Impact Factor
ISSN: 1449-1907
Int J Med Sci 2010; 7(5):267-271. doi:10.7150/ijms.7.267 This issue Cite
Case Report
Treatment of oroantral fistula with autologous bone graft and application of a non-reabsorbable membrane
1. Department of Dental Sciences and Surgery, University of Bari “Aldo Moro”, Italy
2. Department of Dental Sciences, University of Rome “La Sapienza”, Italy
Received 2010-6-23; Accepted 2010-8-9; Published 2010-8-11
Abstract
Aim: The aim of the current report is to illustrate an alternative technique for the treatment of oroantral fistula (OAF), using an autologous bone graft integrated by xenologous particulate bone graft.
Background: Acute and chronic oroantral communications (OAC, OAF) can occur as a result of inadequate treatment. In fact surgical procedures into the maxillary posterior area can lead to inadvertent communication with the maxillary sinus. Spontaneous healing can occur in defects smaller than 3 mm while larger communications should be treated without delay, in order to avoid sinusitis. The most used techniques for the treatment of OAF involve buccal flap, palatal rotation - advancement flap, Bichat fat pad. All these surgical procedures are connected with a significant risk of morbidity of the donor site, infections, avascular flap necrosis, impossibility to repeat the surgical technique after clinical failure, and patient discomfort.
Case presentation: We report a 65-years-old female patient who came to our attention for the presence of an OAF and was treated using an autologous bone graft integrated by xenologous particulate bone graft. An expanded polytetrafluoroethylene titanium-reinforced membrane (Gore-Tex ®) was used in order to obtain an optimal reconstruction of soft tissues and to assure the preservation of the bone graft from epithelial connection.
Conclusions: This surgical procedure showed a good stability of the bone grafts, with a complete resolution of the OAF, optimal management of complications, including patient discomfort, and good regeneration of soft tissues.
Clinical significance: The principal advantage of the use of autologous bone graft with an expanded polytetrafluoroethylene titanium-reinforced membrane (Gore-Tex ®) to guide the bone regeneration is that it assures a predictable healing and allows a possible following implant-prosthetic rehabilitation.
Keywords: oroantral fistula, bone regeneration, maxillary sinus.
BACKGROUND
Oroantral communications (OAC) are rare complications in oral surgery, which recognize upper molars extraction as the most common etiologic factor (frequencies between 0.31% and 4.7% after the extraction of upper teeth1), followed by maxillary cysts, tumors, trauma, osteoradionecrosis, flap necrosis and dehiscence following implant failure in atrophied maxilla.
There is no agreement about the indication of techniques for the treatment of this kind of surgical complication. Spontaneous healing of 1 to 2 mm openings can occur, while untreated larger defects are connected with the pathogenesis of sinusitis (50% of patients after 48 hours - 90% of patients after 2 weeks2).
Therefore, management of communications between oral cavity and sinus after tooth extraction is recommended to promote closure within 24 hours1-3.
However, in patients with larger oroantral communications and those with a history of sinus disease, surgical closure is often indicated 1,2.
Oroantral fistula (OAF) is an epithelialized communication between the oral cavity and the maxillary sinus. The fistula is established for migration of the oral epithelium in the communication, event that happens when the perforation lasts from at least 48-72 hours. After some days, the fistula is organized more and more, preventing therefore the spontaneous closing of the perforation3 .
Many techniques have been described in order to prevent the consequences of a chronical presence of OAC, such as buccal flap, palatal rotation-advancement flap and buccal fat pad1,3-7.
