3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2009; 6(4):192-199. doi:10.7150/ijms.6.192 This issue Cite
Research Paper
OPERATIVE TREATMENT OF TRANSVERSE ACETABULAR FRACTURES: IS IT REALLY NECESSARY TO FIX BOTH COLUMNS?
1. MD, MSc, Attending Orthopaedic Trauma Surgeon, Serviço de Ortopedia e Traumatologia Prof. Nova Monteiro (SOT) - Hospital Municipal Miguel Couto (HMMC), Rio de Janeiro, RJ, Brasil
2. MD, MSc, Chief of Orthopaedic Trauma, Serviço de Ortopedia e Traumatologia Prof. Nova Monteiro, HMMC
3. MD, Attending Orthopaedic Trauma Surgeon, Serviço de Ortopedia e Traumatologia Prof. Nova Monteiro, HMMC
4. MD, PhD, Chief of Orthopaedic Division, Serviço de Ortopedia e Traumatologia Prof. Dr. Donato D'Ângelo, Hospital Santa Tereza, Petrópolis, RJ, Brasil
Received 2009-4-19; Accepted 2009-7-10; Published 2009-7-12
Abstract
Objective: we prospectively evaluated clinical and radiographic outcomes in patients with displaced combined transverse-posterior wall acetabular fractures managed at our Institution over a period of seven years by posterolateral single approach, direct posterior wall and posterior column reduction and plating, and indirect reduction of anterior column controlled by fluoroscopic images with or without lag-screw fixation. The aim was to identify if the obtained immediate postoperative Matta radiographic roof-arc angles after fracture reduction and fixation alters in the postoperative period when comparing posterior plating alone versus posterior plate and anterior column lag-screw fixation. Patients and Methods: 35 skeletally mature patients (31 male and four female, with mean age of 39.9 years old [range, 23.3 to 66.7 y/o]) with combined transverse-posterior wall acetabular fractures surgically treated by a posterolateral single approach were enrolled in this prospective investigation. Nineteen patients had associated orthopaedic injuries. The first part of the acetabular fracture management was similar to all patients and consisted in anatomical reduction and fixation of the transverse posterior component followed by anatomical reduction and fixation of the posterior wall component. The transverse anterior component reduction was controlled by fluoroscopic images (anteroposterior (AP), iliac oblique, and obturator oblique views) and digital palpation through the greater sciatic notch. Fifteen of the 35 patients had an additional lag-screw fixation from the posterior to the anterior columns with an extra-long small-fragment cortical screw. AP and Judet oblique radiographic views were taken at the end of the procedure and roof-arc angles were measured. Clinical results were assigned according to the grading system of Merle D'Aubigne´ and Postel as modified by Matta et al. Radiographic roof-arc angles were checked and compared between the two groups of patients to the same data collected both at the time of the surgical procedure and at three months postoperatively. Statistical analysis was done by either using chi-square (clinical outcome) and Mann-Whitney (roentgenographic outcome) tests, with a level of significance of α = 5%. Results: at final follow-up examination 18 to 84 months postoperatively (mean, 46.8 months), the clinical results were considered satisfactory in 31 (88.6%) patients (excellent in nine (25.7%) and good in 22 (62.9%) patients). There was no difference between patients with (n = 15) and without (n = 20) fixation of the transverse anterior component of the acetabular fracture (p = 0.67). Radiographic roof-arc angles measured at discharge, at three months postoperatively and at the last follow-up consultation didn't changed significantly (p > 0.05). There was no statistically significant difference between patients treated with (n = 15) and without (n = 20) fixation of the anterior component of the transverse acetabular fracture in terms of medial displacement of the femoral head. Conclusion: the authors suggest that associated transverse-posterior wall acetabular fractures can be managed by a single posterior approach. Direct reduction and fixation of the posterior wall and column components is an adequate option for these injuries. If there is adequate indirect reduction of the anterior column, as checked by digital palpation and fluoroscopy, we feel that it is not necessary to fix the anterior column component of the transverse acetabular fracture.
Keywords: acetabulum, fracture, transverse, posterior wall, roof-arc angle.
INTRODUCTION
Combined transverse-posterior wall type is one of the most common patterns of acetabular fracture, accounting for 24% to 32% of those lesions 1-3. Generally the main fracture line of the transverse component crosses the acetabular dome and displaces the weight-bearing area, ultimately altering hip mechanical forces 2,3. The effects of fracture malreduction or nonreduction are varied and most likely would result in posttraumatic arthritis.
