3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2010; 7(5):260-266. doi:10.7150/ijms.7.260 This issue Cite
Research Paper
Changes of uterine blood flow after vaginal radical trachelectomy (VRT) in patients with early-stage uterine invasive cervical cancer
1. Department of Obstetrics and Gynecology, Sapporo Medical University, Sapporo Hokkaido, Japan
2. Department of Radiology, Sapporo Medical University, Sapporo Hokkaido, Japan
Received 2010-6-2; Accepted 2010-8-4; Published 2010-8-5
Abstract
Background. Vaginal radical trachectomy (RT) ligates and cuts several arteries supplying the uterus. Changes of blood supply to the uterus in two patients who experienced pregnancy and delivery were studied by using 3-D CT scanning. Effects of changes of blood supply to the uterus on the pregnancy courses were also examined.
Methods. Vascular distribution in the uterus was studied in two patients who received vaginal RT after delivery. Effects of changes of vascular distribution after vaginal RT were studied with respect to pregnancy courses and cervical functions.
Results. New arterial vascularization from the ascending branches of uterine arteries or other arteries occurred, and these new vessels seemed to supply blood to the remaining cervix. Differences of fetal growth and histopathological changes in the placenta between the two patients could not be detected.
Conclusion. Ligation and cutting of several supplying arteries by RT induces new areterial vascularization and it does not seem to affect fetal growth and placental function.
Keywords: Radical trachelectomy, uterine cervical cancer, 3-D CT scanning
Introduction
Uterine cervical cancer is one of the most common cancers diagnosed in women of reproductive age. Thanks to the progress of the cervical cancer screening system, the mortality rate of patients with cervical cancer has decreased in Japan over the past twenty years1. However, the number of patients with early invasive cervical cancer during reproductive age is increasing. Not a few of them hope to preserve their fertility. Recently, radical trachelectomy (RT) with pelvic lymphadenctomy has become a valuable fertility-preserving treatment option for these patients in Japan2-4. We have already performed 20 vaginal RTs with laparoscopic lymphadenectomy, and have experienced five pregnancies and four deliveries so far. As we reported before, in pregnant patients who undergo this operation, premature labor and the following occurrence of preterm premature rupture of the membrane (pPROM) are thought to be the most troublesome pregnancy-related complications3. Various factors such as lack of a protective effect against vaginal infection or the lack of mechanical support of the residual cervix due to the dissection of the uterine cervix and the division of supplying arteries might induce such complications. On the basis of these complications, there might be reduced blood supply to the remaining uterus. Furthermore, if the blood supply to the uterus is reduced, it could be a cause of intrauterine growth retardation (IUGR) or intrauterine fetal death (IUFD)5.
In this report, we studied changes of the blood supply to the uterus in two patients who experienced pregnancy and delivery. Effects of these changes on the pregnancy courses are also discussed.
Patients and methods
In the period from January 2003 through December 2009, a total of 20 women with early-stage invasive uterine cancer underwent vaginal RT with lymphadenectomy in Sapporo Medical University Hospital. Among them, five patients became pregnant, and four of them delivered by cesarean section. In this study, we performed 3-D CT scanning for assessment of the blood supply to the uterus in two patients who had undergone vaginal RT with pelvic lymphadenectomy after delivery. 3-D CT scanning was also performed in a woman with normal uterus after the delivery for the assessment of an intra-abdominal disease, and her picture was used as a control. The clinical courses of pregnancy, fetal growth measured by ultrasonography, and results of histopathological examination of the placenta were also compared between the two patients. Characteristics of both patients are presented in Table 1. Patient 1 was a 35-year-old Japanese woman, gravida 0 para 0. As a pap smear at a local clinic showed atypical squamous cells corresponding to cervical intraepithelial neoplasia (CIN) 3, she was referred to our hospital. She received diagnostic laser conization, and she was diagnosed as having stage Ib1 squamous cell carcinoma. Then she underwent vaginal RT and laparoscopic lymphadenectomy, and she became pregnant six months after the operation by artificial intrauterine insemination. She was admitted to our hospital with a diagnosis of threatened abortion at 17 weeks of gestation. In spite of bed rest, disinfection therapy, and the administration of ritodrine, she suffered from pPROM at 23 weeks of gestation. Therefore she underwent emergent cesarean section at 24 weeks of gestation.