The problems linked to these techniques are related to the morbidity of the donor site, discomfort for the patient, and no possibility to repeat the same technique after surgical failure.
The aim of the present case report is to analyze the healing of OAF with the associated use of an autologous bone graft, integrated by xenologous particulate bone graft, and a non- reabsorbable membrane.
CASE REPORT
We report a 65-years-old female patient who was referred to our attention for the presence of sporadic intraoral drainage in posterior left maxilla.
The discomfort was of a few years duration and had its origin following an endodontic treatment of tooth 2.6 provided four years before by her dentist.
The radiograph shows many characteristics of OAC/OAF; the apexes of tooth 26 were in extremely close approximation to the maxillary sinus, and an area of periapical rarefaction was evident (Fig. 1).
After the failure of the endodontic treatment the same tooth was subsequently extracted about five months later by the same practitioner for the persistence of symptomatology.
No pain occurred after the extraction, despite the drainage.
The patient was able to give consent after receiving oral and written information.
From the anamnesis, no systemic pathology came out.
Clinical examination of the area failed to disclose any significant pathologic.
Periodontally, there were no pockets, none of the remaining teeth were percussion positive, and the palpation was negative for loss of periodontal attach and abnormal movements.
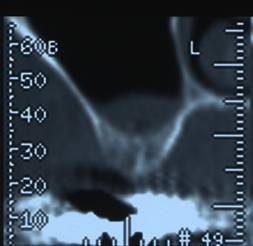
The radiographic (Fig.2) examination did not underline any discontinuity of the sinus floor, but showed radiographic loss of lamina dura at the inferior border of the maxillary sinus over the involved tooth and the localized swelling and thickening of the sinus mucosa; only close the root of 2.7 a periapical lesion was present; radiopacity of different degrees was evident in sinus space.
An explorative surgery was planned in order to evaluate the presence of a possible communication.
One hour before the surgical procedure an antibiotic prophilaxis was performed with amoxicillin and clavulanic acid 2 g.
The fixed partial prosthesis was removed and the contiguous mucosa appeared healthy.
A buccal full thickness flap was harvested and the presence of a small OAF was verified. (Fig.3).
After the evaluation of OAF dimensions (Fig. 4), the surgical procedure was conducted by performing an incision on the bone tissue surrounding the lesion with bone drills and by harvesting a squared wedge bone on the alveolar ridge, in order to avoid the persistence of fibrotic tissue and to permit an adequate bleeding.
An autologous bone graft was taken by a contiguous cortical site using a trephine with an inner diameter matching the size of the bony defect. (Fig. 5).
The graft was press-fit into the defect and a screw was inserted for internal fixation to increase stability (Fig. 6).
The remaining vertical bone defect was filled with a xenogenous bone graft (BIOSS®) (Fig 7), associated to an expanded polytetrafluoroethylene titanium-reinforced membrane (Gore-Tex ®).
A 3.0 silk detached suture was performed (Fig.8) and topic medication with povidone-iodine solution was applied. A systemic antibiotic prophylaxis with amoxicilline and clavulanic acid 1g was prescribed after 6 hours from surgery.
At 10 days from surgery the suture was removed and the mucosa appeared healthy.
At 45 days from surgery, after non-reabsorbable membrane removal (Fig. 9), the clinical control showed an uneventful healing process with complete elimination of the bone defect. (Fig. 10). No pain, fever or discomforts were described. The soft tissues appeared healthy, with normal color, consistence and no bleeding was present in the incision site and around the periodontal pockets of mesial and distal teeth.
The 6 months control showed a normal healing process. The radiographic evaluation with Computerized Tomography demonstrated a complete regeneration of the osseous sinus floor (Fig.11).
Rx after endodontic therapy of tooth 26.

