3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2011; 8(8):717-724. doi:10.7150/ijms.8.717 This issue Cite
Research Paper
A Paired-Comparision of the MultiFunction CardioGramsm (MCG) and Sestamibi SPECT Myocardial Perfusion Imaging (MPI) to Quantitative Coronary Angiography for the Detection of Relevant Coronary Artery Obstruction (≥70%) - A Single-Center Study of 116 Consecutive Patients Referred for Coronary Angiography
1. Heart-Lung Center, Hawthorne, NJ, USA.
2. The Valley Hospital, Ridgewood, NJ, USA.
3. Columbia Presbyterian Medical Center, New York, NY, USA.
Received 2011-9-13; Accepted 2011-10-5; Published 2011-10-28
Abstract
Background: An analysis of the US National Cardiovascular Data Registry has revealed that only 38% of patients referred for coronary angiography after non-invasive coronary testing have relevant coronary obstruction (CO) (≥70%) of one or more coronary arteries.
Methods: A single-center trial was undertaken in 165 consecutive, symptomatic patients with either known or suspected coronary disease and/or valve disease(VHD) who agreed to undergo cardiac catheterization and coronary angiography if stress myocardial perfusion imaging was abnormal. A total of 116 patients with abnormal SPECT MPI tests, persistent chest pain, or significant VHD underwent final analysis. An MCG coronary obstruction (CO) score of ≥ 4.0 was considered indicative of relevant CO (≥70%) in one or more coronary arteries. Angiographic results were finalized by consensus of two angiographers.
Results: CO (≥70%) was present in 53 of 116 patients (46%). The MCG CO score was significantly higher for patients with relevant CO (5.4 ± 1.9 vs. 2.5 ± 1.9). The MCG correctly classified 103 of the 116 patients (89%) enrolled in the study as either having or not having CO (≥70%) (sensitivity- 91%; specificity- 87%; NPV- 92%; PPV- 86%). SPECT MPI was abnormal in 99 of the 116 (85%) patients undergoing catheterization, but correctly classified only 54 of the 116 patients (47%) entered in the study as either having or not having relevant CO (sensitivity-85%; specificity-14%; NPV - 53%; PPV- 45%).
Conclusions: The MCG was shown in this paired-comparison trial with SPECT MPI to safely and accurately identify patients with relevant CO (≥70%) prior to catheterization.
Keywords: Coronary Angiography, Coronary Artery Stenosis, MultiFunction CardioGram
Introduction
Coronary artery disease is the single leading cause of death in the US and the developed world [1]. However, recent data from an expanded analysis of the National Cardiovascular Data Registry in the US has revealed that only 38% of patients referred for coronary angiography, as a result of accepted methods of non-invasive coronary testing actually have relevant CO (≥70%) of one or more coronary arteries [2], strongly suggesting that current non-invasive testing does not accurately identify patients who should undergo coronary angiography.
The Multifunction Cardiogram™ (MCG) has been studied as an innovative computational electro-physiologic signal analysis tool for the non-invasive diagnosis of relevant CO/ischemia (≥70%) [6-10]. In three previous double-blind, controlled, clinical trials of patients scheduled to undergo elective coronary angiography [6-9] MCG accurately identified 88% of the patients finally found to either have or not have relevant CO (≥70%). Limitations of these studies included the lack of a standardized non-invasive diagnostic testing algorithm prior to angiography making it difficult to compare the predictive value of MCG to that of SPECT MPI or other non-invasive diagnostic testing modalities, and that the indications for angiography varied among patients. The purpose of this prospective, single-center, blinded trial was to address these limitations and further evaluate the accuracy of MCG testing by a paired-comparison to stress SPECT MPI in patients referred for coronary angiography because of an abnormal SPECT MPI test.