Patient 2 was a 28-year-old Japanese woman, gravida 0 para 0. She was diagnosed as having stage Ib1 cervical squamous cell carcinoma by diagnostic laser conization at a local hospital. She was referred to our hospital for fertility-sparing treatment. She also underwent vaginal RT and laparoscopic lymphadenectomy. At 14 months after the operation, she became pregnant without any artificial reproductive techniques. We recommended her to enter our hospital early in the second trimester in spite of no signs of threatened abortion. Daily vaginal disinfection with popidone iodine, bed rest, and administration of ritodrine and an ulinastatin vaginal suppository were continued as a new follow-up modality for pregnant patients who received RT. Finally, at 35 weeks of gestation, scheduled cesarean section was performed for her.
The postpartum courses of the patients were not remarkable, and no signs of recurrence have been seen for either patient up to now. Their menstrual cycles also restarted within 6 months postpartum.
Vaginal RT was performed using the laparoscopico-vaginal procedure of Dargent et al. Briefly, a rim of vaginal mucosa was delineated circumferentially and excised so that the anterior and posterior mucosae could cover the cervix. The vesicovaginal space was defined laterally on each side. After identification of the ureters, the bladder pillars were separated and sectioned. Then the proximal parametrium and the cervicovaginal branches of the uterine arteries were excised. After these procedures, the cervix was amputated approximately 10 mm below the isthmus, a nylon suture was placed around the cervix, and a Sturumdorf suture was placed to cover the surface of the cervix.
Clinical characteristics of patients.
| Patient 1 | Patient 2 | |
| age(years) and parity | 35 P0(0) | 28 P0(0) |
| histology and clinical stage | SCC stage Ib1 | SCC stage Ib1 |
| gestation at delivery | 24 weeks + 1 day | 34 weeks + 6 day |
| birth weight and Apgar score | 588g 1(1min.)/1(5min.) | 1862g 7(1min.)/8(5min.) |
| pathology of placenta | Ischemic change(-) CAM(+) | Ischemic change(-) CAM(-) |
| prognosis | NED 27 months | NED 54months |
P(0) means pregnancy0 and delivery0. SCC means squamous cell carcinoma.
CAM means chorioamnionitis. NED means “no evidence of disease”.
Results
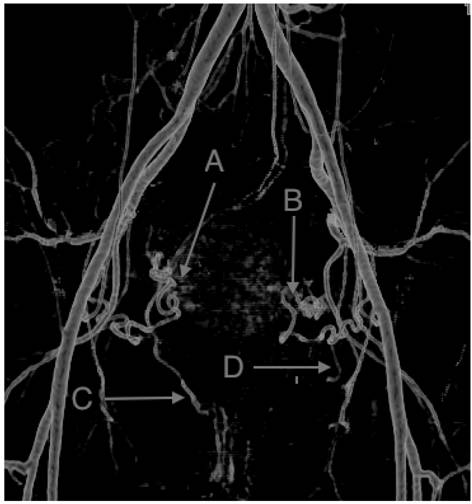
Figures 1 and 2 show the blood vessel distribution in the uterus for both patients. Figure 3 shows the blood distribution in the normal uterus after the delivery. Identification of blood vessels was performed by a radiologist (M.T).
3-D computed tomography (CT) imaging of patient 1. a: Left uterine artery. No descending branch was seen. b: New vessels probably arisen from ascending branch of left uterine artery. c: New vessels probably arisen from ascending branch of right uterine artery. d: Right uterine artery. No descending branch was seen. Identification of each vessel was made by a radiologist (M.T).