Rx after 26 extraction and following rehabilitation with fixed partial prosthesis.

Flap elevation.

Demonstration of OAF existence by pin.

Autologous bone.

Graft stabilized with screw.

Defect filling with xenologous bone.

Sutured flap.

Non-reabsorbable membrane removal.

Clinical evidence of bone healing.

CT at 6 months.
DISCUSSION
Periapical periodontitis may result in maxillary sinusitis of dental origin with resultant inflammation and thickening of the mucosal lining of the sinus in areas adjacent to the involved teeth4 .
This inflammation may be a consequence of overinstrumentation and/or inadvertent injection or extrusion of irrigants, intracanal medicaments, sealers or solid obturation materials.
Furthermore, endodontic surgery performed on maxillary teeth may result in sinus perforation that develop into OAC4 , than into OAF.
Numerous surgical techniques introduced to close OAC and OAF include rotating or advancing local tissues such as the buccal or palatal mucosa, buccal fat pad, submucosal tissue, or tongue tissue6.
Most of them rely on mobilizing the tissue and advancing the resultant flap into the defect5.
The closure of OAF is a major problem considering the phlogistic consequences of sinus membrane infection, with the impossibility to perform implant rehabilitation and pre-implant surgical procedures. In addition, further implant surgery generally requires more reconstructed bone at the implantation site with a monocortical block. The final result is a vascularized new bone formation which eventually osseo-integrated with the surrounding bone.
Moreover, experimental studies confirm that autogeneous bone graft assure more predictable results than xenogenous graft, in term of osteo-integration on the receiving site, in order to obtain the closure of OAC, such as synthetic bone graft substitutes constitute a valid alternative to flap based techniques7-11.
The bone graft techniques for the treatment of moderate to large OAC or OAF demonstrate to be innovative, successful and predictable and permit to avoid the clinical collateral effects, like morbidity of the donor site, related to soft tissue flaps.
These techniques, similar to the one that we reported, were innovative and successful for treating moderate to large OAF.
CONCLUSIONS
OAF should be treated by establishing a physical barrier to prevent infection of the maxillary sinus.
The closure of the communications with autologous bone graft substitutes is a valid alternative to flap based techniques.
Because of the continued need for implant rehabilitation and the necessity of preimplant surgical procedures, such as sinus floor elevation, the routine soft tissue closure of OAF has become a major problem.
Therefore, a method that makes use of autogenous bone grafts harvested from the iliac crest for the closure of the defects has been used 12.
This method causes matting of the mucosae and Schneiderian membrane and makes elevation of the sinus membrane without disruption impossible 2.
Clinical Significance
The principal advantage of the technique described here is the use of autologous bone graft with an expanded polytetrafluoroethylene titanium-reinforced membrane (Gore-Tex ®) to guide the bone regeneration assures a predictable healing and the possibility of a following implant-prosthetic rehabilitation12.
Consent Statement
Written informed consent was obtained from the patients for publication of this study and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this Journal.
Competing interests
The authors declare that they have no competing interests.
References
1. Punwutikorn J, Waikakul A, Pairuchvej V. Clinically significant oroantral communications—a study of incidence and site. Int J Oral Maxillofac Surg. 1994;23:19-21
2. Haas R, Watzak G, Baron M, Tepper G, Mailath G, Watzek G. A preliminary study of monocortical bone grafts for oroantral fistula closure. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003Sep;96(3):263-6
3. Lee BK. One-stage operation of large oroantral fistula closure, sinus lifting, and autogenous bone grafting for dental implant installation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:707-13
4. Hauman CH, Chandler NP, Tong DC. Endodontic implications of the maxillary sinus: a review. Int Endod J. 2002Feb;35(2):127-141
5. Waldrop TC, Semba SE. Closure of oroantral communication using guided tissue regeneration and an absorbable gelatin membrane. J Periodontol. 1993Nov;64(11):1061-6
6. van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000Jun;11(3):256-65
7. Gacic B, Todorovic L, Kokovic V, Danilovic V, Stojcev-Stajcic L, Drazic R, Markovic A. The closure of oroantral communications with resorbable PLGA-coated beta-TCP root analogs, hemostatic gauze, or buccal flaps: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009Dec;108(6):844-50
8. Ngeow WC. The use of Bichat's buccal fat pad to close oroantral communications in irradiated maxilla. J Oral Maxillofac Surg. 2010Jan;68(1):229-30
9. Hernando J, Gallego L, Junquera L, Villarreal P. Oroantral communications. A retrospective analysis. Med Oral Patol Oral Cir Bucal. 2010May1;15(3):499-503
10. Visscher SH, van Minnen B, Bos RR. Closure of oroantral communications using biodegradable polyurethane foam: a feasibility study. J Oral Maxillofac Surg. 2010Feb;68(2):281-6
11. Ogunsalu CO, Rohrer M, Persad H, Archibald A, Watkins J, Daisley H, Ezeokoli C, Adogwa A, Legall C, Khan O. Single photon emission computerized tomography and histological evaluation in the validation of a new technique for closure of oro-antral communication: an experimental study in pigs. West Indian Med J. 2008Mar;57(2):166-72
12. Cortes D, Martinez-Conde R, Uribarri A, Eguia del Valle A, Lopez J, Aguirre JM. Simultaneous oral antral fistula closure and sinus floor augmentation to facilitate dental implant placement or orthodontics. J Oral Maxillofac Surg. 2010May;68(5):1148-51
Author contact
![]() Corresponding author: Dr. Andrea Ballini, Dept. of Dental Sciences and Surgery, Faculty of Medicine and Surgery, University of Bari “Aldo Moro”-Italy, P.zza G. Cesare n.11 -70124 Bari-Italy. E-mail: andrea.balliniuniba.it; Tel: (+39)0805594242; Fax: (+39)0805478043.
Corresponding author: Dr. Andrea Ballini, Dept. of Dental Sciences and Surgery, Faculty of Medicine and Surgery, University of Bari “Aldo Moro”-Italy, P.zza G. Cesare n.11 -70124 Bari-Italy. E-mail: andrea.balliniuniba.it; Tel: (+39)0805594242; Fax: (+39)0805478043.

 Global reach, higher impact
Global reach, higher impact