3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2012; 9(1):11-13. doi:10.7150/ijms.9.11 This issue Cite
Case Report
Traumatic Hemorrhage within a Cerebellar Dermoid Cyst
1. Department of Neurosurgery, First Bethune Hospital of Jilin University, Changchun 130021, Jilin Province, P.R. China.
2. Department of Pathology, First Bethune Hospital of Jilin University, Changchun 130021, Jilin Province, P.R. China.
* Yongxin Luan, Haifeng Wang and Yanping Zhong contribute equally to this paper.
Received 2011-8-14; Accepted 2011-10-26; Published 2011-11-5
Abstract
Intracranial dermoid cysts with hemorrhage are fairly rare. Herein, we reported a 28-year-old female patient with a cerebellar dermoid cyst, which was found accidently on neuro-imaging after head trauma. MR scanning revealed that the lesion was located within the cerebellar vermis and was measured 3.5cm×3.9cm×3.0cm, with hyper-intensity on T1WI and hypo-intensity on T2WI. However, on CT imaging, it showed hyper-dense signals. It was removed completely via midline sub-occipital approach under surgical microscope. Histological examination proved it was a dermoid cyst with internal hemorrhage. In combination with literature review, we discussed the factors that might be responsible for the hemorrhage within dermoid cysts.
Keywords: Dermoid cyst, Hemorrhage, CT, MRI, Head trauma
Introduction
Dermoid cysts are rare congenital benign lesions originating from ectopic inclusion of epithelial cells during the neural tube closure in the third to fifth week of embryonic development. They accounts for approximately 1% of intracranial tumor-like lesions, with the highest incidence in the adults aged from 30 years to 40 years [1]. Although dermoid cyst rupture caused by trauma is not uncommon, it has never been reported that head trauma could lead to the hemorrhage within intracranial dermoid cyst. Herein, we report a case of intracranial dermoid cyst with internal hemorrhage resulting from head trauma.
Case report
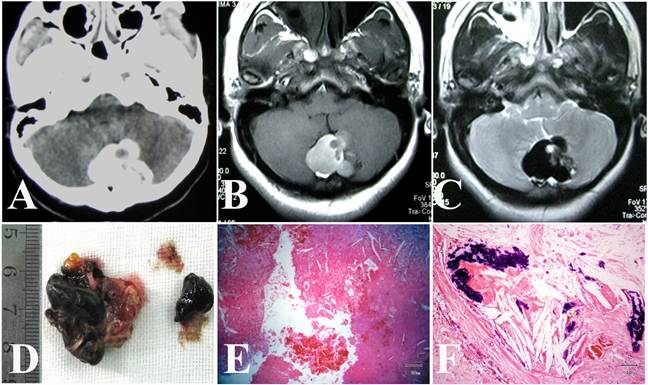
A 28-year-old female patient was emergently sent to a local hospital due to being hit by a falling object in the head. When the examinations with CT and MRI were finished, she was transferred to our hospital for further treatment 7 days later. On physical examination, neither neurological deficit nor midline cutaneous abnormalities were found. CT scanning revealed that a lobar hyperdense lesion with an internal irregular isodense area was located in the posterior fossa (Figure 1). On MR imaging, the lesion was hyper-intensive on T1WI and hypo-intensive on T2WI, located within the cerebellar vermis and measured 3.5cm×3.9cm×3.0cm (Figure 1).
No abnormalities were found preoperatively in the blood count, serum biochemistry, bleeding time, prothrombin time and partial thromboplastin time. She underwent craniotomy via midline suboccipital approach on the eighth day after the head trauma. During surgery, we found the lesion mimic a melanoma by its dark-brown appearance, but its capsule was partially calcified and lined interiorly with yellow fat. Its content consisted mainly of chocolate-like material, hair and old hematoma (Figure 1). Further exploration revealed a solid nodus at the internal side of the capsule, which was hard and in dark-red color. The lesion was resected completely under surgical microscope. The findings of histological examination included squamous epithelium, calcification, keratinous material, hairy substance, hemorrhage, and sheets or nests of hemosiderin-containing histiocytes, which were consistent with the histological features of dermoid cysts (Figure 1). Postoperatively, the patient recovered uneventfully and was discharged. At fellow-up of two and half years, she lived a normal life without any neurological deficits.
Discussion
Head trauma has been shown to be one of the factors leading to the rupture of intracranial dermoid cysts [2], but it has never been noted that head trauma is associated with the hemorrhage within intracranial dermoid cysts. However, for the dermoid cysts outside the cranium, hemorrhage following trauma was found to occur in two cases. One case was an ovarian dermoid cyst, which ruptured as the result of blunt trauma secondary to a motor vehicle collision and developed subsequently into severe hemorrhage in abdominal cavity [3]. The other case was an 85-year-old female who had an orbital dermoid cyst, within which interstitial hemorrhage was found at three months after her blunt head injury [4]. In our case, the head trauma did not cause rupture of the dermoid cyst, but leaded to internal hemorrhage proved subsequently by surgical findings and pathological examination.
Despite no cases of intracranial dermoid cysts has ever been reported to be with internal hemorrhage due to head trauma, by now, spontaneous hemorrhage had been found in four patients with intracranial dermoid cysts [5-7]. Although we do not know why hemorrhage would take place in dermoid cyst, we could refer to the mechanisms which were used for explaining the hemorrhage within brain tumors. In the case of brain tumors, pathological deficits in the walls of the tumoral blood vessels such as hyalinization, necrosis or degeneration are thought to be the main factors leading to the hemorrhage within tumors [8]. Considering three of the four cases with hemorrhagic dermoid cysts were over sixty years of age (Table 1), we speculate the degeneration of the blood vessel might be responsible for the intra-tumoral hemorrhage in elderly patients, despite no detailed description could be found in these reports.
