3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2009; 6(4):143-155. doi:10.7150/ijms.6.143 This issue Cite
Research Paper
Comparison of a Two-Lead, Computerized, Resting ECG Signal Analysis Device, the MultiFunction-CardioGramsm or MCG (a.k.a. 3DMP), to Quantitative Coronary Angiography for the Detection of Relevant Coronary Artery Stenosis (>70%) - A Meta-Analysis of all Published Trials Performed and Analyzed in the US
The Valley Hospital, Ridgewood, NJ and Columbia University College of Physicians and Surgeons, New York, NY, USA
Received 2009-1-19; Accepted 2009-4-6; Published 2009-4-7
Abstract
Background: Accurate, non-invasive diagnosis of, and screening for, coronary artery disease (CAD) and restenosis after coronary revascularization has been a challenge due to either low sensitivity/specificity or relevant morbidity associated with current diagnostic modalities.
Methods: To assess sensitivity and specificity of a new computerized, multiphase, resting electrocardiogram analysis device (MultiFunction-CardioGramsm or MCG a.k.a. 3DMP) for the detection of relevant coronary stenosis (>70%), a meta-analysis of three published prospective trials performed in the US on patient data collected using the US manufactured device and analyzed using the US-based software and New York data analysis center from patients in the US, Germany, and Asia was completed. A total of 1076 patients from the three trials (US - 136; Germany - 751; Asia - 189) (average age 62 ± 11.5, 65 for women, 60 for men) scheduled for coronary angiography, were included in the analysis. Patients enrolled in the trials may or may not have had prior angiography and/or coronary intervention. Angiographic results in all studies were classified for hemodynamically relevant stenosis (> 70%) by two US based angiographers independently.
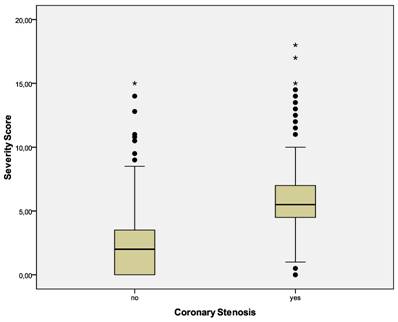
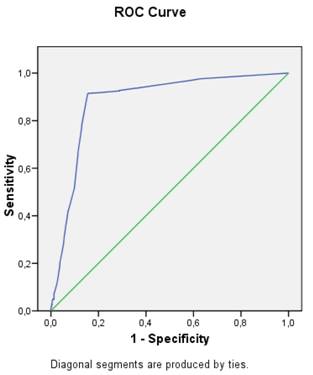
Results: Hemodynamically relevant stenosis was diagnosed in 467 patients (43.4%). The device, after performing a frequency-domain, computational analysis of the resting ECG leads and computer-database comparison, calculated a coronary ischemia “severity” score from 0 to 20 for each patient. The severity score was significantly higher for patients with relevant coronary stenosis (5.4 ± 1.8 vs. 1.7 ± 2.1). The study device (using a cut-off score for relevant stenosis of 4.0) correctly classified 941 of the 1076 patients with or without relevant stenosis (sensitivity-91.2%; specificity-84.6%; NPV 0.942, PPV 0.777). Adjusted positive and negative predictive values (PPV and NPV) were 81.9% and 92.6%, respectively (ROC AUC = 0.881 [95% CI: 0.860-0.903]). Subgroup analysis showed no significant influence of sex, age, race/nationality, previous revascularization procedures, resting ECG morphology, or participating center on the device's diagnostic performance.
Conclusions: The new computerized, multiphase, resting ECG analysis device (MultiFunction-CardioGramsm) has been shown in this meta-analysis to safely and accurately identify patients with relevant coronary stenosis (>70%) with high sensitivity and specificity and high negative predictive value. Its potential use in the evaluation of symptomatic patients suspected to suffer from coronary disease/ischemia is discussed.
Keywords: coronary artery disease, ECG analysis, Coronary Artery Stenosis
Introduction
Coronary artery disease (CAD) is the single leading cause of death in the developed world and is responsible for more than 30% of all deaths in most Organization for Economic Co-operation and Development (OECD) countries [1]. Between 15% and 20% of all hospitalizations are the direct results of CAD [1]. CAD is responsible for 7.2 million deaths annually worldwide and is also an increasing cause of concern in the developing world [2]. In the USA alone the prevalence of CAD is estimated at 5.9% of all Caucasians of age 18 and older [3].
Accurate, non-invasive diagnosis of, and screening for, CAD and restenosis after coronary revascularization has been an elusive challenge. Electrocardiographic methods are routinely used as the first tools for initial screening and diagnosis in clinical practice. The low sensitivity and specificity of these methods makes them less than ideal diagnostic and prognostic indicators of CAD, however [4]. When used by non-specialists, the 12-lead resting ECG shows a sensitivity of less than 50% in diagnosing myocardial infarction [5].
Sensitivity, and to a lesser extent specificity, can be enhanced by different exercise or stress test methods, such as ECG stress testing, nuclear stress testing, or stress echocardiography. Nevertheless, even their sensitivity and specificity are limited, especially in single-vessel CAD [6]. Moreover, stress testing requires significant personnel and time resources, is contraindicated in relevant patient populations, and bears a small but measurable morbidity and mortality [7, 8]. ECG-based methods are even less sensitive in patients after coronary revascularization [9, 10, 11] and may be contraindicated immediately after intervention. Finally, in a recently published cohort study of 8176 consecutive patients presenting with chest pain [43], designed to determine whether the resting and exercise ECG provided prognostic information incremental to medical history, in accurately identifying those at higher risk of Acute Coronary Syndrome and death during a median follow-up of 2.46 years, showed that 47% of all events during follow-up occurred in patients with a negative exercise-ECG result. This study emphasized the limitations of resting or stress-ECGs for risk assessment and highlighted the need for new tests to assess this patient population.
Coronary angiography remains the gold standard for the morphologic diagnosis of CAD and also allows revascularization during the same procedure [12, 13]. Coronary angiography is a relatively safe and effective intervention, yet it is resource-intensive, expensive, and invasive [14, 15]. Non-invasive cardiac imaging techniques such as multi-slice computed tomography (CT), high-resolution magnetic resonance imaging/angiography (MRI/MRA), electron beam angiography (EBA), or positron-emission tomography with CT (PET-CT) have an alleged high sensitivity and specificity for detecting morphologic coronary lesions, and some even claim to permit the functional assessment of myocardial perfusion. Yet these techniques are also not ideal as they are, among other things, expensive, require significant staff and time resources, and lead to significant X-ray radiation exposure (CT, EBA, PET-CT) and/or contrast exposure (MRI/MRA, CT, PET-CT) of the patient [16, 17].
Several methods have been proposed and developed to enhance sensitivity and specificity of the resting ECG for diagnosis of symptomatic and asymptomatic CAD. In theory, such methods may improve diagnostic quality for non-specialists. Yet, diagnostic ECG computer programs have not been shown to be equal or superior to specialist physician's judgment [18]. Moreover, studies comparing computerized with manual ECG measurements in patients with acute coronary syndrome have shown that computerized measurements have diagnostic cut-offs that differ from manual measurements, and they may not be used interchangeably [19]. This is likely one of the reasons underlying the limited acceptance of such techniques in clinical practice.