Although currently there is no doubt of the benefits associated to the anatomical reduction of the displaced articular surface, the appropriate method of internal fixation is still subject of controversy. Conventional treatment concepts related to combined double or extensile approach and posterior and anterior column plating are considered today extremely aggressive. Many authors have demonstrated significant intra- and postoperative complications in patients treated with this protocol, including massive hemorrhage, deep wound infection, and functional heterotopic ossification 4,5.
Giving the severe consequences of a more invasive treatment protocol, recently few authors dealing with this problem have proposed the use of a single posterior approach for the management of combined transverse-posterior wall acetabular fractures 1,6-8. Normally the selected approach is determined by the amount of column displacement, however the associated presence of the posterior wall component makes the use of a posterior approach mandatory. Clinical and biomechanical investigations have shown the stiffest construction for the transverse component to combine a posterior column plate with an anterior column lag-screw, with loss of reduction ranging among 3% and 5% 9,10. Of course, this type of construction has its own associated morbidity. In fact, prolonged operative time and higher risk of articular penetration and neurovascular damage are still limiting factors 11. In addition, despite the results demonstrated by mechanical studies, anatomical articular surface reduction constitutes the cornerstone of proper treatment of this injury.
Matta et al have shown that the radiographic roof-arc angle is a useful technique for evaluating transverse acetabular fracture reduction 12. It is generally accepted that intra-operative roof-arc angles of 45° or more represents a satisfactory restitution of the weight-bearing portion of the acetabulum cavity 12. However, when there is an associated posterior wall fracture, the radiographic roof-arc measurement cannot be used at the preoperative period. Nevertheless, during the surgical procedure the wall fracture is primarily reduced and fixed, and the concept of roof-arc angle can be applied again for the transverse component. In this way, an even less aggressive and more biological surgical intervention should be considered. Additionally, Atchison et al. have found no significant difference when comparing posterior plating alone versus posterior plate and anterior column screw fixation for transverse acetabular fractures at both 0° and 90° of hip flexion 13. Likewise there is little evidence to support fixation of only one acetabular column in the management of combined transverse-posterior wall acetabular fractures, it seems reasonable based on the above mentioned studies 12,13.
At the current investigation, we prospectively evaluated clinical and radiographic outcomes in patients with displaced combined transverse-posterior wall acetabular fractures managed at our Institution over a period of seven years by posterolateral single approach, direct posterior wall and posterior column reduction and plating, and indirect reduction of anterior column controlled by fluoroscopic images with or without lag-screw fixation. The aim was to identify if the obtained intra-operative Matta radiographic roof-arc angles after wall reduction and fixation alters in the postoperative period when comparing posterior plating alone versus posterior plate and anterior column lag-screw fixation.
PATIENTS AND METHODS
Over a seven-year period at a single level-I Trauma Center all patients admitted to the Emergency Department with combined transverse-posterior wall acetabular fractures were primarily included in the study. Patients managed via double approach due to the transverse component and skeletally immature patients were excluded from the current study. Therefore, a consecutive series of 35 skeletally mature patients surgically treated by a posterolateral single approach were enrolled in this prospective investigation.
There were 31 male and four female patients with a mean age of 39.9 years old (ranging from 23.3 to 66.7 y/o). No patient had multiple trauma to other organs and systems. Nineteen patients had 21 associated orthopaedic injuries, including posterior dislocation of the hip (n = 08), ipsilateral femur shaft fracture (n = 06), ipsilateral femur and tibia shaft fractures (n = 02), and contralateral pelvic fracture (n = 03). Three patients had traumatic sciatic nerve dysfunction. Fracture-dislocations of the femoral head were promptly reduced after hospital admission by closed technique (Allis maneuver). The two patients with floating knee injury were managed primarily with transarticular external fixation.
Patients were operated on the first three weeks after admission (mean - 12 days [range - seven to 21 days]) via a posterolateral Kocher-Langenbeck (KL) approach. All orthopaedic injuries were treated at the same surgical procedure. For the acetabular lesion, patients were positioned on a fixed lateral position, with the hip extended and the knee flexed. Femoral shaft fractures were managed by antegrade nailing through the same approach during the acetabular fixation procedure. For the pelvic and tibia lesions patients were positioned supine. Pelvic fractures (all caused by external rotation force) were fixed either with plates and screws or percutaneous screws alone. Tibia shaft fractures were managed by interlocking nailing. Associated orthopaedic lesions and respective treatments are listed in Table I.