Materials and Methods
165 consecutive symptomatic patients with known or suspected coronary disease and/or valvular heart disease (VHD) who agreed to undergo MCG Testing, Stress SPECT MPI with sestamibi, resting TTE, and a coronary angiogram (CA) if stress SPECT MPI results showed evidence of ischemia, and/or if significant VHD was present, and/or if recurrent or persistent chest pain was present despite non-ischemic stress SPECT MPI were enrolled. The trial protocol was approved by the Valley Hospital Institutional Review Board. Stress MPI studies were all performed using standard SPECT techniques and VHD was defined using ASE guideline-based recommendations for severity assessment with TTE. Based on data from previously conducted trials [6-10], an MCG CO score of ≥ 4.0 was considered abnormal and indicative of the presence of relevant CO (≥70%) in one or more coronary arteries or bypass grafts. 49 patients with either normal or equivocal stress MPI results, and insignificant VHD, and no persistent chest pain were not recommended for CA, and, thus were excluded from analysis in the trial. These 49 patients have continued to undergo clinical surveillance since enrolled. 116 patients who underwent MCG testing and showed either abnormal stress MPI (stress defects with partial or complete reperfusion), and/or significant VHD on TTE , and/or recurrent chest pain despite a non-ischemic stress MPI (normal perfusion images or fixed defects with no reperfusion [ischemia]) were referred for CA, and included in the trial analysis. All myocardial perfusion data were acquired using ECG-gating and attenuation correction, and were analyzed visually and semi-quantitatively using Cedars Sinai Polar Map Analysis software with inclusion of perfusion, wall motion, and wall thickening data. Standard nuclear stress test interpretation criteria were used to define the presence/absence of abnormal myocardial perfusion. MCG final reports and stress MPI interpretations were completed prior to catheterization in all cases. Patients enrolled in the trial may or may not have had prior angiography and/or coronary intervention.
When the angiographic data was analyzed in patients with/without previous bypass grafting, the presence of ischemia was defined as CO ≥ 70% in native coronary vessels or bypass grafts affecting one or more of the major coronary distributions (LAD, LCX, and RCA) or ≥ 50% stenosis of the left main coronary artery. Angiographic results in all patients were evaluated quantitatively for relevant stenosis (≥ 70%) by consensus of two angiographers at the time of the catheterization. The second angiographer in all cases was an interventional cardiologist who was blinded to the MCG and SPECT MPI results. The personnel involved in obtaining the SPECT MPI data were blinded to the MCG, TTE, and cardiac catheterization data, and the personnel acquiring the MCG data were blinded to the SPECT MPI, the TTE, and catheterization data. Patients were blinded to their MCG score but not their TTE, MPI, or catheterization data.
The patients in this study were 35-84 years old, had known or suspected CAD with current coronary symptoms, had an intermediate pre-test risk of CAD by risk factor analysis, did not have an acute coronary syndrome, did not have a revascularization procedure or myocardial infarction within three months of entry, had no overlap with any previous MCG study or with the normalized MCG clinico-pathologic database of patients (see below). The MCG database and analysis software was not modified during the study period. Patient characteristics (name, date-of-birth, sex, height, weight), along with a minimum of three 82 second samples of resting two-lead (lead II and V5) ECG data, regardless of the ECG rhythm or morphology, were recorded on each patient entered and sent via the internet to the network center for objective analysis and reporting.
MCG Device and Database
The MCG device used in all patients in the study, is manufactured in the US by Premier Heart, LLC, Port Washington, NY, and records a simultaneous 2-lead resting ECG signal from leads II and V5 for 82 seconds, using proprietary hardware and software. The digitized MCG ECG data along with patient's name, date-of-birth, sex, height, and weight are encrypted (256-bit) by the device at the study location and securely transmitted over the Internet to a central server located in New York, NY for final analysis and reporting of the MCG CO score (0-20).
