3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2012; 9(1):14-19. doi:10.7150/ijms.9.14 This issue Cite
Research Paper
Comparison of Laparoscopic and Laparotomic Surgery for the Treatment of Peritoneal Inclusion Cyst
Department of Obstetrics and Gynecology, The Catholic University of Medicine, Korea
Received 2011-9-29; Accepted 2011-10-26; Published 2011-11-8
Abstract
Objectives: Peritoneal inclusion cyst (PIC) is defined as a fluid-filled mesothelial-lined cysts of the pelvis and it is most frequently encountered in women of reproductive age. The treatment options are observation, hormonal management, imaging-guided aspiration, image-guided sclerotherapy and surgical excision. The objective of this study is to compare between the laparoscopic and laparotomic surgery for the treatment of PIC.
Methods: Thirty-five patients with laparoscopy and forty-eight patients with laparotomy were included in the study. We compared the perioperative and postoperative data, the complications and the recurrence between the two groups.
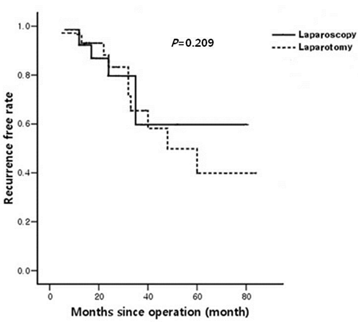
Results: There was a significantly reduced mean length of the hospital stay, estimated blood loss and complication rate in the laparoscopic group as compared to that of the laparotomic group (P=0.037, P=0.047 and P=0.037 respectively). There was also no statistical difference of recurrence rate between thelaparoscopic and laparotomic groups on the Cox proportional hazards model (p=0.209).
Conclusion: Our study showed that laparoscopy was superior to the laparotomy for the mean estimated blood loss, the mean length of the hospital stay and the complication rate except for the recurrence rate.
Keywords: Comparison, Laparoscopy. Peritoneal inclusion cyst
Introduction
Peritoneal inclusion cyst (PIC) is defined as an aggregate mass of variable sized, fluid-filled mesothelial-lined cysts of the pelvis, upper abdomen and retroperitoneum [1]. Mennemeyer and Smith were the first to describe peritoneal inclusion cyst in 1979 [2]. It is also known as “benign (multi) cystic peritoneal mesothliomas,” “inflammatory cysts of the peritoneum,” and “postoperative peritoneal cysts,” [1]. The pathogenesis is not well understood, yet they are thought to arise secondary to intra-abdominal inflammation and subsequent cyst formation with serous fluid derived from the ovarian stroma [3]. The most likely mechanism is that the small amount of follicular fluid extracted in the normal ovary in the ovulatory phase is mostly absorbed [4], but the injured peritoneum due to pelvic inflammatory disease or postoperative adhesion reduces the absorption capacity and the peritoneal fluid gradually accumulates [5]. It is thought that PIC is formed by the accumulation of unabsorbed follicular fluid secreted by the normal ovary in the adhered peritoneum, and the latter is caused by pelvic inflammation and injury [6]. The fact that the main peak incidence of PIC is the premenopausal women gives support that active ovarian tissue contributes the formation of PIC.
The treatment options are observation, hormonal management, imaging-guided aspiration, image-guided sclerotherapy and surgical excision [1, 7-10]. Although complete surgical resection is recommended by some authors [11,12], recurrence after surgical treatment has been reported in about half of the patients [1]. However, most studies have been case reports and small series, and there is a lack of long-term follow-up data. The surgical approach may be via laparotomy or laparoscopy [7,10].
The advantages of laparoscopic surgery include decreased postoperative pain, a short recovery period and improved cosmesis. However, the disadvantages include a longer operating time and the technical difficulty of laparoscopic procedures. Severe pelvic adhesion makes laparoscopic surgery difficult.
The objective of this study is to compare the laparoscopy with laparotomy for the treatment of PIC with respect to various demographic, perioperative and postoperative parameters.
Methods
The Institutional Review Board of the Catholic University approved this investigation.