Associated orthopaedic lesions and respective treatments.
| Orthopaedic lesion | Patients (n = 19) | Treatment |
|---|---|---|
| Posterior dislocation of the hip | 08 | Closed reduction |
| Femoral shaft fractures | 08 | Antegrade reamed nailing |
| Tibia shaft fractures | 02 | Reamed nailing |
| Pelvic fractures | 03 | ------ |
| Horizontal transiliac fracture | 01 | Percutaneous screws |
| Sacro-iliac (SI) dislocation | 02 | Anterior SI double plating |
Source: SOT, HMMC, 2008
The first part of the acetabular fracture management was similar to all patients and consisted in anatomical reduction and temporary fixation of the transverse posterior component followed by anatomical reduction of the wall component and definitive fixation with plating and screws. The transverse anterior component reduction was controlled by fluoroscopic images (anteroposterior (AP), iliac oblique, and obturator oblique views) and manual palpation through the greater sciatic notch.
Fifteen patients had an additional lag-screw fixation from the posterior to the anterior column with an extra-long small-fragment cortical screw. The decision to fix or not the transverse anterior column component was based fundamentally on randomization by the surgeon at the operating room on the day of surgery. There was no significant difference between groups in respect to age, gender, fracture side and complexity, and number of associated lesions. No patient required either a trochanteric osteotomy or a prolongation of the upper part of the surgical incision. All patients were operated on by the same orthopaedic surgeon (VG).
AP and Judet oblique radiographic views were taken at the end of the procedure and roof-arc angles were measured by the surgeon. Postoperatively, intravenous antibiotic was administered for 24 hours (1st generation cephalosporin). Patients entered an institutional physical therapy program, on the basis of a gradual improvement of hip range of motion and quadriceps and gluteus muscles strengthening exercises. They were instructed to use crutches until unprotected, full weight bearing was permitted after all the fractures had healed (mean 12.8 weeks, ranging from 12.0 to 16.3 weeks). Indomethacin 75 mg daily was administered for six weeks beginning on postoperative day 1. Mechanical prophylaxis was done beginning the first day after the surgical procedure and used until patient discharge. No method of pharmacological prophylaxis against deep-vein thrombosis (DVT) was used. The median hospital stay was four days (ranging from two to five days).
After discharge from the hospital, patients were followed on at outclinic regimen on days 21, 45, 90, and 180 and one year after surgery. Then patients were examined once a year. Standard radiographs were taken at all outclinic consultations. At the time of the most recent follow-up, each patient was clinically and radiographically evaluated. Statistical analysis was done by either using chi-square (clinical outcome) and Mann-Whitney (roentgenographic outcome) tests, with a level of significance of α = 5%. Clinical results were assigned according to the grading system of Merle D'Aubigné and Postel as modified by Matta et al (Table II). Radiographic roof-arc angles were checked and compared between the two groups of patients to the same data collected both at the time of the surgical procedure and at three months postoperatively.
Grading system of Merle D'Aubigné and Postel modified (ref. 12).
| Pain | points | Ambulation | points | Range of motion (%) | points | Clinical grade (final score) |
|---|---|---|---|---|---|---|
| No pain | 6 | Normal | 6 | 100 | 6 | Excellent (18) |
| Slight or intermittent | 5 | No cane but slight limp | 5 | 80 | 5 | Good (15 - 17) |
| Mild after ambulation but disappears with rest | 4 | Long distances with cane or crutch | 4 | - | - | Fair (13 - 14) |
| Moderately severe, permits ambulation | 3 | Limited even with support | 3 | 60 | 3 | Poor (≤ 12) |
| Severe with ambulation | 2 | Very limited | 2 | - | - | |
| Severe, prevents ambulation | 1 | Bedridden | 1 | ≤ 40 | 1 |
Source: SOT, HMMC, 2008
RESULTS
In the current series, at final follow-up examination 18 to 84 months postoperatively (mean, 46.8 months), the clinical results were considered satisfactory in 31 (88.6%) patients (excellent in nine (25.7%) and good in 22 (62.9%) patients). There was no significant difference between patients with (14 satisfactory results) and without (17 satisfactory results) fixation of the anterior transverse component of the acetabular fracture (p = 0.67).
Of the 14 satisfactory results seen on patients with anterior column fixation, four were excellent and 10 were good. Of the 17 satisfactory results seen on patients without anterior column fixation, four were excellent and 13 were good.