3-D CT imaging of patient 2. e: Left uterine artery. No descending branch was seen. f: New vessels probably arisen from ascending branch of left uterine artery and some arteries from vagina or pelvic wall . g: New vessels probably arisen from some arteries from vagina or pelvic wall. h: Right ovarian artery supplying blood to the remaining uterus. No right uterine artery could be detected. Main blood supply of the right side of the uterus was through “g” and “h”. Identification of each vessel was also made by a radiologist (M.T).

In vaginal RT, we usually amputate the cervix at the level of the uterine artery, which corresponds to approximately 10 mm below the isthmus. In this procedure, we usually ligate and cut the descending branches of the uterine arteries and vaginal arteries. These arteries mainly supply blood to the lower segment of the uterus. Fig. 1 and Fig. 2 show that the descending branches of uterine arteries and vaginal arteries could not be seen in either patient. New arterial vascularization from the ascending branches of uterine arteries arose, and these new vessels seemed to supply blood to the remaining cervix, including the neo-cervix. On the 3-D CT scan, no ischemic areas were seen in the remaining uterus.
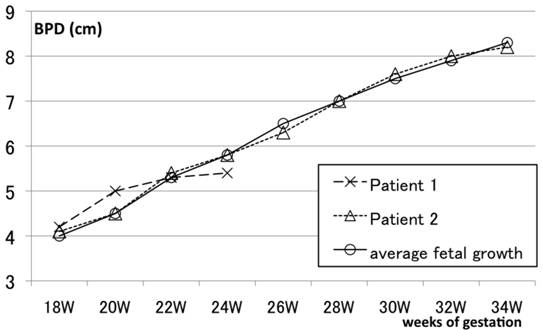
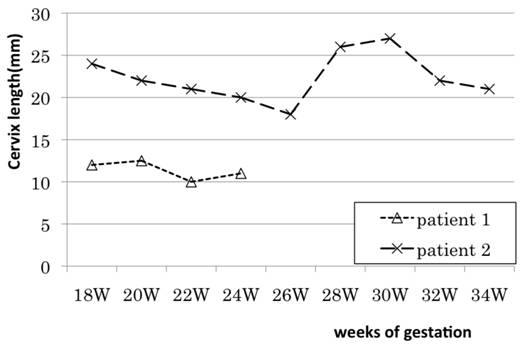
Fig. 3 shows the fetal growth of both patients. Patient 1 received emergent cesarean section at 24 weeks of gestation because of sudden premature rupture of the membrane. Therefore the birth weight of the child of patient 1 was 588g, though she survived thanks to the efforts of neonatologists and co-workers. Fetal growth up to the delivery was appropriate for gestational age for patient 1. Fetal growth of patient 2 was also within the normal range over the pregnancy period. Fig. 4 shows changes of cervical length as measured by transvaginal ultrasonography in the both patients. The remaining cervix of patient 1 was shorter than that of patient 2 over the pregnancy period.
Furthermore as shown in Table 1, the placenta from patient 1 showed the existence of severe chorioamionitis, which might have been a cause of pPROM; however, no ischemic changes of the placenta were detected histopathologically. The placenta of patient 2, who delivered at 35 weeks of gestation, did not show ischemic changes either.
3-D CT imaging of a patient with normal uterus after the delivery. A: Ascending branch of right uterine artery. B: Ascending branch of left uterine artery. C: Descending branch of right uterine artery. D: Descending branch of left uterine artery. Identification of each vessel was also made by a radiologist (M.T).
Ultrasonographic changes of BPD as a marker of fetal growth in patient 1 and patient 2. Fetal growth of each patient assessed by the changes of BPD (biparietal diameter) was within normal range over the pregnancy period, although patient 1 received emergent cesarean section at 24 weeks of gestation because of sudden premature rupture of the membrane.
