm (Group 2).
Discussion
This study is, to our knowledge, the first report of the clinical course of the DME limited to mild to moderate degree.
Thickening of the retina at or within 500 μm of the center of the macular is classified as CSME in ETDRS and recommended to be treated with macular laser photocoagulation regardless of degree of macular edema. Focal laser photocoagulation reduced the risk of moderate visual loss by 50% in patients with CSME, while progressive visual loss occurs in up to 25% of patients despite laser treatment in other report [10]. One of the reasons of different reports of visual outcome might be due to various degrees of macular edema which were lumped together from 250 μm to 1000 μm. Since the diagnosis of CSME was made on the basis of slit lamp biomicroscopy and stereo fundus photography in ETDRS, it was subjective and relatively insensitive to subtle changes in retinal thickness. Therefore, CMT measured by OCT could be more sensitive and reproducible than conventional examination of ETDRS for diagnosing and monitoring the effect on the treatment response in DME.
Shahidi et al [11] reported that the level of foveal thickening before treatment strongly correlated with the degree of thickening after treatment and suggested quantitative retinal thickness measurement for assessing and monitoring macular edema. Estabrook et al [9] reported that patients with moderate macular thickening of 300 to 400 μm showed significant reduction in CMT with slight improvement in BCVA by laser treatment, while patient with mild macular edema of <300 μm showed statistically insignificant worsening of visual acuity with increased thickening, implying poor response to laser treatment. One limitation of this study was that there was no control group which had not received laser treatment.
In our study, eyes with CMT between 300 to 500 μm showed significant improvement of CMT which agreed with previous study. However it is interesting to note that significant improvement of CMT was revealed not only with laser treatment group but also with natural course group in our study. we assumed that general conditions such as the improvement in the blood glucose level might affect the decrease of DME [12,13]. The eyes with CMT between 250 to 300 μm showed statistically insignificant difference of visual acuity and CMT which is also agreed with previous report, though the eyes in our study had not received any specific treatment.
We assumed that the severe macular edema -over 500 μm for example- might have more edema beyond the potential of spontaneous resolution and have more risk of visual deterioration. This is why specific treatment for moderate macular edema such as laser treatment or IVTA is needed. On the contrary, mild macular edema -such as < 300 μm in our study- have less edema for reversal to normal and less risk for visual deterioration. The specific treatment for mild macular edema could be helpful but benefit may be limited and the potential complications associated with treatment are concerned. One study, which could support our assumption, has found that a retinal thickening in DME of 60% above normal value has a 50% probability for reversal of thickening with laser treatment, whereas thickening >130% has a <2.5% probability [11].
However, visual outcome did not seem to correlate with retinal thickness in our study. Even though all subgroups in group 2 showed significant reduction of CMT, no subgroup showed statistically significant improvement of BCVA. Diabetic Retinopathy Clinical Research Network (DRCR.Net) [14] reported that there was modest correlation between BCVA and OCT center point thickness, which suggested that OCT measurement alone might not be a good surrogate for visual acuity in DME. From this report and our study, it can be inferred that assessment of macular thickness is certainly clinically useful, but it is just one of several variables affecting visual acuity.
We assumed that the uncorrelation between BCVA and CMT might be caused by functional damage of photoreceptor, cataract, delayed-onset of macular ischemia and so on. Goebel et al [15] found similar moderate correlation between visual acuity and OCT in DME and found that correlation improved when excluding from analysis patients with macular nonperfusion and cataract.
The limitation of our study is retrospective in design, which has the possibility of selection bias. In addition to this, comparison of clinical course according to the treatment modalities could be limited by this sample size and 6 months follow-up. The reliability of statistical analysis could be decreased by its small sample size. 6 months follow-up is shorter than other studies such as ETDRS [3] and DRCR.net study [14] and could not secure its stability. Prospective study with larger numbers of subjects and long term follow-up period will be necessary.