At the central server location in New York, a series of Discrete Fourier Transformations (DFT) and post-DFT signal averaging are performed on the data from the patient's two resting ECG leads followed by signal averaging. The final averaged digital data segment is then subjected to six mathematical transformations (auto and cross power spectra, coherence, phase angle shift, impulse response, cross correlation, transfer function, and an amplitude histogram) which generate a large inventory of empirically derived normalized mathematical indexes. The resulting mathematically integrated patterns of the abnormal indexes are then compared for degree of abnormality to the index patterns in the reference database to reach a final diagnostic output. The diagnostic output is represented as a combination of the overall disease severity score from 0 to 20 and an indicator of the presence of local or global ischemia, which together indicate the level of coronary obstruction/myocardial ischemia that is present in the study patient.
The database against which the incoming MCG data are compared originated from data gathering trials conducted from 1978 to 2000 in more than 30 institutions in Europe, Asia, and North America on ~100,000 individuals of varying ages and degrees of coronary disease including a normal population at each age [11]. The MCG database consists of ~10,000 validated normal patients and ~30,000 validated patients with varying degrees of severity of coronary disease. Ages range from 14 to 100 with an equal number of patients and 49% females in every age range in the database. All MCG data and analyses included in the database were performed using the same standardized and calibrated analog signal collection and processing equipment as in the current trial and were analyzed using the same software and hardware located at the central server location in New York. All MCG analyses in this database have been validated against the final medical and angiographic diagnoses, confirmed by two US independent academic angiographers having access to all the diagnostic tests including angiography results, lab, and cardiac enzyme test results. The MCG's current diagnostic capability for identification of local or global ischemia and the disease severity score used in this clinical study is based on this large proprietary database of validated MCG analyses accumulated since 1990. See Appendix in (7) for further details.
Statistical Methods
Descriptive statistics were calculated for all variables including confidence intervals. Differences between paired or two unpaired mean values were analyzed with the t-test, and degrees of freedom were adjusted according to a variance estimate if the F-test could not show equality of variances. Differences between more than two mean values were analyzed with the Scheffé test where homogeneity of variances was assessed with the Levene statistic. For two-way and multi-way tables, Fisher's exact test was used to calculate significance levels.
Odds ratios including 95% confidence intervals were calculated for all variables. Positive and negative predictive values (PPV, NPV) for the assessment of CO were calculated with adjustment to prevalence of stenosis [12]. To assess the performance of the prediction of stenosis independent of the prevalence of stenosis, the positive and negative likelihood ratios (LR) were calculated [13]. A value of p <0.05 was considered statistically significant. All analyses were done with SPSS for Windows Version 15 (SPSS Inc., Chicago, IL, USA).
Results
Final analysis was performed on 116 patients. No patients were excluded from the study because of poor quality MCG tracings or uninterpretable SPECT images. The 49 patients excluded from analysis significantly differed from the included patients with respect to age (61.7 +/- 13.1 vs. 67.3 +/- 11.3. years; p < 0.05) and sex (44.9% excluded females vs. 29.3% included females; p < 0.05). Only eight percent (8%) of patients (4/49) excluded had an abnormal MCG CO score ≥ 4 with evidence of moderate/severe local ischemia. These patients are being followed closely for major adverse coronary events.
Twenty of the 116 patients (17%) included in the study had previous coronary artery bypass grafting 12 or more weeks before inclusion in the study. Patients with previous coronary bypass grafting were significantly older (p <0.05) and more frequently male
Relevant CO was diagnosed by angiography in 53 of 116 patients (46%). There were no significant age differences between patients with and without angiographically proven relevant CO (p = 0.4). There were however significant gender differences with regard to the finding of relevant CO at angiography (29% female vs 52% male) (p <.02).