The present study compared a new computer-enhanced, multi-phase, resting ECG analysis device, MultiFunction-CardioGramsm or MCG (a.k.a 3DMP), to immediate and subsequent coronary angiography to evaluate the device's accuracy in detecting the presence and recurrence of hemodynamically relevant CAD.
Materials and Methods
Data from three published trials of the use of MCG in the identification of relevant coronary stenosis was used in this meta-analysis. The included studies were all carried out using the US FDA-approved Premier Heart'sTM MCG device on patients undergoing standard coronary angiography at a total of seven medical centers (Westchester Medical Center, Valhalla, NY, Siegburg Heart Hospital, Siegburg, Germany, and five medical centers in Asia - Center A, Cardiovascular Center, Seoul National University Bundang Hospital, Gyeonggi-do, South Korea, Center B, Mount Elizabeth Medical Centre, Singapore, Center C, Tokyo Heart Center, Tokyo, Japan, Center D, Wockhardt Heart Hospital, Mumbai, India, and Center E, HSC Medical Center, Kuala Lumpur, Malaysia) after its use was approved by the respective institutional review boards. Written informed consent was waived by each participant as a result of the disclosed non-risk designation of the study device. All patients received a full explanation and gave verbal consent to the study and the use of their de-identified data. Patients were only included if they underwent MCG testing prior to the scheduled reference coronary angiogram.
Patients Enrolled
A total of 1076 patients scheduled for coronary angiography were included in the meta-analysis. These represented a convenience sample of patients in the respective institutions in that each patient was already scheduled for the reference coronary angiography for any indication. Coronary angiographic data was recorded digitally and on cine angiographic film and was sent back to the United States for expert review by two independent US interventional cardiologists. Thirty patients from HSC Medical Center, Kuala Lumpur, Malaysia had to be excluded from the study because angiograms were not made available for US external review due to unforeseen legal limitations. Moreover, during the study a total of 84 patients (7.2%) were excluded due to inability to obtain adequate MCG two-lead ECG tracing quality (64 Westchester, 17 Siegburg, 3 Asia Centers) and were not included in this meta-analysis. The reasons for the poor technical quality of the MCG ECG recordings related primarily to unavoidable kinetic or electromagnetic field artifact, 60-cycle interference, lower frequency ambient noises, or poor lead placements. The included patient population had no overlap with any previously published or un-published study or with the actual independently validated MCG clinico-pathologic reference database of 40,000 patients accumulated over more than two decades. The MCG reference database used in the computer-database comparative analysis of each patient's data, was not modified or updated during the study period. Patient demographics, medical history, and risk factors apart from sex, age, height, weight and three samples of 82 second resting two ECG data were not recorded because they are not required for the MCG analysis.
Study device
The study device used in all patients in each included trial, MCG (a.k.a. 3DMP), is manufactured in the US by Premier Heart, LLC, Port Washington, NY, and records a simultaneous 2-lead resting ECG from leads II and V5 for 82 seconds using proprietary hardware and software. The analog MCG ECG signal is amplified, digitized, and down-sampled to a sampling rate of 100 Hz to reduce data transmission size; subsequent data transformations performed on the data do not require higher than 100 Hz/sec resolution. The digitized MCG ECG data was encrypted by the device at each study location and securely transmitted over the Internet to a central server located in New York, NY for final analysis and reporting.
At the central server location in New York, a series of Discrete Fourier Transformations (DFT) and post DFT signal averaging are performed on the data from the two ECG leads during the 82 second sampling period followed by signal averaging. The final averaged digital data, obtained from multiple cardiac cycles, is then subjected to six mathematical transformations (auto power spectrum, coherence, phase angle shift, impulse response, cross correlation, and transfer function - thus the trademark MultiFunction CardioGram) in addition to an amplitude histogram, which generates a large inventory of normalized mathematical indexes of abnormality. It is the pattern of these mathematical indexes of abnormality, obtained from analysis of multiple cardiac cycles of the resting ECG not a specific time-based segment of data (i.e. ST segment), that contains the deviations from normal that are measured by the MCG device. The resulting mathematically integrated patterns of the abnormal indexes are then compared for their degree of abnormality to the abnormal index patterns in the reference database to reach a final diagnostic output. The diagnostic output is represented as a combination of the disease severity score from 0 to 20 and the presence of local or global ischemia, which indicates the level of coronary obstruction/myocardial ischemia that is present in the study patient.
The reference clinico-pathologic database, against which the patient's MCG index patterns are compared, originated from data-gathering trials conducted from 1978 to 2000 in more than 30 institutions in Europe, Asia, and North America on individuals of varying ages and degrees of coronary disease state including 10,000 normals with no definable coronary disease [20, 21]. All MCG data and spectral analyses included in the database were performed using the same “made in USA” equipment as in the included trials and were analyzed using the same software and hardware located at the central server location in New York. All MCG analyses in this database have been validated against the final medical and angiographic diagnoses, confirmed by two independent academic angiographers having access to all the diagnostic tests including angiography results, lab, and cardiac enzyme test results.
One important difference between MCG and other ECG methods is that the MCG digitized analog electrocardiogram signals are locally recorded, but remotely analyzed at a central US data facility, due to the size and complexity of the digital signal processing, the analysis by multiple mathematic functions, and the required comparison to the reference clinico-pathologic database. Further aspects of the underlying technology and methodology have been described elsewhere [20, 21, 22].
MCG ECG acquisition and processing
MCG tests were conducted as follows by a trained trial site technician as part of a routine electrocardiographic workup received by each patient < 24 hours (average 2.5 hrs) prior to angiography. Patients were tested while quietly lying supine following 20 minutes of bed rest. Five ECG wires with electrodes were attached from the MCG machine to the patient at the four standard limb lead and precordial lead V5 positions. An automatic 82-second simultaneous two-lead (leads V5 and II) ECG sample was acquired with amplification and digitization. During the sampling, the ECG tracings displayed on the MCG screen were closely monitored for tracing quality.
The digital data was then de-identified, encrypted, and sent via a secure Internet connection to the central server in New York A second identical copy of the data was saved on the site MCG machine for post-study verification purposes before the data analysis was carried out. The quality of the tracing was visually rechecked and graded as “good,” “marginal,” or “poor”. A poor tracing was defined by one of the following:
- five or more 5.12-second segments of ECG data containing baseline artifact that deviated from the baseline by ≥2 mm and appears ≥10 times,
- two or more 5.12-second segments of ECG data containing baseline artifact that deviated from the baseline by ≥5 mm,
- in a 25-mm section of waveform in any 5.12-second segment of the ECG data, the waveform strays from the baseline by ≥3 mm,
- a radical deviation away from the baseline angle of at least 80° with peak amplitude of ≥2 mm measured from the baseline, occurring two or more times,
- a single episode of radical deviation away from the baseline angle of at least 80° with peak amplitude of ≥5 mm measured from the baseline.
A marginal tracing was defined by significant baseline fluctuations that did not meet the above criteria. A good tracing had no significant baseline artifact or baseline fluctuation. Tracings consistently graded as poor after repeated sampling were excluded from the present study, as noted above. All other tracings were included in the study.