We conducted a retrospective study involving patients who were operated on at the Saint Vincent Hospital, Catholic Medical College, during the period January 2003 - December 2009. We began performing laparosopic surgery since 2003. The patients' data was extracted from the available paper charts and computerized charts. The preoperative diagnosis was made by transvaginal ultrasonography, computer tomography (CT) or magnetic resonance imaging (MRI). All the patients underwent laparoscopic or laparotomic surgery for removal of the PIC. The bilaterality, location and size of cysts were described. The size of the cyst was defined as the mean diameter of the longitudinal and transverse dimensions and the height of the cyst. The outcome was assessed according to the operative time, the estimated blood loss, the serum CA-125 level, the number of septations of the cyst, the difference of hemoglobin between pre-operation and the one day post-operation, the length of hospital stay, the perioperative and postoperative complications, and recurrence of PIC. The operating time was defined as the time from entry into the operating room to the time of the delivering the patient to the postoperative anesthesia care unit.
For each patient, subsequent follow-up evaluations were performed by clinical assessment and an ultrasound examination in the outpatient clinic. The histories of previous abdominal and pelvic surgery were total hysterectomy, abdominal myomectomy, cesarean section, an operation on the ovary and fallopian tube, appendectomy and surgery of the small and large bowel. We categorized the follow-up results of the operation to complete remission, clinically successful and recurrence. Complete remission indicated total collapse of a PIC without associated symptoms. If a patient's symptoms improved and the mean diameter of the longitudinal and transverse dimensions of a cyst decreased by more than 50%, then the operation was considered as clinically successful. However, if the mean diameter of a cyst increased by over 50% the operation was considered as recurrence [13].
Statistical analysis was performed with SPSS (version 12.0; SPSS Inc., Chicago, IL, USA). All the data was described as means ± standard deviation (SD) or numbers (percentages). Continuous variables were compared with a 2-tailed t-test. Categorical variables were compared with Pearson's χ2 test. Recurrence was calculated from the date of diagnosis to the date of recurrence or the last follow-up. Cox proportional hazards model was used to calculate the recurrence rate. Differences in recurrence between two groups and other characteristics in terms of univariate analysis were assessed with the log-rank test. P values <0.05 were considered to be significant.
Procedure of the laparoscopy
The patients were recommended to have bowel preparation the day before their operation. The operation was done under general anesthesia with the patients in the Trendelenburg position. After disinfection and sterile coverage, we started with a small horizontal incision for placing the Veres needle. After insufflation of CO2 to a limited pressure of 12mHg, a 10 mm re-usable trocar was placed and the camera was inserted. However, when peritoneal adhesion was suspected by lifting the abdomen around the umbilicus, we tried the open method for entry of a 10 mm trocar [14]. The whole abdominal cavity, including the peritoneum, liver, gall bladder, stomach, spleen, appendix and bowels, was inspected for pathologies. Further two 5 mm trocars were placed laterally right and left. After placing the patient in a head-down position, the bowels were moved out of the pelvic and the inner genital organs were inspected. The peritoneum was incised over the cyst with scissors or monopolar cutting with low voltage. With the use of meticulous dissection close to the abdominal and pelvic structures, the delineated cyst wall was mobilized and resection was done. The cyst was placed into an Endobag (Sejong Corporation, Incheon, Korea), and the sac and cyst were extracted through the 10-mm port. The barrier agent Interceed (Ethicon Inc., Somerville, NJ, USA) was applied to the site of the former adhesion to prevent further adhesion. After deflating the intra-abdominal carbon dioxide gas, the laparoscopic ports were sutured. The specimen was taken to the pathologist for the histological diagnosis.
Procedure of the laparotomy
Laparotomy was done either through a horizontal incision above the symphysis or by vertical incision depending on the size of the cyst and the previous operative scar. The operation was done under general anesthesia with the patients in a supine position. Opening and inspection of the abdominal cavity, and pushing the bowels out of the pelvis were done. The procedure of cyst resection was same as that of the laparoscopic operation. The peritoneum was incised over the cyst with Mayo scissors or Metzenbaum. With the use of meticulous dissection close to abdominal structures, the delineated cyst wall was mobilized and resection was done. The barrier agent Interceed (Ethicon Inc., Somerville, NJ, USA) was applied to the site of the former adhesion to prevent further adhesion. After bleeding control, the abdominal wall was closed layer by layer.