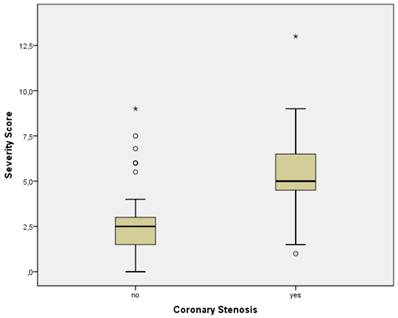
Patients without a significant CO had an MCG CO score < 4.0 (mean 2.5 ± 0.25 SEM) more frequently than those with a relevant CO (CO score ≥ 4.0) (mean 5.4 ± 0.26 SEM) by a wide margin (p <0.001) (Figure 1). The results indicate that MCG in this study had a sensitivity of 91% (0.79 - 0.97 CI) and a specificity of 87% (0.76 - 0.94 CI) for the prediction of CO. The positive predictive value (PPV) was 0.86 (0.74 - 0.94 CI), and the negative predictive value (NPV) was 0.92 (0.81 - 0.97 CI). (Table 1). SPECT Nuclear sensitivity in the study was 85% (0.72 - 0.93 CI), specificity was 14% (0.07 - 0.25 CI), PPV was 46% (0.35 - 0.56 CI), and NPV was 53% (0.28 - 0.77 CI) overall.
MCG CO Score vs. coronary stenosis (all patients). Boxplots of MCG CO scores in all patients with and without relevant coronary stenosis. The boundaries of the box are Tukey's hinges. The median is identified by the line inside the box. The length of the box is the interquartile range (IQR) computed from Tukey's hinges. Values more than three IQR's from the end of a box are labeled as extreme, denoted with an asterisk (*). Values more than 1.5 IQR's but less than 3 IQR's from the end of the box are labeled as outliers (•). Whiskers show high/low values. Outliers and Extremes were included in the overall statistical analysis because the assumptions about the distribution of the data (normal distribution) were not violated.
Composite Data
| Results | Disease | Test Results | a piori | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | TP | TN | FP | FN | Dis+ | Dis- | Test+ | Test- | Correct # | Correct % | Risk % | Sensitivity | Specificity | PPV | NPV | LR+ | LR- | |
| MCG vs. Cath | ||||||||||||||||||
| Total | 116 | 48 | 55 | 8 | 5 | 53 | 63 | 56 | 60 | 103 | 89% | 46% | 0.906 | 0.873 | 0.857 | 0.917 | 7.132 | 0.108 |
| female | 34 | 10 | 20 | 4 | 0 | 10 | 24 | 14 | 20 | 30 | 88% | 29% | 1.000 | 0.833 | 0.714 | 1.000 | 6.000 | 0.000 |
| male | 82 | 38 | 35 | 4 | 5 | 43 | 39 | 42 | 40 | 73 | 89% | 52% | 0.884 | 0.897 | 0.905 | 0.875 | 8.616 | 0.130 |
| < 65 yoa | 52 | 14 | 31 | 5 | 2 | 16 | 36 | 19 | 33 | 45 | 87% | 31% | 0.875 | 0.861 | 0.737 | 0.939 | 6.300 | 0.145 |
| 65+ yoa | 64 | 34 | 24 | 3 | 3 | 37 | 27 | 37 | 27 | 58 | 91% | 58% | 0.919 | 0.889 | 0.919 | 0.889 | 8.270 | 0.091 |
| no CABG | 96 | 37 | 48 | 8 | 3 | 40 | 56 | 45 | 51 | 85 | 89% | 42% | 0.925 | 0.857 | 0.822 | 0.941 | 6.475 | 0.088 |