Of the unsatisfactory clinical results (n = 04), three (8.6%) occurred in patients without fixation of the anterior column of the acetabulum. One (2.8%) patient had an avascular necrosis of the femoral head, but refused further treatment and is still seen at outpatient clinic yearly. One (2.8%) patient had a loss of articular reduction 45 days after discharge. She was a morbidly obese patient and refused a second operation at our institution. She has undergone joint replacement in another institution. Posttraumatic osteoarthritis of the hip was seen in another patient and he was submitted to a total hip replacement 24 months after the index surgical procedure. The last unsatisfactory outcome occurred in a patient who had lag-screw fixation of the anterior column of the acetabulum. He developed an osteonecrosis of the femoral head 12 months after the trauma and underwent total hip replacement at this time.
Sciatic nerve palsy was seen in three patients at the time of hospital admission, but resolved completely after a mean of 12 months. Two (18.2%) patients with an associated femoral shaft fracture complicated during the postoperative period. One of them developed a persistent drainage through the stab incisions used to distally lock the intramedullary nail. Screws were removed just after the femoral fracture healed and the drainage resolved uneventfully. The other patient developed a vascular hypertrophic nonunion and was managed by exchange nailing just after this diagnosis. The fracture finally healed 20 weeks after the second operation with a residual limb shortening of 13 mm. Of the two patients treated by tibial nailing, both went to consolidation of the fracture without any healing disturbance. However, one of them required nailing removal due to persistent anterior knee pain (despite adequate introduction of the nail tip and no patellar ligament impingement). Finally, all patients with an associated pelvic lesion showed a satisfactory result during the last outclinic consultation. Figures 1 to 3 illustrate cases from the actual series.
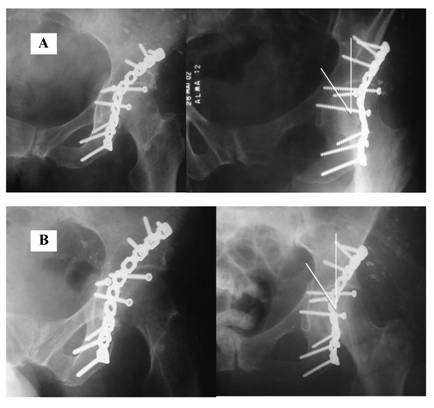
Except for the patient who had loss of articular reduction, the other 34 patients showed acetabular fracture healing at 12 weeks as shown by roentgenological examination. Post-operative reduction checked before patient discharge showed radiographic Matta angle superior to 45o in all cases of the current study. Radiographic roof-arc angles measured at three months postoperatively and at the last follow-up consultation didn't changed significantly (p > 0.05). There was no statistically significant difference between patients treated with and without fixation of the anterior component of the transverse acetabular fracture in terms of medial displacement of the femoral head (due to inadequate quadrilateral plate buttressing). Immediate post-operative and last follow-up consultation radiographs of a patient without anterior column fixation are demonstrated in Figure 3.
Pre-operative radiographs and CT scan, and postoperative radiographs of a patient (31 y/o female, road-traffic accident, unrestrained) who had fixation of the anterior component of the transverse acetabular fracture with an extra-long small fragment cortical screw ('home-run screw'). Note that the long screw bends as a result of the intimate contact with the pelvic brim. Follow-up duration of 18 months.
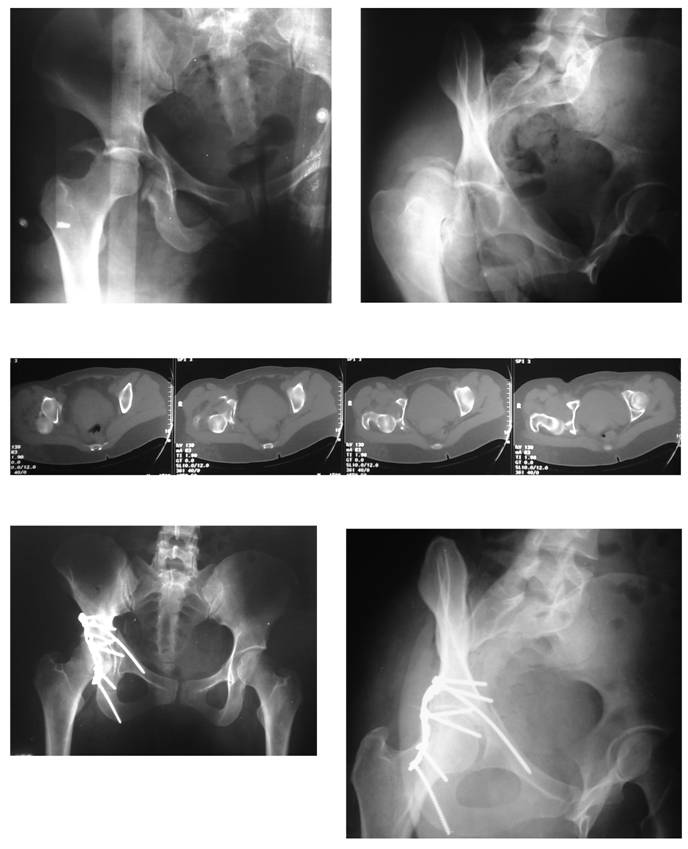
Pre-operative radiographs and CT scan, and postoperative radiographs of a patient (57 y/o male, road-traffic accident, unrestrained) without fixation of the anterior component of the transverse acetabular fracture with. Observe the anatomic reduction of both column of the acetabulum and the perfect congruency between the femoral head and the roof. Follow-up duration of 26 months.