Transvaginal ultrasonographic changes of cervical length during pregnancy after vaginal radical trachelectomy(RT). The remaining cervix of patient 1 was shorter than that of patient 2 over the pregnancy period.
Discussion
In this study, we looked at changes of blood supply to the uterus after vaginal RT in two patients who experienced pregnancy. The effects of blood supply on the fetal growth and the placental changes were also studied. RT removes the cervix of the uterus, parametrium, and upper vagina through a vaginal approach and is designed to preserve childbearing potential in young patients with cervical cancer. This procedure requires ligation and cutting the descending branches of uterine arteries as well as the division of vaginal arteries. The uterus has six main supplying arteries: two ovarian, two uterine, and two vaginal arteries. It is said that four of the six arteries are required to ensure uterine viability5. However, almost half of the supplying arteries are cut after vaginal RT. Sieunarine et al. reported that the blood flow reduction after ovarian artery ligation was more pronounced than after uterine artery ligation in rats, which means that the ovarian artery might be the major contributor of blood flow to the uterus. In this study, 3D CT scans also showed sufficient blood flow to the uterine body through both ovarian arteries, the remaining ascending branches of uterine arteries, and a new network of vessels. No difference between the patients could be detected for the blood flow distribution.
Are these networks of new vessels sufficient for the maintenance of pregnancy? A decrease of blood supply to the uterus can cause abortion or intrauterine growth retardation (IUGR) of the fetus 6. In these conditions, several pathological changes of the placenta can be seen. Ischemic changes of the placenta include an increase of avascular villi, syncytial knots, and an immature syncytial sprout, or increased lesions of placental infarction6,7. Furthermore, as we reported before, molecular biological changes such as increased expression of apoptosis-related genes are also seen8. However, the placentas of the both patients in this study showed no such ischemic changes. Furthermore, fetal growth of both patients up to delivery was within the normal range. These results suggest that division of the descending branches of uterine arteries and vaginal arteries does not seem to affect fetal growth.
Does division of descending branches of uterine arteries and vaginal arteries affect the function of the neo-cervix?
Lack of mechanical support of the residual cervix, ascending infection and chorioamnonitis, caused by disruption of the endocervical glands and reduced secretion of mucus, have been thought be causes of pPROM. As we have shown in this study, the remaining cervix of patient 1 after vaginal RT was found to be shorter than that of patient 2 by transvaginal ultrasonographic assessment over the pregnancy period. Although patient 1 suffered from pPROM at 23 weeks of gestation, the blood supply to the lower segment of the uterus did not show any differences between the two patients. For this patient, the cause of pPROM might have been chorioamnionitis caused by the reasons described above.
RT now has become an acceptable treatment modality in patients with early invasive uterine cancer who hope for preservation of fertility. However, vaginal RT is completely different from laser conization from the point of view of targeting lesions and postoperative invasiveness.
Although more than 300 pregnancies have been reported since Dargent reported his first series of radical trachelectomies in 1994 9,10,11, there are still few reports on pregnancy complications after RT. It is known that lack of a protective effect against vaginal infection or the lack of mechanical support of the residual cervix due to the dissection of the uterine cervix might be a cause of pPROM, and the following occurrence of preterm premature delivery. Furthermore, as Martin et al. reported, in patients with high risk of recurrence, adjuvant therapies such as radiation therapy or chemotherapy might be necessary after RT. Those therapies could also affect the fertility and the pregnancy course of the patient. However, as far as we know, effects of changes of blood supply to the uterus after RT have never been discussed.