| CABG | 20 | 11 | 7 | 0 | 2 | 13 | 7 | 11 | 9 | 18 | 90% | 65% | 0.846 | 1.000 | 1.000 | 0.778 | NaN | 0.154 |
| no diabetes | 99 | 38 | 49 | 8 | 4 | 42 | 57 | 46 | 53 | 87 | 88% | 42% | 0.905 | 0.860 | 0.826 | 0.925 | 6.446 | 0.111 |
| diabetes | 17 | 10 | 6 | 0 | 1 | 11 | 6 | 10 | 7 | 16 | 94% | 65% | 0.909 | 1.000 | 1.000 | 0.857 | NaN | 0.091 |
| no arterial hypertension | 29 | 12 | 12 | 3 | 2 | 14 | 15 | 15 | 14 | 24 | 83% | 48% | 0.857 | 0.800 | 0.800 | 0.857 | 4.286 | 0.179 |
| arterial hypertension | 87 | 36 | 43 | 5 | 3 | 39 | 48 | 41 | 46 | 79 | 91% | 45% | 0.923 | 0.896 | 0.878 | 0.935 | 8.862 | 0.086 |
| no anemia | 104 | 43 | 50 | 6 | 5 | 48 | 56 | 49 | 55 | 93 | 89% | 46% | 0.896 | 0.893 | 0.878 | 0.909 | 8.361 | 0.117 |
| anemia | 12 | 5 | 5 | 2 | 0 | 5 | 7 | 7 | 5 | 10 | 83% | 42% | 1.000 | 0.714 | 0.714 | 1.000 | 3.500 | 0.000 |
| no LV hypertrophy | 69 | 27 | 34 | 6 | 2 | 29 | 40 | 33 | 36 | 61 | 88% | 42% | 0.931 | 0.850 | 0.818 | 0.944 | 6.207 | 0.081 |
| LV hypertrophy | 47 | 21 | 21 | 2 | 3 | 24 | 23 | 23 | 24 | 42 | 89% | 51% | 0.875 | 0.913 | 0.913 | 0.875 | 10.06 | 0.137 |
| Nuclear vs. Cath | ||||||||||||||||||
| Total | 116 | 45 | 9 | 54 | 8 | 53 | 63 | 99 | 17 | 54 | 47% | 46% | 0.849 | 0.143 | 0.455 | 0.529 | 0.991 | 1.057 |
| female | 34 | 8 | 2 | 22 | 2 | 10 | 24 | 30 | 4 | 10 | 29% | 29% | 0.800 | 0.083 | 0.267 | 0.500 | 0.873 | 2.400 |
| male | 82 | 37 | 7 | 32 | 6 | 43 | 39 | 69 | 13 | 44 | 54% | 52% | 0.860 | 0.179 | 0.536 | 0.538 | 1.049 | 0.777 |
| < 65 yoa | 52 | 15 | 3 | 33 | 1 | 16 | 36 | 48 | 4 | 18 | 35% | 31% | 0.938 | 0.083 | 0.313 | 0.750 | 1.023 | 0.750 |
| 65+ yoa | 64 | 30 | 6 | 21 | 7 | 37 | 27 | 51 | 13 | 36 | 56% | 58% | 0.811 | 0.222 | 0.588 | 0.462 | 1.042 | 0.851 |
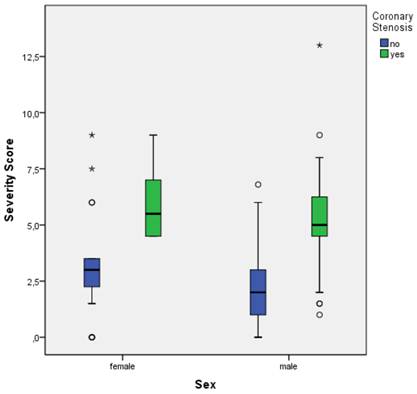
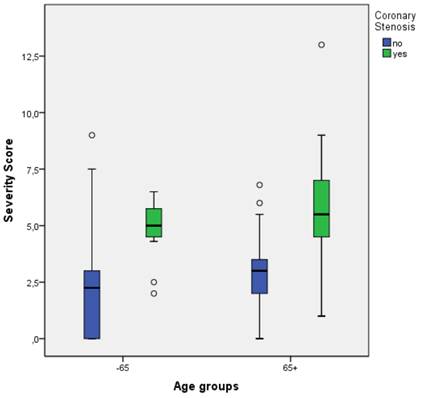
Figure 1, a boxplot of MCG CO scores versus the documented presence or absence of relevant CO by coronary angiography, demonstrates the clear separation of the mean and median MCG scores in the two groups (p < .01) of patients with and without relevant CO (≥70%). Figure 2 illustrates a boxplot of MCG CO scores from the gender subgroups showing that MCG was equally discriminatory between men and women at detecting the presence of relevant CO. In Figure 3, the MCG data from patients above and below the age of 65 in the study, demonstrated the ability of MCG to clearly separate those with and without relevant CO in the two age groups.
