3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2009; 6(3):114-115. doi:10.7150/ijms.6.114 This issue Cite
Short Communication
Ocular Manifestations of West Nile Virus Infection
Department of Ophthalmology, Fattouma Bourguiba University Hospital, Monastir (Tunisia)
Published 2009-5-26
West Nile Virus (WNV), first isolated in 1937 in the West Nile district of Uganda, is a single-stranded RNA flavivirus. It is a member of the Japanese encephalitis serogroup. WNV infection is a zoonotic disease transmitted by a mosquito vector (type Culex), with wild birds serving as its reservoir. The disease is endemic in Europe, Australia, Asia, Africa, and North and Central America since its appearance in New York in 1999.1
Most human infections are subclinical (80%) or manifest as febrile illness (20%). Severe neurologic disease (meningoencephalitis), frequently associated with advanced age and diabetes, was initially reported to occur in less than 1% of patients. However, over time, WNV infection has increased in severity. The diagnosis is confirmed by detection of IgM antibody in serum or cerebrospinal fluid.1
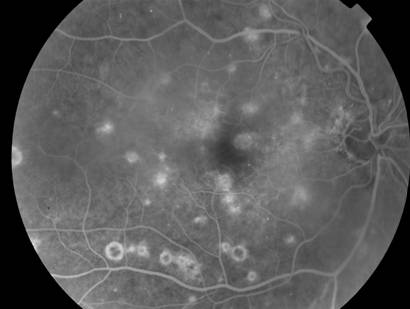
A typical multifocal chorioretinitis, frequently asymptomatic, is the most common ocular manifestation of WNV infection (80%).2 Active chorioretinal lesions appear as circular, deep, creamy lesions on ophthalmoscopy, with early hyopofluorescence and late staining on fluorescein angiography (FA). Inactive chorioretinal lesions typically are partially atrophic and partially pigmented with a “targetlike appearance”: central hypofluorescence and peripheral hyperfluorescence on FA (Figure 1). Chorioretinal lesions vary in number and size, involving the midperiphery, with or without involvement of the posterior pole. Linear clustering of chorioretinal lesions, following the course of retinal nerve fibers, is a prominent feature (> 80%). Indocyanine green angiography shows more lesions, in the form of hypofluorescent spots, than those appreciated clinically or by FA.
Other ocular manifestations of WNV infection include anterior uveitis, retinal vasculitis, optic neuritis, subconjunctival hemorrhage, sixth nerve palsy, nystagmus, and congenital chorioretinal scarring.2,3
Ocular disease usually has a self-limited course, and visual acuity returns to baseline in most patients. However, persistent visual loss may occur due to foveal chorioretinal scar, choroidal neovascularization, vitreous hemorrhage, tractional retinal detachment, severe ischemic maculopathy, optic atrophy, and retrogeniculate damage.
Midphase fluorescein angiogram of a 64-year-old diabetic woman with a 20-day history of fever and headache shows chorioretinal lesions with central hypofluorescence and peripheral hyperfluorescence. Note the presence of mild non-proliferative diabetic retinopathy.
There is no proven treatment for WNV infection. In cases of severe disease, therapy is supportive, with hospitalization, intravenous fluids, respiratory support, and prevention of secondary infection.
Prevention is the mainstay of WNV infection control, with public health measures to reduce the number of mosquitos (draining standing water, larvicides…) and personal protection against mosquito bites (repellants, window screens, protective clothing,…). Vaccination, a long term solution, is still in the research phase.
In conclusion, chorioretinal involvement, frequently asymptomatic and self-limited, is present in almost 80% of patients with WNV infection associated with neurologic disease. The unique pattern of multifocal chorioretinitis can help establish an early diagnosis of the disease while serologic testing is pending. Therefore, an ocular examination, including ophthalmoscopy and FA in selected cases, should be part of the routine evaluation of patients with clinically suspected WNV infection.
References
1. Hayes EB, Gubler DJ. West Nile virus: epidemiology and clinical features of an emerging epidemic in the United States. Annu Rev Med. 2006;57:181-94
2. Khairallah M, Ben Yahia S, Ladjimi A. et al. Chorioretinal involvement in patients with West Nile virus infection. Ophthalmology. 2004;111:2065-70
3. Garg S, Jampol LM. Systemic and intraocular manifestations of West Nile virus infection. Surv Ophthalmol. 2005;50:3-13

 Global reach, higher impact
Global reach, higher impact