In conclusion, the eye with mild DME between 250 to 300 μm did not show worsening of visual acuity or macular edema without any specific treatment. In moderate DME of between 300 to 500 μm, although IVTA seemed to be effective to decrease the macular edema at one month after the injection, there was no significant difference with laser treatment and natural course after 6 months. Therefore, close observation without specific treatment could be one of the options with the patients of mild or moderate DME who are contraindicated or reluctant to the treatments.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Bhagat N, Grigorian RA, Tutela A, Zarbin MA. Diabetic macular edema: pathogenesis and treatment. Surv Ophthalmol. 2009;54:1-32
2. Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. XV. The long-term incidence of macular edema. Ophthalmology. 1995;102:7-16
3. Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. ETDRS report number 1. Arch Ophthalmol. 1985;103:1796-806
4. Polito A, Shah SM, Haller JA, Zimmer-galler I, zeimer R, Campochiaro PA. et al. Comparison between retinal thickness analyzer and optical coherence tomography for assessment of foveal thickness in eyes with macular disease. Am J Ophthalmol. 2002;134:240-51
5. Chan A, Duker JS, Ko TH; Fujimoto JG, Schuman JS. Normal macular thickness measurements in healthy eyes using stratus optical coherence tomography. Arch Ophthalmol. 2006;124(2):193-198 doi:10.1001/archopht.124.2.193
6. Jonas JB, Kreissig I, Sofker A, Degenring R. Intravitreal injection of trimacinolone for diffuse diabetic macular edema. Arch Ophthalmol. 2003;121:57-61
7. Martidis A, Duker JS, Greenberg PB, Rogers AH, Puliafito CA, Reichel E. et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002;109:920-27
8. Massin P, Audren F, Haouchine B, Erginay A, Bergmann JF, Benosman R. et al. Intravitreal triamcinolone acetonide for diabetic diffuse macular edema: preliminary results of prospective controlled trial. Ophthalmology. 2004;111:218-24
9. Estabrook EJ, Madhusudhana KC, Hannan SR, Newsom RS. Can optical coherence tomography predict the outcome of laser photocoagulation for diabetic macular edema? Ophthalmic Sur Lasers Imaging. 2007;38:478-83
10. Early Treatment Diabetic Retinopathy Study Research Group. Effects of aspirin of treatment on diabetic retinopathy. ETDRS report number 8. Ophthalmology. 1991;98:757-65
11. Shahidi M, Ogura Y, Blair NP, Zeimer R. Retinal thickness change after focal laser treatment of diabetic macular edema. Br J Ophthlamol. 1994;78:827-30
12. Lobo CL, Bernardes RC, de Abreu JR, Cunha-Vaz JG. One-year follow-up of blood-retinal barrier and retinal thickness alteration in patients with type 2 diabetes mellitus and mild nonproliferative retinopathy. Arch Ophthalmol. 2001;119:1469-74
13. Kojima T, Terasaki H, Nomura H. et al. Vitrectomy for diabetic macular edema: effect of glycemic control(HbA1c), renal function(creatinine) and other local factors. Ophthalmic Res. 2003;35:192-8
14. Browning DJ, Gassman AR, Aiello LP, Beck RW, Broen DM, Fong DS. et al. Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007;114:525-36
15. Goebel W, Kretzchmar-Gross T. Retinal thickness in diabetic retinopathy: a study using optical coherence tomography (OCT). Retina. 2002;22:759-767
Author contact
![]() Corresponding author: In Won Park, M.D., Ph.D. Department of Ophthalmology Hallym University Sacred Heart Hospital, #896 Pyeongchon-dong, Anyang-city, Gyeonggi-do 431-070, Korea. Tel: 82-31-380-3835, Fax: 82-31-380-3837, E-mail: piw0930com.
Corresponding author: In Won Park, M.D., Ph.D. Department of Ophthalmology Hallym University Sacred Heart Hospital, #896 Pyeongchon-dong, Anyang-city, Gyeonggi-do 431-070, Korea. Tel: 82-31-380-3835, Fax: 82-31-380-3837, E-mail: piw0930com.

 Global reach, higher impact
Global reach, higher impact