Result
The demographic, perioperative and postoperative data are shown in Table 1 and 2. A laparoscopy was performed in 35 patients and a laparotomy was performed in 48 patients. Of the 35 patients, 4 underwent laparoscopic adhesiolysis of the PIC and 31 underwent laparoscopic complete resection of the PIC. Of the 48 patients in the laparotomic group, 11 underwent only adhesiolysis of the PIC, and 37 underwent complete resection of the PIC. One case in the laparoscopy was converted to laparotomy due to severe pelvic adhesion and excessive bleeding.
No significant difference was found in the mean age, parity, the mean number of previous abdominal operations, the type of operation, and the mean cyst diameter, the duration since the last operation and the serum CA 125 level between the two groups. In both group, the location of the PIC was mostly on the left side. There were a significantly shorter mean length of hospital stay, less estimated blood loss and a lesser difference between the preoperative and the one day postoperative hemoglobin level in the laparoscopic group compared to that of the laparotomic group (P=0.037, P=0.047 and P=0.040, respectively). The mean operative time was lower in the laparoscopic group than that of the laparotomic group, but there was no statistical significance (P=0.053).
Distribution of patient's characteristics and demographic data
| Laparoscopy (N=35) | Laparotomy (N=48) | P value | |
|---|---|---|---|
| Mean age (years) | 43.0 ± 11.0 | 44.9 ± 6.5 | 0.281 |
| Mean parity | 1.6 ± 1.0 | 1.7 ± 1.0 | 0.606 |
| Mean number of previous abdominal operation | 1.7 ± 1.0 | 1.7 ± 0.8 | 0.947 |
| Duration since last operation (years) | 7.1 ± 7.0 | 6.1 ± 4.7 | 0.463 |
| Title of operation | 0.251 | ||
| Adhesiolysis | 4 | 11 | |
| Cyst resection | 31 | 37 | |
| Mean cyst diameter (cm) | 8.8 ± 3.4 | 9.9 ± 3.1 | 0.139 |
| CA 125 | 20.0 ± 21.9 | 18.2 ± 37.3 | 0.823 |
| Location of cyst (%) | 0.347 | ||
| Left | 22 | 36 | |
| Right | 9 | 10 | |
| Both | 4 | 2 | |
| Number of septations in cyst | 0.214 | ||
| 0 | 20 | 19 | |
| 1 | 7 | 17 | |
| ≥ 2 | 8 | 12 | |
| Concurrent disease (%) | |||
| Endometriosis | 7 | 10 | 0.575 |
| PID | 5 | 2 | 0.126 |
Comparison between laparoscopy and laparotomy for perioperative and postoperative data
| Laparoscopy | Laparotomy | P value | |
|---|---|---|---|
| Mean operative time (min) | 112.9 ± 32.3 | 130.5 ± 45.2 | 0.053 |
| Mean estimated blood loss (mL) | 158.6 ± 135.3 | 218.3 ± 130.3 | 0.047 |
| The mean difference of hemoglobin (preoperative day - Postoperative day 1) | 1.1 ± 0.8 | 1.4 ± 0.8 | 0.040 |
| Mean length of hospital stay (days) | 5.1 ± 2.6 | 6.8 ± 4.2 | 0.037 |
The intraoperative, short-term and long-term complications are listed in Table 3. The total complication rate was lower in the laparoscopic group than that in the laparotomic group (P=0.037). In the laparoscopic group, two patients had postoperative ileus. They received conservative care without further procedures. In the laparotomic group, 4 cases of wound problems including 2 case of wound seroma, 1 case of wound disruption, and 1 case of ventral hernia, 2 cases of postoperative ileus and 2 cases of perioperative transfusion. One case was a bladder injury and the other was small bowel injury. Of the 4 patients with wound problem, 2 underwent wound revision and hernia repair. Conservative care and intravenous antibiotics therapy were done for the 2 cases of postoperative ileus. Both the intrapoerative bladder injury and small bowel injury were detected intraoperatively and primary repair was then done.