MCG provided automatic diagnosis of regional or global ischemia, including silent ischemia, due to coronary artery disease and calculated a severity score ranging from 0 to 20 where a higher score indicated a higher likelihood of myocardial ischemia due to coronary stenosis. Following the MCG manufacturer's recommendation, a cut-off of 4.0 for the severity score was used in this meta-analysis; a score of 4.0 or higher was considered indicative of a hemodynamically relevant coronary artery stenosis of >70% in at least one large-sized vessel.
Angiographers and staff at each study site were blinded to all MCG results and findings. The MCG technicians and all Premier Heart staff were blinded to all clinical data including pre-test probabilities for CAD and the coronary angiography findings from the study patients.
Angiography
After the MCG test, coronary angiography was performed at the discretion of the attending physicians and following the standards of the institution. Angiographers were blinded to the MCG test results. Angiograms were classified by the respective angiographer and independently by two US based academic research angiographers within 4 weeks after the angiogram. If the two independent investigators did not agree on the results, they discussed the angiograms and conferred with the US study monitor until agreement was reached. Angiograms were classified as follows:
Non-obstructive CAD: angiographic evidence of coronary artery stenosis of ≤70% in a single or multiple vessels. Evidence included demonstrable vasospasm, delayed clearance of contrast medium indicating potential macro- or micro-vascular disease, or CAD with at least 40% luminal encroachment observable on angiograms. These patients were classified as negative for hemodynamically relevant CAD (= “stenosis: no”).
Obstructive CAD: angiographic evidence of coronary artery sclerosis of >70% in a single or multiple vessels, with the exception of the left main coronary artery, where ≥50% was considered obstructive. These patients were classified as positive for hemodynamically relevant CAD (= “stenosis: yes”).
The results from the angiograms represent the diagnostic endpoint against which MCG was tested.
Statistical Methods
The data acquisition process, all angiography reports, and all MCG test results were monitored by an independent, US cardiologist, study monitor formerly based at the National Institutes of Health, who verified the double-blindness of the study and the data integrity. Two, independent, academic research cardiologists from US, reviewed the coronary angiographic data for each patient. In the event of disagreement among the academic research cardiologists, discussion with the study monitor occurred until agreement was achieved.
Descriptive statistics were calculated for all variables. Differences between paired or two unpaired mean values were analyzed with the t-test, and degrees of freedom were adjusted according to a variance estimate if the F-test could not show equality of variances. Differences between more than two mean values were analyzed with the Scheffé test where homogeneity of variances was assessed with the Levene statistic. For two-way and multi-way tables, Fisher's exact test was used to calculate significance levels.
Odds ratios including 95% confidence intervals were calculated. Sensitivity and specificity were calculated as were receiver operating characteristic (ROC) curves including an estimate of the area under the curve (AUC). Positive and negative predictive values (PPV, NPV) for the assessment of coronary stenosis were calculated with adjustment to prevalence of stenosis [23]. Moreover, to assess the performance of the prediction of stenosis independent of the prevalence of stenosis, the positive and negative likelihood ratios (LR) were calculated [24]. A value of p <0.05 was considered statistically significant. All analyses were done with SPSS for Windows Version 15 (SPSS Inc., Chicago, IL, USA).
Results
Final analysis was performed on 1076 patients. Patients excluded from analysis (as noted above in Methods) for either poor MCG digitized analog ECG signal quality or inability to undergo US expert review of their angiography were not significantly different from the included patients with respect to age (59.4 +/- 10.7 vs. 61.3 +/- 12.9 years; p = 0.909) and sex (18% female vs. 30%; p = 0.210). Included patients comprised 686 men and 390 women with an average age of 62.0 +/- 11.5 years (21-88). Women were significantly older than men (65.0 +/- 10.9 vs. 60.3 +/- 11.4 years; p <0.05). (Table 1.)
Listing Of Average Age By Gender And By Center Of Patients Included In The Meta-Analysis. SD = standard deviation, n = number of patients in each group.
| Sex | Total | ||||
|---|---|---|---|---|---|
| female | male | ||||
| Age (years) | Age (years) | ||||
| Center | Germany (Center S) | Mean | 65.32 | 60.46 | 62.24 |
| SD | 10.58 | 10.73 | 10.92 | ||
| n | 276 | 475 | 751 | ||
| % | 38.6 | 61.4 | 100.0 | ||
| Asia (Overall) | Mean | 65.14 | 59.58 | 61.26 | |
| SD | 10.80 | 13.43 | 12.92 | ||
| n | 57 | 132 | 189 | ||
| % | 32.1 | 67.9 | 100.0 | ||
| Asia - Center A | Mean | 63.4 | 60.1 | 61.1 | |
| SD | 9.3 | 13.4 | 12.4 | ||
| n | 19.0 | 46.0 | 65.0 | ||
| % | 30.3 | 69.7 | 100.0 | ||
| Asia - Center B | Mean | 59.1 | 56.5 | 57.5 | |
| SD | 8.6 | 10.5 | 9.7 | ||
| n | 7.0 | 12.0 | 19.0 | ||
| % | 37.9 | 62.1 | 100.0 | ||
| Asia - Center C | Mean | 73.3 | 70.0 | 71.1 | |
| SD | 8.6 | 9.7 | 9.4 | ||
| n | 15.0 | 29.0 | 44.0 | ||
| % | 35.2 | 64.8 | 100.0 | ||
| Asia - Center E | Mean | 62.1 | 53.2 | 55.5 | |
| SD | 11.6 | 12.2 | 12.6 | ||
| n | 16.0 | 45.0 | 61.0 | ||
| % | 29.4 | 70.6 | 100.0 | ||
| USA (Center W) | Mean | 63.21 | 60.89 | 61.86 | |
| SD | 12.48 | 12.05 | 12.24 | ||
| n | 57 | 79 | 136 | ||
| % | 42.8 | 57.2 | 100.0 | ||
| Total | Mean | 64.98 | 60.34 | 62.02 | |
| SD | 10.90 | 11.44 | 11.46 | ||
| n | 390 | 686 | 1,076 | ||
| % | 38.0 | 62.0 | 100.0 | ||
Gender distribution was not significantly different between all medical centers included in the meta-analysis (p = 0.340). Patients from Asia Center C, the Tokyo Heart Center, Tokyo, Japan, were significantly older than those of all other Asia centers (p <0.05, details in table 1). Females were older in all centers, although differences did not always reach statistical significance. (Table 2.)
