3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2009; 6(3):137-138. doi:10.7150/ijms.6.137 This issue Cite
Short Communication
Optical Coherence Tomography in ocular toxoplasmosis
Centre Cochin Ambulatoire d'Ophtalmologie - Hôpital Cochin, Paris (France)
Published 2009-3-19
Optical Coherence Tomography (OCT) is now a method of choice to asses conditions such as macular holes, diabetic macular edema or central serous chorioretinopathy [1]. OCT measurements of retinal thickness have a good reproducibility as demonstrated in repeated examinations. The main application of OCT in inflammatory eye diseases is for the analysis of cystoid macular edema [2;3].
Ocular toxoplasmosis is the most frequent cause of posterior segment inflammation. [4]. Twenty-five consecutive patients seen in a single referral center between November 2003 and August 2004 were studied. Presumed ocular toxoplasmosis was diagnosed based on the clinical appearance of retinochoroiditis and a positive serology. Lesions were presumed to be active in the presence of whitish edematous areas.[5] Fluorescein angiography was performed in active cases. Lesions were presumed to be scarred when pigmented and/or atrophic. Areas of retinochoroiditis were further analyzed by the Zeiss OCT3 imager (Humphrey-Zeiss, San Leandro, California, USA). Two perpendicular scans centered on the lesion were performed. The length of scans was 3 or 6 mm, according to the size of the lesion. The vitreoretinal interface was analyzed and measures of retinal thickness were performed.
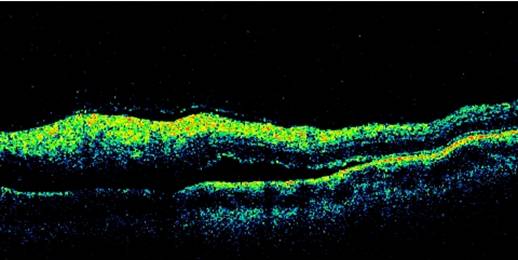
Fourteen men and 11 women were included. The mean age was 25.5 ± 9.9 years. Fifteen patients (60%) had had a previous episode of retinochoroiditis. Active lesions were observed in 16 subjects and scarred lesions in 9 subjects. Active areas appeared as hyperreflective images, which were localized in the retina in 15 cases and in the choroid in 1 case. Partial posterior vitreous detachment with a localized vitritis contiguous to the site of active retinochoroiditis, was observed in 13 cases. Sub-retinal fluid was detected by OCT in 3 cases, but was present on fluorescein angiograms only in 2 of these cases (Figure 1). Scarred areas were characterized by retinal atrophy. The mean retinal thickness at the center of active lesions was 353 ± 98 µm (range 184 - 614 µm), compared to 135 ± 95 µm (range 0 - 338 µm) for scarred lesions (p<0.001).
OCT is safe, non invasive and devoided of any side effects, therefore follow-up measurements are unlimited, while fluorescein angiography is invasive and it carries some risks and side effects in certain subjects. Active toxoplasmic lesions have shown 3 main OCT characteritics:
- A highly reflective intraretinal area corresponding with the area of retinitis.
- A posterior hyaloid thickened and detached over the lesion and contained irregular hyperreflective formation.
- A shadow effect of the underlying choroidal tissue.
Reliable measurements of retinal thickness by OCT may be impossible in the presence of severe vitritis. Fluorescein angiograms remain very useful for the assessment of vasculitis and blood-retinal barrier breakdowns, whereas OCT detects sub-retinal fluid with a higher sensitivity.
We have shown that OCT imaging can distinguish between active and scarred toxoplasmic lesions. OCT provides quantitative measurements of retinal thickness, which could be useful in future prospective studies, to guide therapeutic decisions and to monitor the efficacy of treatments.
Optical Coherence Tomography in ocular toxoplasmosis
References
1. Puliafito CA, Hee MR, Lin CP. et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995;102:217-29
2. Antcliff RJ, Stanford MR, Chauhan DS. et al. Comparison between optical coherence tomography and fundus fluorescein angiography for the detection of cystoid macular edema in patients with uveitis. Ophthalmology. 2000;107:593-9
3. Hassenstein A, Bialasiewicz AA, Richard G. Optical coherence tomography in uveitis patients. Am J Ophthalmol. 2000;130:669-70
4. Smit RL, Baarsma GS, de Vries J. Classification of 750 consecutive uveitis patients in the Rotterdam Eye Hospital. Int Ophthalmol. 1993;17:71-6
5. Bosch-Driessen LE, Berendschot TT, Ongkosuwito JV, Rothova A. Ocular toxoplasmosis: clinical features and prognosis of 154 patients. Ophthalmology. 2002;109:869-78

 Global reach, higher impact
Global reach, higher impact