Five cases recurred in the laparoscopic group and 10 cases recurred in the laparotomic group (Table 4). Of the 5 cases in laparoscopic group, 2 cases underwent ultrasonography-guided aspiration and 3 cases underwent repeat laparoscopic cyst resection without further recurrence. One case had underlying pelvic endometriosis (stage IV). Two cases had an operation for performing adhesiolysis. Of the 10 recurred cases in laparotomic group, 2 cases underwent ultrasonography-guided aspiration and 1 case underwent laparoscopic cyst resection without further recurrence. Two cases had underlying pelvic endometriosis (stage IV) and 1 case had underlying pelvic inflammatory disease. Three cases had the operation for performing adhesiolysis. For comparing the recurrence rate, we performed a univariate analysis to determine the impact of age, the mean number of previous abdominal operations, the type of operation, the number of septations in the cyst and concurrent disease on recurrence. The type of operation had significant correlation with recurrence (P=0.030). There was no statistical difference of the recurrence rate between two groups on the Cox proportional hazards model (P=0.209; Fig.1).
Recurrence according to the Cox model.
Comparison between laparoscopy and laparotomy for complications
| Laparoscopy | Laparotomy | P value | |
|---|---|---|---|
| Total | 3 | 11 | 0.037 |
| Wound problem | 0 | 4 | |
| Seroma | 0 | 2 | |
| Wound disruption | 0 | 1 | |
| Ventral hernia | 0 | 1 | |
| Bladder injury | 0 | 1 | |
| Small bowel injury | 0 | 1 | |
| Transfusion | 1 | 2 | |
| Ileus | 2 | 3 |
Comparison between laparoscopy and laparotomy for recurrences
| Laparoscopy | Laparotomy | |
|---|---|---|
| Recurrence (%) | ||
| Complete remission | 28 (80.0%) | 35 (72.9%) |
| Clinically successful | 2 (5.7%) | 3 (6.3%) |
| Recurrence | 5 (14.3%) | 10 (20.8%) |
| Title of operation | ||
| Aspiration | 2 (50%) | 3 (27.2%) |
| Cyst resection | 3 (9.7%) | 7 (18.9%) |
Discussion
PIC is a rare tumor of an unknown origin, and it is most frequently encountered in women of reproductive age. Arguments for a pure reactive process versus a neoplastic spectrum continue to arise. Some investigators have mentioned that PIC may form as a result of a localized peritoneal fluid collection due to the presence of peritoneal adhesions, and these peritoneal adhesions have a relation to previous pelvic surgery, endometriosis or pelvic inflammatory disease. However, others have said that a PIC has a neoplastic etiology according to its recurrence, as well as according to the gross tumor-like appearance of these lesions [11].
The current literature is mostly based on case reports and small series and a uniform treatment approach and long-term follow-up data are lack. There are various treatment options for PIC, ranging from observation to complete resection. Observation with serial imaging is a feasible management option for asymptomatic patients with an incidentally discovered PIC [15]. Image-guided aspiration provides fluid for cytologic evaluation and it can lead to resolution of symptoms with minimal intervention and few complications. However, conservative management of a cystic lesion has not been effective and a tissue sample is required for making the histologic diagnosis and a biopsy is recommended if there is any suspicion of malignancy [16]. Birch et al. reported that approximately 50% of cysts recur after aspiration, and aspiration may provide temporary relief of symptoms but not a histologic diagnosis [10]. Sclerotherapy using of an intracystic catheter to instill either ethalol or povidone-iodine is a less invasive method and it has been used for the treatment of cysts in the abdominal organs and for treating postoperative lymphoceles [9,17]. Lim et al. reported that 30 cases of aspiration and sclerotherapy under ultrasonography and/or fluoroscopy guidance with absolute ethanol or 10% povidone-iodine showed a 90% of success rate and there was complete resolution [18]. However, studies with the long-term data, follow-up and complication rate of sclerotherapy are lack. Complications of sclerotherapy may occur such as viscus perforation, infection, bleeding, or the spillage of cystic fluid and/or sclerosant into the peritoneal cavity. Long-term data regarding the procedural complications or effects of sclerotherapy are also not available [9,13]. Although not a PIC, Takayasu et al. reported a case of a hepatic benign cyst that developed into adenocarcinoma after sclerotherapy with ethanol [19].