Immediate postoperative and last outclinic consultation radiographs of a patient (66.7 y/o female, road-traffic accident, unrestrained) without fixation of the anterior component of the transverse acetabular fracture. Roof-arc measurements didn't alter and the fracture healed uneventfully. After 56 months from the surgery, there are no signs of arthritis.
In order to check for any bias due to the small number of patients on the current investigation, retrospective power analysis was calculated. Post-hoc analysis showed an adequate effect size on the population studied.
DISCUSSION
Transverse and posterior wall fractures of the acetabulum is a frequent combination 2,3. Generally the femoral head acts as a hammer and dislocates the main components of the fracture either posteriorly or medially 3. The displacement changes the shape of the acetabulum cavity altering the normal hip forces shared equally by the dome and the walls. Abnormal loads applied to the hip joint ultimately leads to cartilage degeneration and early posttraumatic arthritis. For this reason, treatment consists in anatomical restitution of joint congruity, stable fixation of the fracture components, and early hip motion.
Until recently transverse-posterior wall acetabular fractures were treated by direct reduction via anterior and posterior approaches, and internal fixation using plates and screws. Although adequate in terms of bone exposure, there were an extensive intraoperative bleeding and a higher risk of neurovascular damage. Probably because of the elevated rate of morbidity associated to the procedure, other options were gradually described for the management of this type of fracture.
Currently transverse-posterior wall acetabular fractures are preferably treated by a single posterior approach. Reduction and fixation of the displaced posterior wall and column components are carried out through direct visualization and the anterior component is stabilized with one lag-screw passed from the posterior to the anterior column of the acetabulum. Although this construct reduces extensile dissection related complications and provides adequate strength and stiffness, some potential problems are still pointed out, as a longer operative time and a higher risk of implant articular penetration and neurovascular lesion 7,11,14.
In the current study, a group of patients with associated transverse-posterior wall acetabular fractures were treated without fixation of the anterior column. Two recent biomechanical investigations support this technique for transverse acetabular fractures. In one study, Atchison et al showed no significant difference when comparing posterior plating alone versus posterior plate and anterior column screw fixation at both 0° and 90° of hip flexion 13. In another study, Chang et al demonstrated significantly greater yield and maximum strength of fixation with posterior column plate and screw construct when compared both to two lag-screws and screw and wire techniques 15. Although, these experiments have been conducted in isolated transverse acetabular fracture models, we hypothesized that it can be extrapolated for transverse-posterior wall lesions if direct reduction and fixation of the wall fracture is performed. Therefore, one should address the transverse component as it was an elementary fracture.
By using roof-arc measurements as described by Matta et al 12, we found no significant difference between patients with and without anterior column fixation. As it was not the aim of this study, operative time, radiation exposure, and bleeding were not evaluated. However, it seems obvious that all of these variables tend to be reduced if the surgeon does not fix the anterior column component of the fracture. Moreover, iatrogenic neurovascular trauma also seems to be more preventable by avoiding the anterior quadrants of the acetabulum 11.
Finally, transverse acetabular fractures are characterized by a unique distal bone block, with no separation into ischium and pubis fragments (as occurs in the “T” type pattern), and a perfect reduction of the posterior column implies a perfect reduction of the anterior column, without rotation 2,3. Obviously it is necessary to have adequate intraoperative fluoroscopic images in order to verify a correct alignment and continuity of the ilioischium line (by using the obturator oblique view of Judet). Other important and definitive step for the success of the procedure is the palpation of the anterior column through the greater sciatic notch. If there is any doubt about a perfect reduction of the anterior column, we do not recommend leave it without fixation. Although this was not currently investigated (as it was not a problem observed for us), trochanteric osteotomy with or without surgical dislocation of the hip may help in reducing the anterior column component of the fracture.