Average Age And Number Of Patients By Center, Sex, And Prior Revascularization Status. n = number of patients in each group, SD = standard deviation, N/A = not applicable.
| Revascularization | Total | ||||||
|---|---|---|---|---|---|---|---|
| no | yes | ||||||
| Sex | Sex | ||||||
| female | male | female | male | ||||
| Age (years) | Age (years) | Age (years) | Age (years) | ||||
| Country | Germany (Siegburg) | Mean | 64.34 | 59.94 | 68.36 | 61.71 | 62.24 |
| SD | 11.08 | 11.00 | 8.20 | 9.97 | 10.92 | ||
| n | 209 | 336 | 67 | 139 | 751 | ||
| Asia (Multi-Center) | Mean | 64.60 | 57.73 | 68.00 | 64.91 | 61.26 | |
| SD | 10.25 | 12.92 | 13.74 | 13.62 | 12.92 | ||
| n | 48 | 98 | 9 | 34 | 189 | ||
| Asia - Center A | Mean | 63.22 | 57.91 | 67.00 | 66.42 | 61.09 | |
| SD | 9.53 | 13.73 | 11.10 | 10.61 | 12.38 | ||
| n | 18.00 | 34.00 | 1.00 | 12.00 | 65.00 | ||
| Asia - Center B | Mean | 62.00 | 53.50 | 55.33 | 59.50 | 57.47 | |
| SD | 6.73 | 6.16 | 10.69 | 13.56 | 9.69 | ||
| n | 4.00 | 6.00 | 3.00 | 6.00 | 19.00 | ||
| Asia - Center C | Mean | 71.17 | 69.19 | 82.00 | 70.92 | 71.11 | |
| SD | 8.18 | 9.13 | 3.61 | 10.70 | 9.40 | ||
| n | 12.00 | 16.00 | 3.00 | 13.00 | 44.00 | ||
| Asia - Center E | Mean | 61.50 | 53.83 | 66.50 | 43.67 | 55.51 | |
| SD | 11.80 | 11.77 | 13.44 | 16.80 | 12.59 | ||
| n | 14.00 | 42.00 | 2.00 | 3.00 | 61.00 | ||
| USA (Westchester) | Mean | 63.21 | 60.89 | .N/A | .N/A | 61.86 | |
| SD | 12.48 | 12.05 | . | . | 12.24 | ||
| n | 57 | 79 | 136 | ||||
| Total | Mean | 64.18 | 59.66 | 68.32 | 62.34 | 62.02 | |
| SD | 11.20 | 11.57 | 8.91 | 10.82 | 11.46 | ||
| n | 314 | 513 | 76 | 173 | 1,076 | ||
Two hundred forty nine patients (23% of those included in the analysis) had either percutaneous coronary intervention (PCI) (188 or 17.3%) or coronary artery bypass grafting (61 or 5.7%) for revascularization 6 or more weeks before inclusion in the study. All other patients (827 or 77%) had no coronary revascularization procedure in their medical history. Patients with previous revascularization were significantly older (p <0.05) and more frequently male, although this difference was not statistically significant (p = 0.185). There were significant differences in the frequency of patients with revascularization between the centers (details in table 2).
Hemodynamically relevant coronary stenosis was diagnosed by angiography in 467 patients (43.4%). Although the percentage of patients with relevant coronary stenosis varied between centers, these differences were not significant (p = 0.563). There were no significant age differences between patients with and without angiographically proven relevant coronary stenosis (p = 0.389). There were also no significant gender differences (p = 1.000). Patients with revascularization procedures in their medical history were less frequently diagnosed with relevant coronary stenosis, although this difference was also not statistically significant (p = 0.117). However, patients with prior revascularization of any type were correctly identified as having relevant stenosis a higher percentage of the time (90% vs 87%) than patients without prior revascularization. In the case of prior PCI, patients with relevant stenosis were identified correctly by MCG 89% of the time and in the case of prior CABG, patients with relevant stenosis were identified correctly 93% of the time. The negative predictive value of an MCG score ≤ 4 in patients with prior PCI was 95.2% and in patients with prior CABG the NPV was 100 %. (Table 3).
Average Age By Center, Country, Sex, And Revascularization Status And The Presence Or Absence Of Relevant Coronary Stenosis > 70%. n = number of patients in each group, SD = standard deviation.
| Coronary Stenosis >70% | Total | ||||
|---|---|---|---|---|---|
| no | yes | ||||
| Age (years) | Age (years) | ||||
| Centers | A | Mean | 58.10 | 65.88 | 61.09 |
| SD | 13.52 | 8.54 | 12.38 | ||
| n | 40 | 25 | 65 | ||
| B | Mean | 57.22 | 57.70 | 57.47 | |
| SD | 9.22 | 10.58 | 9.69 | ||
| n | 9 | 10 | 19 | ||
| C | Mean | 70.73 | 71.93 | 71.11 | |
| SD | 9.84 | 8.68 | 9.40 | ||
| n | 30 | 14 | 44 | ||
| E | Mean | 55.36 | 55.68 | 55.51 | |
| SD | 13.85 | 11.18 | 12.59 | ||
| n | 33 | 28 | 61 | ||
| S | Mean | 60.94 | 64.03 | 62.24 | |
| SD | 11.22 | 10.25 | 10.92 | ||
| n | 435 | 316 | 751 | ||
| W | Mean | 57.66 | 65.38 | 61.86 | |
| SD | 12.15 | 11.24 | 12.24 | ||
| n | 62 | 74 | 136 | ||
| Country | Germany | Mean | 60.94 | 64.03 | 62.24 |
| SD | 11.22 | 10.25 | 10.92 | ||
| n | 435 | 316 | 751 | ||
| Asia (Multi-Center) | Mean | 60.61 | 62.21 | 61.26 | |
| SD | 13.78 | 11.57 | 12.92 | ||
| n | 112 | 77 | 189 | ||
| USA | Mean | 57.66 | 65.38 | 61.86 | |
| SD | 12.15 | 11.24 | 12.24 | ||
| n | 62 | 74 | 136 | ||
| Revascularization | no | Mean | 59.08 | 64.00 | 61.38 |
| SD | 11.93 | 10.71 | 11.63 | ||
| n | 441 | 386 | 827 | ||
| yes | Mean | 64.40 | 63.67 | 64.16 | |
| SD | 10.73 | 10.42 | 10.62 | ||
| n | 168 | 81 | 249 | ||
| Sex | female | Mean | 63.61 | 67.69 | 64.98 |
| SD | 11.27 | 9.62 | 10.90 | ||
| n | 259 | 131 | 390 | ||
| male | Mean | 58.28 | 62.49 | 60.34 | |
| SD | 11.77 | 10.69 | 11.44 | ||
| n | 350 | 336 | 686 | ||
| Total | Mean | 60.55 | 63.94 | 62.02 | |
| SD | 11.85 | 10.65 | 11.46 | ||
| n | 609 | 467 | 1,076 | ||
The area under the receiver operator curve (ROC) for the entire study population was calculated to be 0.881 (0.86-0.903).(Figure 2). The coordinates of the curve confirmed that a cut-off score of 4.0 provides the best combination of sensitivity and specificity for the prediction of relevant coronary stenosis from the MCG test that was reproducible throughout the participating centers.
Patients without a significant coronary stenosis had a severity score ≤ 4.0 more frequently than those with a relevant coronary stenosis by a wide margin (p <0.001). The results indicate that MCG showed a sensitivity of 91.2% and a specificity of 84.6% for the prediction of coronary stenosis. The Bayes Corrected positive predictive value (PPV) was 0.78, and the Bayes Corrected negative predictive value (NPV) was 0.94. A positive likelihood ratio of over 6 and a negative likelihood ratio of 0.1 indicate a good to strong diagnostic value for this test (table 4).