The recommended treatment is complete resection and the importance of surgery for making the diagnosis and treatment is supported by most authors [10,12]. The advantage of surgical management is that a definitive diagnosis is possible by obtaining a histologic specimen. The surgical management options vary from conservative adhesiolysis to radical excision. Definitive treatment is defined as complete resection of the entire macroscopically visible cyst wall. The surgical approach may be via laparoscopy or laparotomy. Recently, there are a few reports on successful laparoscopic resection of PIC. Porpora et al. reported that successful laparoscopic removal of a well-differentiated papillary mesothlioma of the peritoneum in a 46-year-old woman [20]. Nezhat et al. reported successful treatments of 3 cases of peritoneal mesothlioma associated with pelvic endometriosis [21].
PIC is associated with severe adhesion to the adjacent visceral organ and peritoneal wall. For resection of PIC, abdominal and pelvic adhesiolysis are necessary. Adhesiolysis by laparoscopy and laparotomy can be very time-consuming and technically difficult and it is best performed by an expert surgeon. However, laparoscopy has some advantages compared to laparotomy in our experience. First, despite lengthy laparoscopy, most patients are discharged earlier than when undergoing a laparotomy, they experience minimal complications and they return to full activity within one and two weeks of surgery [22]. Second, in laparoscopy, the port wound and the wound at the target of dissection are far away from each other, so the chances of adhesion to the peritoneum are less because for adhesion, both layers, which tend to adhere to each other, should be in contact [23]. Third, in laparoscopy there is less chance of drying of tissue because the inside environment is cut off from the outside. Fourth, the excellent visualization and magnification of laparoscopy allowed better access and exposure for further adhesiolysis [22].
Our study showed that laparoscopy was superior to laparotomy for the mean estimated blood loss, the mean difference of hemoglobin, the mean length of hospital stay, and the complication rate. However, there is no significant statistical difference for the recurrence rate of PIC between two groups.
Our study had several limitations. First, the surgical procedure was performed by several gynecologists with different levels of experience, and the participation of multiple operators may have affected the results. Second, there were wide differences in the follow-up period after surgery. We preferred laparoscopy for the direct inspection of pathology and to make the differential diagnosis of malignancy. A comparative study between laparoscopy and sclerotherapy as a minimal invasive technique may be necessary.
However, our study is the first study that has compared laparoscopy with laparotomy for the treatment of PIC, and we showed that the laparoscopy is superior to the laparotomy. Laparoscopy by well-skilled surgeons may decrease the mean operative time, the rate of conversion to laparotomy and the surgical complication.
In conclusion, laparoscopic surgery is a safe, effective and reliable method for the treatments of PIC. Laparoscopic surgery may reduce the perioperative and postoperative complications and hasten the recovery and return to routine activity. However, for the evaluation of recurrence rate, it is necessary to perform a long-term, larger-scale study.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Ross MJ, Welch WR, Scully RE. Multilocular peritoneal inclusion cysts (so-called cystic mesotheliomas). Cancer. 1989;64:1336-46
2. Mennemeyer R, Smith M. Multicystic, peritoneal mesothelioma: a report with electron microscopy of a case mimicking intra-abdominal cystic hygroma (lymphangioma). Cancer. 1979;44:692-8