MCG Sensitivity averaged between 85% and 92% with only two exceptions (females and patients with anemia where sensitivity was 100%). MCG specificity also varied between subgroups from 83% to 91% with few exceptions such as the anemia subgroup (71%), patients with normal blood pressure (80%), patients with diabetes (100%), and patients with prior CABG (100%). In these subgroups, the number of patients was too low to achieve meaningful statistics.
However, MCG accurately classified 30/34 (88%) women as either having or not having relevant CO while SPECT MPI accurately classified 10/34 (29%) women as either having or not having relevant CO. For the female subgroup, MCG sensitivity was 100%, specificity 83%, and NPV was 100%, while SPECT sensitivity was 80%, specificity was 8%, and NPV was 50%. These differences were statistically significant with a p < 0.01.
For patients 65 years old or older the MCG sensitivity was 92%, the specificity was 89%, and the positive and negative predictive values were 92% and 89% respectively. The SPECT MPI sensitivity in patients over the age of 65 was 81% and the specificity was 22% with a positive and negative predictive value of 59% and 46% respectively. (Table 1.)
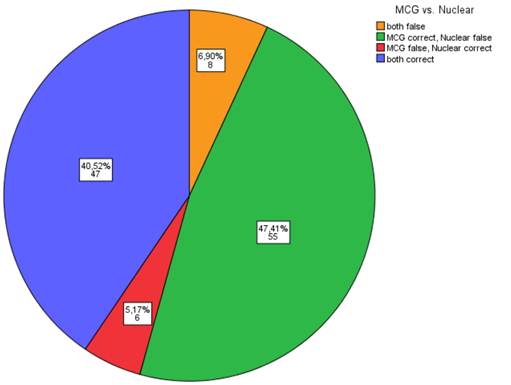
In paired-comparison, Table 2 shows that MCG and SPECT MPI testing were false indicators of relevant CO 6.9% of the time and were both correct indicators of the presence of relevant CO 40.5% of the time. However, MCG was the correct indicator CO and SPECT MPI was the incorrect indicator of CO 47.4% of the time, while MCG was the incorrect indicator of CO and SPECT MPI was the correct indicator of CO only 5.2% of the time.
MCG CO Score vs. coronary stenosis vs. sex. Boxplots of MCG CO scores in all patients with and without relevant coronary stenosis. (See Figure 1 Legend for further explanation of boxplots.)
MCG CO Score vs. coronary stenosis vs. age groups. Boxplots of MCG CO scores in all patients with/without relevant coronary obstruction. (See Figure 1 Legend for further explanation of boxplots.)
Correct Detection of CAD Defined by Angiographic Results: MCG Compared to SPECT Nuclear Testing (absolute numbers of patients and percentages).
Discussion
The overall diagnostic sensitivity of 91% and specificity of 85% of the MCG test documented in a meta-analysis [10] of the published MCG clinical trials had confirmed the diagnostic utility of this device to predict the presence of relevant CO (≥70%) in a population with a demonstrated intermediate pre-test risk of disease (27.7% to 43.4%). The current trial is a direct, paired-comparison of the accuracy of the MCG test and of SPECT MPI in predicting the existence of relevant CO (as determined by coronary angiography) in consecutive symptomatic patients undergoing typical sequential non-invasive evaluation for the presence of anatomically relevant CO. The study was not designed or powered to show superiority of one modality over another in the trial, but simply to assess the accuracy of each modality used in the same patient in predicting the presence or absence of anatomically relevant CO.