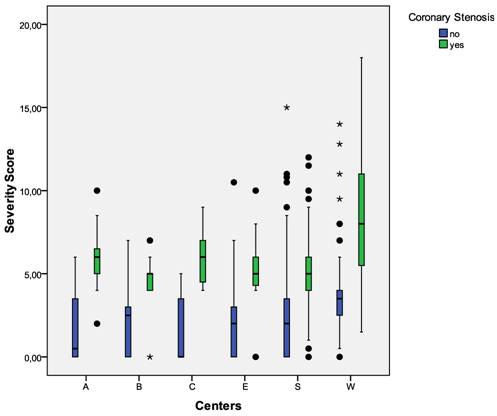
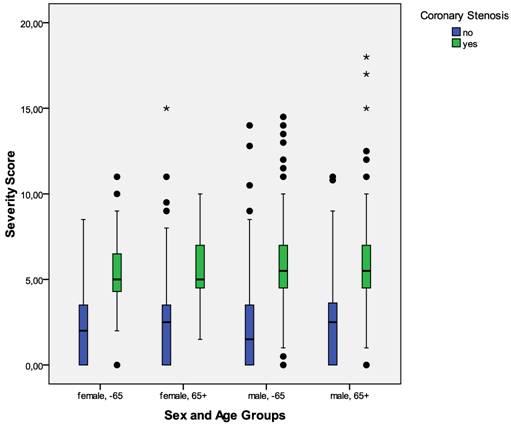
Sensitivity and specificity showed slight differences between participating centers, age, and gender groups, as well as between patients with and without revascularization procedures in their history. But for every group, sensitivity was always 90% or better and specificity better than 80% (detailed results in table 4), even for those in the revascularization group with a lower angiographic a priori pretest probability of 0.325, or women having ages equal or greater than 65 years old with the a priori pretest probability of only 0.388. Since there were only a small number (n=43) of women under the age of 65 in this cohort, the deviations may be considered as an epiphenomenon. From the most currently accumulated data (pending publication), the sensitivity and specificity for this group also falls between 90+% and 85+% respectively. The gender data in the trials for patients 65 years of age or older was also particularly noteworthy. For males and females 65 years old or older the sensitivity was 92% and 97% respectively, the specificity was 80% and 79% respectively, and the negative predictive values were 88% and 98% respectively. These results demonstrate a significant improvement in detection accuracy for hemodynamically relevant coronary stenosis in ≥ 65 year old females, a group that has heretofore been difficult to evaluate for obstructive coronary disease using existing ECG or stress imaging modalities.(Table 4.)
Summary Of Overall MCG Data For The Detection Of Relevant Coronary Stenosis. n = number of cases; TP = true positives; TN = true negatives; FP = false positives; FN = false negatives; a priori = a priori probability of stenosis; Correct = fraction of correctly predicted cases; Sens = sensitivity; Spec = specificity; PPV = positive predictive value; NPV = negative predictive value; LR+ = positive likelihood ratio; LR- = negative likelihood ratio; OR = odds ratio; ROC AUC = receiver operating curve area under the curve for continuous severity score; 95% CI = 95% confidence interval; Lower = Lower boundary of 95% CI; Upper = Upper boundary of 95% CI; NaN = not a number; Revasc = coronary revascularization in medical history.
| ROC AUC | Odds Ratio | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | TP | TN | FP | FN | Sens. | Spec. | PPV | NPV | Correct | a piori | ROC AUC | lower CI | upper CI | PPV (Bayes) | NPV (Bayes) | LR+ | LR- | Odds Ratio | lower CI | upper CI | |
| Combined Analysis | |||||||||||||||||||||
| Total | 1076 | 426 | 515 | 94 | 41 | 0.912 | 0.846 | 0.819 | 0.926 | 0.875 | 0.434 | 0.881 | 0.860 | 0.903 | 0.777 | 0.942 | 5.910 | 0.104 | 56.925 | 38.594 | 83.963 |
| USA | 136 | 72 | 45 | 17 | 2 | 0.973 | 0.726 | 0.809 | 0.957 | 0.860 | 0.544 | 0.886 | 0.825 | 0.946 | 0.835 | 0.950 | 3.548 | 0.037 | 95.294 | 21.014 | 432.131 |
| Asia | 189 | 73 | 97 | 15 | 4 | 0.948 | 0.866 | 0.784 | 0.971 | 0.899 | 0.407 | 0.914 | 0.868 | 0.961 | 0.770 | 0.972 | 7.079 | 0.060 | 118.017 | 37.594 | 370.482 |
| Germany | 751 | 281 | 373 | 62 | 35 | 0.889 | 0.857 | 0.819 | 0.914 | 0.871 | 0.421 | 0.873 | 0.846 | 0.900 | 0.767 | 0.936 | 6.239 | 0.129 | 48.301 | 31.034 | 75.175 |
| female | 390 | 121 | 221 | 38 | 10 | 0.924 | 0.853 | 0.761 | 0.957 | 0.877 | 0.336 | 0.885 | 0.849 | 0.920 | 0.617 | 0.978 | 6.296 | 0.089 | 70.371 | 33.878 | 146.172 |
| male | 686 | 305 | 294 | 56 | 31 | 0.908 | 0.840 | 0.845 | 0.905 | 0.873 | 0.490 | 0.881 | 0.853 | 0.908 | 0.839 | 0.908 | 5.673 | 0.110 | 51.653 | 32.377 | 82.405 |
| < 65 years | 623 | 216 | 332 | 47 | 28 | 0.885 | 0.876 | 0.821 | 0.922 | 0.880 | 0.392 | 0.892 | 0.865 | 0.920 | 0.747 | 0.948 | 7.138 | 0.131 | 54.492 | 33.108 | 89.688 |
| 65+ years | 453 | 210 | 183 | 47 | 13 | 0.942 | 0.796 | 0.817 | 0.934 | 0.868 | 0.492 | 0.858 | 0.821 | 0.896 | 0.812 | 0.936 | 4.608 | 0.073 | 62.897 | 32.987 | 119.926 |
| Female, < 65 years | 184 | 43 | 121 | 12 | 8 | 0.843 | 0.910 | 0.782 | 0.938 | 0.891 | 0.277 | 0.896 | 0.838 | 0.953 | 0.579 | 0.975 | 9.345 | 0.172 | 54.198 | 20.754 | 141.533 |
| Female, 65+ years | 206 | 78 | 100 | 26 | 2 | 0.975 | 0.794 | 0.750 | 0.980 | 0.864 | 0.388 | 0.857 | 0.803 | 0.911 | 0.656 | 0.987 | 4.725 | 0.032 | 150.000 | 34.545 | 651.330 |
| Male, < 65 years | 439 | 173 | 211 | 35 | 20 | 0.896 | 0.858 | 0.832 | 0.913 | 0.875 | 0.440 | 0.886 | 0.853 | 0.920 | 0.795 | 0.931 | 6.300 | 0.121 | 52.147 | 29.051 | 93.605 |
| Male, 65+ years | 247 | 132 | 83 | 21 | 11 | 0.923 | 0.798 | 0.863 | 0.883 | 0.870 | 0.579 | 0.865 | 0.814 | 0.915 | 0.896 | 0.846 | 4.571 | 0.096 | 47.429 | 21.754 | 103.407 |
| No Revasc | 827 | 351 | 367 | 74 | 35 | 0.909 | 0.832 | 0.826 | 0.913 | 0.868 | 0.467 | 0.873 | 0.847 | 0.899 | 0.806 | 0.923 | 5.419 | 0.109 | 49.736 | 32.423 | 76.295 |
| PCI | 188 | 47 | 120 | 15 | 6 | 0.887 | 0.889 | 0.758 | 0.952 | 0.888 | 0.282 | 0.894 | 0.841 | 0.947 | 0.552 | 0.981 | 7.981 | 0.127 | 62.667 | 22.938 | 171.205 |
| CABG | 61 | 28 | 28 | 5 | 0 | 1.000 | 0.848 | 0.848 | 1.000 | 0.918 | 0.459 | 0.902 | 0.814 | 0.989 | 0.826 | 1.000 | 6.600 | 0.000 | NaN | NaN | NaN |
| Revasc of any type | 249 | 75 | 148 | 20 | 6 | 0.926 | 0.881 | 0.789 | 0.961 | 0.896 | 0.325 | 0.902 | 0.860 | 0.944 | 0.644 | 0.981 | 7.778 | 0.084 | 92.500 | 35.642 | 240.058 |
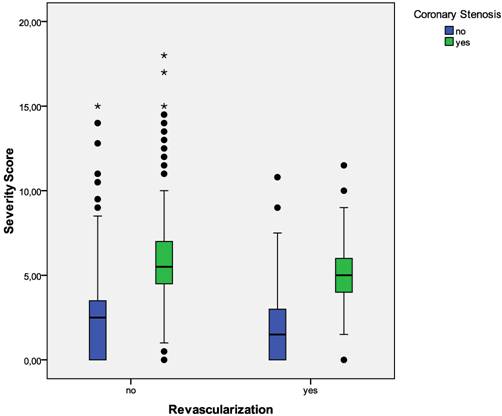
Figure 1 is a boxplot of MCG severity scores versus the documented presence or absence of relevant coronary stenosis by coronary angiography. Note the clear separation of the mean and median scores in the two groups (p < .01). Figure 3 is a boxplot of MCG severity scores from all participating centers separated by whether or not the score was associated with the finding of relevant coronary stenosis on coronary angiography. Again note the clear separation of the scores identifying patients with and without coronary stenosis. Figure 4 shows the boxplot of MCG severity scores by sex and age groups and Figure 5 shows the boxplot of the MCG severity score data from patients with and without prior revascularization. Please note that in all these boxplots and the sub-groups they depict, the MCG cut-off score of 4.0 appears to clearly identify the populations within the study population that have critical coronary stenosis.