3. Hoffer FA, Kozakewich H, Colodny A. et al. Peritoneal inclusion cysts: ovarian fluid in peritoneal adhesions. Radiology. 1988;169:189-91
4. Koninckx PR, Renaer M, Brosens IA. Origin of peritoneal fluid in women: an ovarian exudation product. Br J Obstet Gynaecol. 1980;87:177-83
5. Verger C, Luger A, Moore HL. et al. Acute changes in peritoneal morphology and transport properties with infectious peritonitis and mechanical injury. Kidney Int. 1983;23:823-31
6. Sohaey R, Gardner TL, Woodward PJ. et al. Sonographic diagnosis of peritoneal inclusion cysts. J Ultrasound Med. 1995;14:913-7
7. Letterie GS, Yon JL. Use of a long-acting GnRH agonist for benign cystic mesothelioma. Obstet Gynecol. 1995;85:901-3
8. Inman DS, Lambert AW, Wilkins DC. Multicystic peritoneal inclusion cysts: the use of CT guided drainage for symptom control. Ann R Coll Surg Engl. 2000;82:196-7
9. Lipitz S, Seidman DS, Schiff E. et al. Treatment of pelvic peritoneal cysts by drainage and ethanol instillation. Obstet Gynecol. 1995;86:297-9
10. Birch DW, Park A, Chen V. Laparoscopic resection of an intra-abdominal cystic mass: a cystic mesothelioma. Can J Surg. 1998;41:161-4
11. Sethna K, Mohamed F, Marchettini P. et al. Peritoneal cystic mesothelioma: a case series. Tumori. 2003;89:31-5
12. van Ruth S, Bronkhorst MW, van Coevorden F. et al. Peritoneal benign cystic mesothelioma: a case report and review of the literature. Eur J Surg Oncol. 2002;28:192-5
13. Jeong JY, Kim SH. Sclerotherapy of peritoneal inclusion cysts: preliminary results in seven patients. Korean J Radiol. 2001;2:164-70
14. Nuzzo G, Giuliante F, Tebala GD. et al. Routine use of open technique in laparoscopic operations. J Am Coll Surg. 1997;184:58-62
15. Tangjitgamol S, Erlichman J, Northrup H. et al. Benign multicystic peritoneal mesothelioma: cases reports in the family with diverticulosis and literature review. Int J Gynecol Cancer. 2005;15:1101-7
16. Soreide JA, Soreide K, Korner H. et al. Benign peritoneal cystic mesothelioma. World J Surg. 2006;30:560-6
17. Akhan O, Karcaaltincaba M, Ozmen MN. et al. Percutaneous transcatheter ethanol sclerotherapy and catheter drainage of postoperative pelvic lymphoceles. Cardiovasc Intervent Radiol. 2007;30:237-40
18. Lim HK, Cho JY, Kim SH. Sclerotherapy of peritoneal inclusion cysts: a long-term evaluation study. Abdom Imaging. 2010;35:431-6
19. Takayasu K, Mizuguchi Y, Muramatsu Y. et al. Late complication of a large simple cyst of the liver mimicking cystadenocarcinoma after sclerotherapy. AJR Am J Roentgenol. 2003;181:464-6
20. Porpora MG, Brancato V, D'Elia C. et al. Laparoscopic diagnosis and treatment of a well-differentiated papillary mesothelioma of the peritoneum. J Am Assoc Gynecol Laparosc. 2002;9:384-8
21. Nezhat FR, DeNoble SM, Brown DN. et al. Laparoscopic management of peritoneal mesothelioma associated with pelvic endometriosis. J Minim Invasive Gynecol. 2010;17:646-50
22. Chopra R, McVay C, Phillips E. et al. Laparoscopic lysis of adhesions. Am Surg. 2003;69:966-8
23. Gutt CN, Oniu T, Schemmer P. et al. Fewer adhesions induced by laparoscopic surgery? Surg Endosc. 2004;18:898-906
Author contact
![]() Corresponding author: Joo Hee Yoon, M.D., Ph.D., Department of Obstetrics and Gynecology, Seoul St. Mary's Hospital, Catholic University School of Medicine, 505, Banpo-dong, Seocho-gu, Seoul, Korea. E-mail: jhyoonac.kr, Phone: 82-2-2258-6177; Fax: 82-31-254-7481
Corresponding author: Joo Hee Yoon, M.D., Ph.D., Department of Obstetrics and Gynecology, Seoul St. Mary's Hospital, Catholic University School of Medicine, 505, Banpo-dong, Seocho-gu, Seoul, Korea. E-mail: jhyoonac.kr, Phone: 82-2-2258-6177; Fax: 82-31-254-7481

 Global reach, higher impact
Global reach, higher impact