The study population had an overall CAD pretest probability of 46% (Intermediate Risk by Diamond-Forrester criteria [20]). The study only permitted patients with an abnormal SPECT MPI test, significant VHD with/without a normal SPECT MPI test, or patients with persistent coronary symptoms and a normal SPECT MPI test to undergo cardiac catheterization. While the MCG findings were consistent with the prior published data [6-10], SPECT MPI was associated with a high number of false positives (46%) that led to angiography in 54 patients whose management did not change based on the results, therefore, arguably making the angiogram medically unnecessary.
One limitation of the present study was that the anatomic obstructions were not explicitly quantified, in all patients, using a suitable scoring system such as the BARI (Bypass Angioplasty Revascularization Investigation) system [18] and there was no systematic functional analysis of lesion severity (induction of ischemia) using techniques of Fractional Flow Reserve. Regardless, the assessment of the anatomic coronary lesions in the present study was made by two experienced US based angiographers who independently visually evaluated the angiograms and agreed on the severity grading of obstructions. As the target criterion was an anatomic CO (≥70%), implying the need for an interventional treatment strategy, it is possible that borderline lesions were classified incorrectly as less severe (<70%). This may have further artificially reduced the calculated specificity of both the MCG and SPECT MPI methods.
Another limitation is the single-center enrollment of patients. Although this may limit the generalizability of the findings, the demographic distribution of this patient population matches those reported in the literature for symptomatic patients undergoing evaluation for CAD[2, 14-17, 19]. In addition, 54% of all the participants, 71% of women, and 42% of patients aged ≥ 65 did not have relevant CO on angiography, with MCG CO scores ranging from completely normal (0.0-0.5) to less than 4.0. This is similar to the findings of other studies, appearing to justify the study population's applicability to the general population of coronary disease patients in the US as described by Patel [2]. In the Patel study, less than half of the patients referred for catheterization due to abnormal stress imaging or CT angiographic data, were actually found to have anatomically severe CO (≥70%).
Finally, enrolling patients with valvular heart disease with symptoms suggestive of coronary insufficiency could have further reduced specificity of SPECT MPI due to documented examples of reduced coronary flow reserve in these patients. However, of the 8 patients with moderate to severe VHD enrolled in the study, three patients had abnormal SPECT MPI. Only 1 of these three patients with an abnormal SPECT MPI had no significant CO (i.e. < 70%), while 2 with an abnormal SPECT MPI had significant CO (≥70%) on catheterization demonstrating inclusion of these patients had little impact on overall study results.
In conclusion, the MCG device provides a highly sensitive and specific test for the detection of relevant CO, in a real world population of patients at low or intermediate pre-test risk of CO. The findings of this study strongly suggest that these patients will benefit from MCG testing when being considered for coronary angiography because an MCG CO score of < 4 indicates the patient can be safely managed medically without the need for invasive evaluation.