Severity Score Versus Coronary Stenosis In The Entire Study Population. Boxplots of MCG severity scores in all patients with and without relevant coronary stenosis. The boundaries of the box are Tukey's hinges. The median is identified by the line inside the box. The length of the box is the interquartile range (IQR) computed from Tukey's hinges. Values more than three IQR's from the end of a box are labeled as extreme, denoted with an asterisk (*). Values more than 1.5 IQR's but less than 3 IQR's from the end of the box are labeled as outliers (•). Whiskers show high/low values. Outliers and Extremes were included in the overall statistical analysis because the assumptions about the distribution of the data (normal distribution) were not violated.
ROC For The Entire Study Population Using A Cut-Off MCG Score of 4.0. Area Under The Curve Was 0.881 (0.860 - 0.903).
Severity Score Versus Coronary Stenosis In The Entire Study Population By Individual Center. Boxplots of MCG severity scores in patients with and without relevant coronary stenosis from the individual centers included in the meta-analysis. The boundaries of the box are Tukey's hinges. The median is identified by the line inside the box. The length of the box is the interquartile range (IQR) computed from Tukey's hinges. Values more than three IQR's from the end of a box are labeled as extreme, denoted with an asterisk (*). Values more than 1.5 IQR's but less than 3 IQR's from the end of the box are labeled as outliers (•). Whiskers show high/low values. Outliers and Extremes were included in the overall statistical analysis because the assumptions about the distribution of the data (normal distribution) were not violated.
Severity Score Versus Coronary Stenosis In The Entire Study Population By Sex And Age Groups. Boxplots of MCG severity scores in patients with and without relevant coronary stenosis according to sex and age groups. The boundaries of the box are Tukey's hinges. The median is identified by the line inside the box. The length of the box is the interquartile range (IQR) computed from Tukey's hinges. Values more than three IQR's from the end of a box are labeled as extreme, denoted with an asterisk (*). Values more than 1.5 IQR's but less than 3 IQR's from the end of the box are labeled as outliers (•). Whiskers show high/low values. Outliers and Extremes were included in the overall statistical analysis because the assumptions about the distribution of the data (normal distribution) were not violated.
Severity Score Versus Coronary Stenosis In The Entire Study Population According To Whether Patients Had Prior Revascularization Or Not. Boxplots of MCG severity scores in patients with and without relevant coronary stenosis according to whether the patients had prior revascularization. The boundaries of the box are Tukey's hinges. The median is identified by the line inside the box. The length of the box is the interquartile range (IQR) computed from Tukey's hinges. Values more than three IQR's from the end of a box are labeled as extreme, denoted with an asterisk (*). Values more than 1.5 IQR's but less than 3 IQR's from the end of the box are labeled as outliers (•). Whiskers show high/low values. Outliers and Extremes were included in the overall statistical analysis because the assumptions about the distribution of the data (normal distribution) were not violated.
Discussion
The overall sensitivity of 91% and specificity of 85% of the MCG device in this meta-analysis further confirms the strength of this device to identify relevant coronary stenosis (>70%) in a population with a demonstrated pre-test risk of disease from 27.7% to 43.4%. Subjects included in the trial were ambulatory patients who presented to their physicians for evaluation. Physicians used tools commonly at their disposal, including the available stress ECG modalities, to decide whether to refer the patient for coronary angiography, and had no knowledge the patient was a candidate for or would be included in an MCG study. The specific intent of the studies included in this meta-analysis was not to study MCG as a screening device, but instead to focus primarily on its potential as a diagnostic assay for relevant coronary stenosis.
Resting ECG analysis, including 12-lead ECG, typically has significantly less sensitivity in detecting ischemia or obstructive coronary disease in patients with a low pre-test risk of disease. Clinical studies report a wide range for sensitivity from 20% to 70% for acute myocardial infarction (AMI) (review in [4]) and less for hemodynamically significant CAD ischemia [25]. Diagnostic yield from a resting ECG can be improved by exercise testing. Whereas exercise ECG has a reported specificity of over 80% under ideal conditions, in routine clinical use the sensitivity utilizing exercise-based ECG is typically not better than 50-60% [6, 26, 27, 28].
Performance of exercise ECG testing can be further enhanced by multivariate analysis of ECG and clinical variables. First studies into computerized, multivariate exercise ECG analysis showed good to excellent sensitivity in men and women (83% and 70%, respectively) and specificity (93%, 89%) [29, 30]. These results were confirmed by a second group of researchers [31] and are similar to our findings with MCG. Other researchers used different statistical approaches and models of multivariate stress ECG analysis with different sets of variables included in the models [32, 33, 34, 35]. Although these approaches provided significantly better diagnostic performance than did standard exercise ECG testing, it appears that none of these methods has been implemented in broad clinical practice or a commercial product. It should also be noted that none of the above referenced studies included patients with previous coronary revascularization.
Stress echocardiography performed by experienced investigators may provide better sensitivity and specificity than does stress ECG. Numerous studies into exercise echocardiography as a diagnostic tool for CAD have been done. Reported sensitivities range from 31% to over 90% and specificities from 46% to nearly 100% [36, 37, 38]. With experienced investigators, sensitivities of over 70% and specificities better than 85% can be expected.