A, CT scan revealed a hyperdense lesion containing irregular isodense area in the posterior fossa; The lesion presented hyper-intensity on T1WI (B), hypo-intensity on T2WI (C). D, macroscopic view of the removed lesion; E, interstitial hemorrhage within dermoid cyst; F, squamous epithelium, calcification, keratinous materials and cholesterol deposits. (Eematoxylin-Eosin staining, E, 20×; F, 40×.)
Summary of intracranial dermoid cysts with hemorrhage reported to date
| No. | Age /Sex | Cyst Location | CT scan | MRI scan | Reference |
|---|---|---|---|---|---|
| 1 | 61y/F | Sylvian fissure | Iso and hypodense | T1WI: hyper- and hypointense T2WI: hyperintense Enhancement: faintly peripheral enhancement | [5] |
| 2 | 63y/F | Parasellae | hyperdense | T1WI: hyperintense T2WI: hypointense | [6] |
| 3 | 73y/M | Posterior fossa | hyperdense | T1WI: hyperintense T2WI: N/A Enhancement: peripheral enhancement | [7] |
| 4 | 16y/M | Posterior fossa | hyperdense | T1WI: hyperintense T2WI: hypointense Enhacement: homogeneous enhancement | [9] |
| 5 | 28y/F | Posterior fossa | hyperdense | T1WI: hyperintense T2WI: hypointense FLAIRE: hypointense | This case |
Different with those three cases, the forth case was a 16-year-old boy [9]. His intracranial dermoid cyst enhanced homogeneously when contrast medium was used, which was very rare because dermoid cyst usually presented peripheral enhancement on contrast imaging. Thus, the boy case might indicate that hyper-vascularity might be another factor in association with hemorrhage within dermoid cysts. For our case, the patient is a young female at the age of 28, and no abnormalities were found preoperatively in the blood count, serum biochemistry, bleeding time, prothrombin time and partial thromboplastin time. Therefore, we think that head trauma is the inducer responsible for the hemorrhage within her dermoid cyst.
Compared with MR imaging, CT scanning is more sensitive to detect the internal hemorrhage within dermoid cyst, because no matter with or without internal hemorrhage, dermoid cysts usually present hyper-intensity on T1-weighted sequences, with variable signal on T2 weighted sequences ranging from hypo-intensity to heterogeneous hyper-intensity. On CT imaging, hemorrhagic dermoid cysts often show higher signal density than non-hemorrhagic dermoid cysts do. Of the four cases of hemorrhagic dermoid cysts mentioned above, three showed hyper-dense signals and one showed iso-dense signal. Therefore, CT is more contributive to make correct diagnosis for hemorrhagic dermoid cysts.
Conclusions
Our case showed that head trauma is a factor leading to the hemorrhage within dermoid cysts. CT is more sensitive to detect the bleeding within dermoid cysts than MRI. For the patient who had a history of head trauma, dermoid cyst with hemorrhage should be speculated under the condition that his intracranial lesion showed the typical features of dermoid cysts on MRI and hyper-dense signals on CT. To the best of our knowledge, this is the first case showing that hemorrhage within intracranial dermoid cyst is associated with head trauma.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Pant I, Joshi SC. Cerebellar intra-axial dermoid cyst: a case of unusual location. Childs Nerv Syst. 2008;24(1):157-159
2. Kim IY, Jung S, Jung TY, Kang SS, Kim TS. Traumatic rupture of an intracranial dermoid cyst. J Clin Neurosci. 2008;15(4):469-471
3. Levine RL, Pepe PE, Blackstone W, Danzinger J, Varon J. Occult traumatic avulsion of an ovarian dermoid cyst. Am J Emerg Med. 1992;10(4):344-346
4. Kudo K, Tsutsumi S, Suga Y, Okura H, Abe Y. et al. Orbital dermoid cyst with intratumoral inflammatory hemorrhage: case report. Neurol Med Chir (Tokyo). 2008;48(8):359-362
5. Chen JC, Chen Y, Lin SM, Tseng SH. Sylvian fissure dermoid cyst with intratumoral hemorrhage: case report. Clin Neurol Neurosurg. 2005;108(1):63-66
6. Mamata H, Matsumae M, Yanagimachi N, Matsuyama S, Takamiya Y. et al. Parasellar dermoid tumor with intra-tumoral hemorrhage. Eur Radiol. 1998;8(9):1594-1597
7. Neugroschl C, David P, Sadeghi N, Soebert A, Pirotte B. et al. Unusual CT features of dermoid cyst in the posterior fossa. Eur Radiol. 2002;12(11):2726-2729
8. Kondziolka D, Bernstein M, Resch L, Tator CH, Fleming JF. et al. Significance of hemorrhage into brain tumors: clinicopathological study. J Neurosurg. 1987;67(6):852-856
9. Sanchez-Mejia RO, Limbo M, Tihan T, Galvez MG, Woodward MV. et al. Intracranial dermoid cyst mimicking hemorrhage. Case report and review of the literature. J Neurosurg. 2006;105(4 Suppl):311-314
Author contact
![]() Corresponding author: Pengfei Ge, E-mail: pengfeigecom. Address: Department of Neurosurgery, 1st Bethune Hospital, Jilin University.71 xinmin Avenue, Changchun 130021, Jilin Province, P.R. China.
Corresponding author: Pengfei Ge, E-mail: pengfeigecom. Address: Department of Neurosurgery, 1st Bethune Hospital, Jilin University.71 xinmin Avenue, Changchun 130021, Jilin Province, P.R. China.

 Global reach, higher impact
Global reach, higher impact