Acknowledgements
The authors wish to acknowledge the substantial contribution of Michael Imhoff, MD, PhD, Ruhr-University Bochum, Germany, to the statistical analysis of the data collected during the conduct of this trial. Also, the effort of Theresa Lairmore, certified nuclear technologist, in the acquisition and processing of all SPECT MPI data in this trial is greatly appreciated.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. OECD. OECD Health Data 2005: Statistics and Indicators for 30 Countries. Paris: OECD Publishing. 2005
2. Patel MR, Peterson ED, Dai D. et al. Low Diagnostic Yield of Elective Coronary Angiography. N Engl J Med. 2010;362:886-95
3. Gibbons RJ, Balady GJ, Beasley JW. et al. ACC/AHA Guidelines for Exercise Testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). J Am Coll Cardiol. 1997;30:260-311
4. Gibbons RJ, Balady GJ, Bricker JT. et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002;106:1883-1892
5. Gibbons RJ, Abrams J, Chatterjee K, et al.; American College of Cardiology; American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina). ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients with Chronic Stable Angina). J Am Coll Cardiol. 2003;41:159-168
6. Weiss MB, Narasimhadevara SM, Feng GQ, Shen JT. Computer-enhanced frequency-domain and 12-lead electrocardiography accurately detect abnormalities consistent with obstructive and nonobstructive coronary artery disease. Heart Dis. 2002;4:2-12
7. Grube E, Bootsveld A, Yuecel S. et al. Computerized two-lead resting ECG analysis for the detection of coronary artery stenosis. Int J Med Sci. 2007;7:249-263
8. Grube E, Bootsveld A, Buellesfeld L. et al. Computerized two-lead resting ECG analysis for the detection of coronary artery stenosis after coronary revascularization. Int J Med Sci. 2008;5(2):50-61
9. Hosokawa J, Shen JT, Imhoff M. Computerized 2-Lead Resting ECG Analysis for the Detection of Relevant Coronary ArteryStenosis in Comparison With Angiographic Findings. Congestive Heart Failure. 2008;14:251-260
10. Strobeck JE, Shen JT, Singh B. et al. Comparison of a Two-Lead, Computerized, Resting ECG Signal Analysis Device, the MultiFunction-CardioGramsm or MCG (a.k.a. 3DMP), to Quantitative Coronary Angiography for the Detection of Relevant Coronary Artery Stenosis (≥70%) - A Meta-Analysis of all Published Trials Performed and Analyzed in the US. Int J Med Sci. 2009;6(4):143-155
11. Feng G. EKG and EEG Multiphase Information Analysis (A collection of unpublished notes, thesis, papers and published articles from mid seventies to the late eighties translated into English from Chinese); First Edition. USA: American Medical Publishers. 1992
12. Altman DG, Bland JM. Diagnostic tests 2: Predictive values. BMJ. 1994;309:102
13. Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ. 2004;329:168-169
14. Tak T, Gutierrez R. Comparing stress testing methods. Available techniques and their use in CAD evaluation. Postgrad Med. 2004;115:61-70
15. Hecht HS, Shaw RE, Chin HL. et al. Silent ischemia after coronary angioplasty: evaluation of restenosis and extent of ischemia in asymptomatic patients by tomographic thallium-201 exercise imaging and comparison with symptomatic patients. J Am Coll Cardiol. 1991;17:670-677
16. Pirelli S, Danzi GB, Alberti A. et al. Comparison of usefulness of high-dose dipyridamole echocardiography and exercise electrocardiography for detection of asymptomatic restenosis after coronary angioplasty. Am J Cardiol. 1991;67:1335-1338
17. Schroeder E, Marchandise B, De Coster P. et al. Detection of restenosis after coronary angioplasty for single-vessel disease: how reliable are exercise electrocardiography and scintigraphy in asymptomatic patients? Eur Heart J. 1989;10(Suppl G):18-21
18. Alderman E, Stadius M. The angiographic definitions of the bypass angioplasty re-vascularization investigation. Coron Artery Dis. 1992;3:1189-1207
19. Scanlon PJ, Faxon DP, Audet AM. et al. ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation. 1999;99:2345-2357
20. Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary artery disease. New Engl J Med. 1979;300:1350-1358
Author contact
![]() Corresponding author: John E. Strobeck, MD, PhD, 297 Lafayette Avenue, Hawthorne, NJ 07506. 973-423-9388 Office.
Corresponding author: John E. Strobeck, MD, PhD, 297 Lafayette Avenue, Hawthorne, NJ 07506. 973-423-9388 Office.

 Global reach, higher impact
Global reach, higher impact