In this report, we looked at changes of the blood supply to the uterus in two patients who experienced pregnancy and delivery. RT seems to change blood flow to the uterine body through the neovascularization. However, we believe that the division of the descending branches of uterine arteries and vaginal arteries leads neither to a decrease of blood supply to, nor to the dysfunction of, the neo-cervix. And these procedures also do not affect the fetal growth and the placental growth. Furthermore, neovascularisation of the remaining uterine cervix would have been completed relatively early after the operation because both patients became pregnant within two years. Thus effects of changes of uterine blood flow on pregnancy courses seemed to be minimal. However, the following up of pregnancy in patients who underwent RT is still a challenge for obstetrician. Further clinical investigation to prevent pregnancy-related complications in patients who underwent RT would improve the pregnancy outcome of these patients.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Ushijima K. Current status of gynecologic cancer in Japan. J. Gynecol. Oncol. 2009;20:67-71
2. Ishika S, Endo T, Hayashi T, Kitajima Y, Sugimura M, Sagae S, Saito T. Successful delivery after vaginal radical trachelectomy for invasive uterine cervical cancer. Int. J. Clin. Oncol. 2006;11:146-149
3. Ishika S, Endo T, Hayashi T, Baba T, Umemura K, Saito T. Pregnancy-related complications after vaginal radical trachelectomy for early-stage invasive uterine cervical cancer. Int. J. Clin. Oncol. 2007;12:350-355
4. Nishio H, Fujii T, Kameyama K, Susumu N, Nakamura M, Iwata T, Aoki D. Abdominal radical trachelectomy as a fertility-sparing procedure in women with early-stage cervical cancer in a series of 61 women. Gynecol. Oncol. 2009;115:51-55
5. Sieunarine K, Boyle DC, Corless DJ, Noakes DE, Ungar L, Marr CE, Lindsay I, Del Priore G, Smith JR. Pelvic vascular prospects for uterine transplantation. Int. Surg. 2006;91:217-222
6. Salafia CM, Minior VK, Lopez-Zeno JA, Whittington SS, Pezzullo JC, Vintzileos AM. Relationship between placental histologic features and umbilical cord blood gases in preterm gestations. Am. J. Obstet. Gynecol. 1995:1058-64
7. Haezell AE, Moll SJ, Jones CJ, Baker PN, Croker JP. Formation of syncytial knots is increased by hyperoxia, hypoxia and reactive oxygen species. Placenta. 2007;28(Suppl. A):S33-40
8. Ishioka S, Ezaka Y, Umemura K, Hayashi T, Endo T, Saito T. Proteomic analysis of mechanisms of hypoxia-induced apoptosis in trophoblastic cells. Int. J. Med. Sci. 2007;4:36-44
9. Dargent D, Martin X, Sacchetoni A. et al. Laparoscopic vaginal radical trachelectomy: a treatment to preserve the fertility of cervical carcinoma patients. Cancer. 2000;88:1877-1882
10. Jolly JA, Battista L, Wing DA. Management of pregnancy after radical trachelectomy: case reports and systemic review of the literature. Am. J. Perinatol. 2007;24:531-539
11. Plante M. Vaginal radical trachelectomy: an update. Gynecol. Oncol. 2008;111:S105-S110
12. Martin X.J.B, Golfier F, Romestaing P, Raudrant D. First case of pregnancy after radical trachelectomy and pelvic irradiation. Gynecol.Oncol. 1999;74:286-287
Author contact
![]() Corresponding author: Shin-ichi Ishioka, Department of Obstetrics and Gynecology, Sapporo Medical University. Minami 1-jo, Nishi 16-chome, Chuo-ku, Sapporo Hokkaido, Japan 064-8543. Tel. +81-11-611-2111 (ext. 3373); Fax +81-11-563-0860; e-mail: ishiokaac.jp
Corresponding author: Shin-ichi Ishioka, Department of Obstetrics and Gynecology, Sapporo Medical University. Minami 1-jo, Nishi 16-chome, Chuo-ku, Sapporo Hokkaido, Japan 064-8543. Tel. +81-11-611-2111 (ext. 3373); Fax +81-11-563-0860; e-mail: ishiokaac.jp

 Global reach, higher impact
Global reach, higher impact