In a comprehensive systematic review of 16 prospective studies, myocardial perfusion scintigraphy showed better positive and negative likelihood ratios than did routine exercise ECG testing [39]. However, wide variation between studies was reported with positive LR ranging from 0.95 to 8.77 and negative LR from 1.12 to 0.09. Another review of stress scintigraphy studies showed similar results, with a diagnostic accuracy of 85% but wide variation between studies (sensitivity 44%-89%, specificity 89%-94% for 2+ vessel disease) [40]. In one study, the combination of stress ECG testing with myocardial scintigraphy using multivariate analysis provided only limited improvement of diagnostic accuracy [41].
Whereas the reported diagnostic performance of stress echocardiography, myocardial scintigraphy, and stress scintigraphy are not dissimilar to what we found for MCG, imaging modalities can provide additional information such as spatial localization that a resting ECG method cannot.
MCG's sensitivity and specificity for the detection of coronary stenosis was good to excellent in all patient groups included in this meta-analysis, with only moderate differences between groups. Moreover, there were only small differences in the results between the different centers. The optimal cut-off for the device-determined severity score was not different between patient groups or medical centers. These results indicate that MCG generates reproducible and stable results in diverse patient populations and different medical settings. Although the number of patients with a revascularization procedure in their medical history was small, the findings may further indicate that MCG provides reliable results in this patient group where other ECG or stress modalities often perform unsatisfactorily [9, 10, 11].
The endpoint of this study was the morphologic diagnosis of CAD on coronary angiography, whereas the investigated electro-physiologic method (MCG) assesses functional changes of electro-myocardial function secondary to changes in coronary blood flow, including both local and global forms of ischemia. Therefore, even under ideal conditions, a 100% coincidence between angiographic findings and MCG results could not be expected. The disagreements mainly stem from under- or over-estimation of disease severity by MCG or the angiographer. Technicians' misidentifying poor quality tests as “acceptable” for MCG interpretation is a source for potential discordance of MCG data and angiographic data. Finally, microvascular disease, not associated with definable epicardial vessel lesions on angiography, resulting in myocardial ischemia can create a false positive result, and critical stenosis of an epicardial vessel with a well-established collateral circulation resulting in a reduction of myocardial ischemia may result in a false negative result. Clinical correlation of MCG data will always be required by the treating physician.
Resting and stress ECG analyses in CAD patients primarily focus on time-dependent ST-segment analysis and the detection of other abnormalities, such as Q-wave abnormalities, Q-T interval, etc. This is not comparable to the MCG concepts and technology, which performs a coronary disease/ischemia assessment from a complex mathematical analysis performed in both the frequency and the time domains.
One limitation of the present study was that the angiographic results were not explicitly quantified using a suitable scoring system such as the BARI (bypass angioplasty revascularization investigation) system in all studies [42]. Still, the assessment of coronary lesions in the present study was consistent between two experienced US based angiographers who independently evaluated the angiograms. As the target criterion was hemodynamically relevant coronary stenosis (>70%), implying an indication for therapeutic intervention, borderline lesions may have been classified as non-relevant. This may have further artificially reduced the calculated specificity of the MCG method.
Another limitation may have been the recruitment of patients. The patient population in all studies included in the meta-analysis represented a convenience sample of patients from a larger group of consecutive patients scheduled for coronary angiography in the respective centers. Although this may limit the generalizability of the patient sample employed herein, the demographic distribution of this sample matches very well with the distributions reported in the literature for patients with CAD. In addition, ~57% of all the participants, and in particular ~67% of revascularization group, ~72% of women under the age of 65, and ~61% of women ≥ 65 did not have hemodynamically significant CAD, with MCG severity scores ranging from completely normal (0.0-0.5) to less than 4.0. Therefore, it appears justified to assume that the study findings from the investigated patient group are valid for a general population of CAD patients.
MCG performed very well in the group who had either prior PCI or prior CABG (Table 4). Despite the fact that in 188 patients with a prior PCI history there was a low a priori pre-test risk of coronary stenosis of 28%, MCG correctly identified 89% of these patients as either having relevant stenosis or not. If the MCG score was below 4.0 in this group, the negative predictive value of the test was 95.2%. In the 61 patients with a history of prior CABG, the a priori pre-test risk of coronary stenosis was 46%. In this group, MCG correctly identified 92% as either having relevant stenosis or not, and if the score was below 4.0, the negative predictive value of the MCG test was 100%. These impressive findings suggest a role for MCG testing in the evaluation of disease progression or restenosis after revascularization. Further studies will need to be done pre- and post- revascularization to confirm this data.
Finally, MCG was compared to angiography, but not directly to any other non-invasive diagnostic technology in the studies included in this meta-analysis. Therefore, inference about the potential superiority or inferiority of MCG compared to other ECG-based methods can only be drawn indirectly from other studies. But even with this important caveat, the data presented in this study on sensitivity and specificity of MCG for the detection of relevant CAD is considerably better than the published sensitivity, specificity, and negative predictive value of the most widely used stress ECG-based methods, including combined stress imaging techniques. Additionally, the reported sensitivity, specificity, and negative predictive value of 97%, 79%, and 98% respectively, for females 65 years of age or older is superior to published data for stress ECG and stress perfusion or wall motion imaging [6-8]. This presents a significant improvement in detection accuracy for hemodynamically relevant coronary stenosis in Medicare age females when the results are indirectly compared with other ECG or imaging stress diagnostic modalities. In addition, the MCG analysis servers and methodology are available 24/7/365 to provide an objective, affordable, accurate, safe, and immediately accessible diagnosis on the Internet for patients in a wide variety of care settings including EMS, Urgent Care Facilities, Emergency Rooms, and in- or out-patient clinics/hospitals. The use of the MCG in clinical practice has been reliably extended to monitor the progression or the development of ischemia and the improvement of ischemia after interventional and/or optimized medical therapies. Future research will also include direct comparisons between MCG and other commonly used or new non-invasive or invasive diagnostic and monitoring methods.
In conclusion, the multi-functional mathematical systems analysis of the resting ECG in the frequency and time domains done using the MCG device appears to provide a high sensitivity and specificity for the identification of relevant CAD, as diagnosed by coronary angiography, in patients with a low or high pre-test risk of coronary disease, that appears to be equal to or better than those of any other resting or stress ECG/imaging methods currently used in clinical practice.
Conflict of Interest
With the exception of Joseph T. Shen, MD, the developer of the MCG technology and founder of Premier Heart, LLC, the authors have declared that no conflict of interest exists.