In terms of mechanical stability of the construction, Chang et al and Shazar et al have shown sufficient stability with a posterior column plate with two screws on each side of the fracture 15,16.
On the basis of our observations, it is reasonable to suggest that associated transverse-posterior wall acetabular fractures can be managed by a single posterior approach. Direct reduction and fixation of the posterior wall and column components is an adequate option for these injuries. It is not necessary to fix the anterior column component of the transverse fracture.
CONFLICT OF INTEREST
The authors have declared that no conflict of interest exists.
References
1. Giordano V, Amaral NP, Franklin CE, Pallottino A, Albuquerque RP, Giordano M. Functional outcome after operative treatment of displaced fractures of the acetabulum: a 12-month to 5-year follow-up investigation. Eur J Trauma Emerg Surg. 2007;33:520-7
2. Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction: preliminary report. J Bone Joint Surg [Am]. 1964;46:1615-46
3. Letournel E. Acetabulum fractures: classification and management. Clin Orthop Rel Res. 1980;151:81-106
4. Kaempfe FA, Bone LB, Border JR. Open reduction and internal fixation of acetabular fractures: Heterotopic ossification and other complications of treatment. J Orthop Trauma. 1991;3:439-45
5. Oh C-W, Kim P-T, Park B-C, Kim S-Y, Kyung H-S, Jeon I-H, Cheon S-H, Min W-K. Results after operative treatment of transverse acetabular fractures. J Orthop Sci. 2006;11:478-84
6. Gross T, Jacob AL, Messmer P, Regazzoni P, Steinbrich W, Huegli RW. Transverse acetabular fracture: hybrid minimal access and percutaneous CT-navigated fixation. AJR. 2004;183:1000-2
7. Parker JP, Copeland C. Percutaneous fluoroscopic screw fixation of acetabular fractures. Injury. 1997;28:597-600
8. Starr AJ, Reinert CM, Jones AL. Percutaneous fixation of the columns of the acetabulum: A new technique. J Orthop Trauma. 1998;12:51-8
9. Thomas KA, Vrahas MS, Noble JW Jr, Bearden CM, Reid JS. Evaluation of hip stability after simulated transverse acetabular fractures. Clin Orthop Rel Res. 1997;340:244-56
10. Vrahas MS, Widding KK, Thomas KA. The effects of simulated transverse, anterior column, and posterior column fractures of the acetabulum on the stability of the hip joint. J Bone Joint Surg [Am]. 1999;81:966-74
11. Feugier P, Fessy MH, Béjui J, Bouchet A. Acetabular anatomy and the relationship with pelvic vascular structures. Implications in hip surgery. Surg Radiol Anat. 1997;19:85-90
12. Matta JM, Anderson LM, Epstein HC. et al. Fractures of the acetabulum: A retrospective analysis. Clin Orthop Rel Res. 1986;205:230-40
13. Atchison SM, Mukherjee DP, Kruse RN, Mayeux R, Albright JA. Internal fixation of transverse acetabular fractures. Proceedings of the Fourteenth Southern Biomedical Engineering Conference. 1995;7:55-6
14. Ebrahein NA, Xu R, Biyani A, Benedetti JA. Anatomic basis of lag screw placement in the anterior column of the acetabulum. Clin Orthop Rel Res. 1997;339:200-5
15. Chang J-K, Gill SS, Zura RD, Krause WR, Wang G-J. Comparative strength of three methods of fixation of transverse acetabular fractures. Clin Orthop Rel Res. 2001;392:433-41
16. Shazar N, Brumback RJ, Novak VP, Belkoff SM. Biomechanical evaluation of transverse acetabular fracture fixation. Clin Orthop Rel Res. 1998;352:215-22
Author contact
![]() Correspondence to: Dr. Vincenzo Giordano, Rua Aristides Espínola 11/301, Leblon, CEP: 22440-050, Rio de Janeiro, RJ, Brasil. Tel/Fax: 21 2274-6830. E-mail: sot.hmmccom.br
Correspondence to: Dr. Vincenzo Giordano, Rua Aristides Espínola 11/301, Leblon, CEP: 22440-050, Rio de Janeiro, RJ, Brasil. Tel/Fax: 21 2274-6830. E-mail: sot.hmmccom.br

 Global reach, higher impact
Global reach, higher impact