References
1. OECD. OECD Health Data 2005: Statistics and Indicators for 30 Countries. Paris: OECD Publishing. 2005
2. Mackay J, Mensah G. Atlas of Heart Disease and Stroke. Geneva: WHO Press. 2004
3. Thom T, Haase N, Rosamond W, et al.; American Heart Association Statistics Committee, Stroke Statistics Subcommittee. Heart disease and stroke statistics--2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85-e151
4. Ammar KA, Kors JA, Yawn BP, Rodeheffer RJ. Defining unrecognized myocardial infarction: a call for standardized electrocardiographic diagnostic criteria. Am Heart J. 2004;148:277-284
5. Salerno SM, Alguire PC, Waxman HS. Competency in interpretation of 12-lead electrocardiograms: a summary and appraisal of published evidence. Ann Intern Med. 2003;138:751-760
6. Tak T, Gutierrez R. Comparing stress testing methods. Available techniques and their use in CAD evaluation. Postgrad Med. 2004;115:61-70
7. Gibbons RJ, Balady GJ, Beasley JW. et al. ACC/AHA Guidelines for Exercise Testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). J Am Coll Cardiol. 1997;30:260-311
8. Gibbons RJ, Balady GJ, Bricker JT. et al. ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002;106:1883-1892
9. Hecht HS, Shaw RE, Chin HL. et al. Silent ischemia after coronary angioplasty: evaluation of restenosis and extent of ischemia in asymptomatic patients by tomographic thallium-201 exercise imaging and comparison with symptomatic patients. J Am Coll Cardiol. 1991;17:670-677
10. Pirelli S, Danzi GB, Alberti A. et al. Comparison of usefulness of high-dose dipyridamole echocardiography and exercise electrocardiography for detection of asymptomatic restenosis after coronary angioplasty. Am J Cardiol. 1991;67:1335-1338
11. Schroeder E, Marchandise B, De Coster P. et al. Detection of restenosis after coronary angioplasty for single-vessel disease: how reliable are exercise electrocardiography and scintigraphy in asymptomatic patients? Eur Heart J. 1989;10(Suppl G):18-21
12. Braunwald E, Antman EM, Beasley JW. et al. ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction--2002: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). Circulation. 2002;106:1893-1900
13. Gibbons RJ, Abrams J, Chatterjee K. et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients with Chronic Stable Angina). J Am Coll Cardiol. 2003;41:159-168
14. Mason JJ, Owens DK, Harris RA. et al. The role of coronary angiography and coronary revascularization before noncardiac vascular surgery. JAMA. 1995;273:1919-1925
15. Scanlon PJ, Faxon DP, Audet AM. et al. ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation. 1999;99:2345-2357
16. Budoff MJ, Achenbach S, Duerinckx A. Clinical utility of computed tomography and magnetic resonance techniques for noninvasive coronary angiography. J Am Coll Cardiol. 2003;42:1867-1878
17. Traversi E, Bertoli G, Barazzoni G. et al. Non-invasive coronary angiography with multislice computed tomography. Technology, methods, preliminary experience and prospects. Ital Heart J. 2004;5:89-98
18. Hurst JW. Current status of clinical electrocardiography with suggestions for the improvement of the interpretive process. Am J Cardiol. 2003;92:1072-1079
19. Eskola MJ, Nikus KC, Voipio-Pulkki LM. et al. Comparative accuracy of manual versus computerized electrocardiographic measurement of J-, ST- and T-wave deviations in patients with acute coronary syndrome. Am J Cardiol. 2005;96:1584-1588
20. Feng G. EKG and EEG Multiphase Information Analysis (A collection of unpublished notes, thesis, papers and published articles from mid seventies to the late eighties translated into English from Chinese), First Edition. USA: American Medical Publishers. 1992
21. Weiss MB, Narasimhadevara SM, Feng GQ, Shen JT. Computer-enhanced frequency-domain and 12-lead electrocardiography accurately detect abnormalities consistent with obstructive and nonobstructive coronary artery disease. Heart Dis. 2002;4:2-12
22. Grube E, Bootsveld A, Yuecel S. et al. Computerized two-lead resting ECG analysis for the detection of coronary artery stenosis. Int J Med Sci. 2007;7:249-263
23. Altman DG, Bland JM. Diagnostic tests 2: Predictive values. BMJ. 1994;309:102
24. Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ. 2004;329:168-169
25. Mant J, McManus RJ, Oakes RA. et al. Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care. Health Technol Assess. 2004;8:1-158
26. Anthony D. Diagnosis and screening of coronary artery disease. Prim Care. 2005;32:931-946
27. Cox JL, Teskey RJ, Lalonde LD, Iles SE. Noninvasive testing in women presenting with chest pain: evidence for diagnostic uncertainty. Can J Cardiol. 1995;11:885-890
28. Curzen N, Patel D, Clarke D, ete al. Women with chest pain: is exercise testing worthwhile? Heart. 1996;76:156-160
29. Detry JM, Robert A, Luwaert RJ. et al. Diagnostic value of computerized exercise testing in men without previous myocardial infarction. A multivariate, compartmental and probabilistic approach. Eur Heart J. 1985;6:227-238
30. Robert AR, Melin JA, Detry JM. Logistic discriminant analysis improves diagnostic accuracy of exercise testing for coronary artery disease in women. Circulation. 1991;83:1202-1209
31. Deckers JW, Rensing BJ, Tijssen JG. et al. A comparison of methods of analysing exercise tests for diagnosis of coronary artery disease. Br Heart J. 1989;62:438-444
32. Koide Y, Yotsukura M, Yoshino H, Ishikawa K. A new coronary artery disease index of treadmill exercise electrocardiograms based on the step-up diagnostic method. Am J Cardiol. 2001;87:142-147
33. Lehtinen R, Sievänen H, Uusitalo A. et al. Performance characteristics of various exercise ECG classifiers in different clinical populations. J Electrocardiol. 1994;27:11-22
34. Pruvost P, Lablanche JM, Beuscart R. et al. Enhanced efficacy of computerized exercise test by multivariate analysis for the diagnosis of coronary artery disease. A study of 558 men without previous myocardial infarction. Eur Heart J. 1987;8:1287-1294
35. Rodriguez M, Moussa I, Froning J. et al. Improved exercise test accuracy using discriminant function analysis and "recovery ST slope". J Electrocardiol. 1993;26:207-218
36. Geleijnse ML, Krenning BJ, Soliman OI. et al. Dobutamine stress echocardiography for the detection of coronary artery disease in women. Am J Cardiol. 2007;99:714-717
37. Marwick TH, Shaw L, Case C. et al. Clinical and economic impact of exercise electrocardiography and exercise echocardiography in clinical practice. Eur Heart J. 2003;24:1153-1163
38. Smart SC, Bhatia A, Hellman R. et al. Dobutamine-atropine stress echocardiography and dipyridamole sestamibi scintigraphy for the detection of coronary artery disease: limitations and concordance. J Am Coll Cardiol. 2000;36:1265-1273
39. Mowatt G, Vale L, Brazzelli M. et al. Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction. Health Technol Assess. 2004;8:1-207
40. Elhendy A, Bax JJ, Poldermans D. Dobutamine stress myocardial perfusion imaging in coronary artery disease. J Nucl Med. 2002;43:1634-1646
41. Morise AP, Diamond GA, Detrano R, Bobbio M. Incremental value of exercise electrocardiography and thallium-201 testing in men and women for the presence and extent of coronary artery disease. Am Heart J. 1995;130:267-276
42. Alderman E, Stadius M. The angiographic definitions of the bypass angioplasty re-vascularization investigation. Coron Artery Dis. 1992;3:1189-1207
43. Sekhri N, Feder GS, Junghans C. et al. Incremental prognostic value of the exercise electrocardiogram in the initial assessment of patients with suspected angina: cohort study. BMJ. 2008;337:a2240
Author contact
![]() Correspondence to: John E. Strobeck, MD, PhD, Director, Heart Failure Program, The Valley Hospital, Ridgewood, NJ 07450.
Correspondence to: John E. Strobeck, MD, PhD, Director, Heart Failure Program, The Valley Hospital, Ridgewood, NJ 07450.

 Global reach, higher impact
Global reach, higher impact