3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2009; 6(2):106-110. doi:10.7150/ijms.6.106 This issue Cite
Research Paper
Clinical Symptoms Associated with Asystolic or Bradycardic Responses on Implantable Loop Recorder Monitoring in Patients with Recurrent Syncope
Department of Medicine, University of Toledo Medical Center, Toledo OH 43614, USA
Received 2009-2-16; Accepted 2009-4-8; Published 2009-4-9
Abstract
Background: Implantable loop recorders (ILR) have been found to be useful in the diagnosis and management of syncope of unclear etiology. The clinical symptoms of abnormalities seen during ILR monitoring have not been adequately studied.
Aim: The aim of this retrospective study was to determine the clinical symptoms which were the best predictors of asystolic or bradycardic responses during ILR monitoring.
Methods: Patients with either asystole or bradycardia recorded during ILR monitoring were analyzed from our database. The clinical characteristics of these patients were compared to the patients with ILR's who did not have recorded bradycardic episodes. The episodes were characterized as being convulsive or nonconvulsive, brief (<5 minutes) or prolonged (> 5 minutes), and having had a prodrome or no prodrome.
Results: Eleven patients (4 males and 7 females; age 39 ±11years) had asystole or bradycardia on ILR monitoring. Eleven patients (2 males and 9 females; age 46±23) had no bradycardiac events. Palpitations, convulsive syncope, prolonged episode, and prodrome were present in 37% vs. 74% (P = 0.125), 62% vs. 0% (P = 0.002), 87% vs. 0% (P=0), and 73% vs. 13% (P=0.009) patients, respectively, in the asystole/bradycardia and non-bradycardia groups. In the asystole/bradycardia group eight patients had bradycardia (HR < 20) for > 10 seconds and three patients had asystole >10 seconds.
Conclusion: Convulsive syncope, prolonged loss of consciousness during syncopal episode, and absence of prodrome or aura are clinical predictors of asystole or bradycardia on ILR monitoring.
Keywords: Implantable loop recorders, bradycardia, asystole, convulsions.
Introduction
Ambulatory cardiac monitoring with Holter or external loop recorders is frequently employed in the evaluation of patients with recurrent syncope. However, several non-randomized studies demonstrate a relatively low (<40%) diagnostic yield from this approach [1-5]. Implantable loop recorders (ILR's), by contrast, allow for a more prolonged period of monitoring as well as automatic activation during events, resulting in a higher diagnostic yield than traditional monitoring techniques [6-12]. During ILR monitoring of patients with recurrent syncope, bradycardic events are encountered more frequently than are tachycardiac ones [13-15]. The clinical symptoms most predictive of significant bradycardic events (such as prolonged sinus pauses or complete heart block) recorded during ILR monitoring have not been well reported. The aim of the present study was to identify the clinical characteristics and symptoms obtained from patient histories that best correlate with significant bradycardic events recorded during ILR monitoring.
Methods
The study was a retrospective analysis which was approved by the University of Toledo Institutional Review Board. A comprehensive review of patient charts was performed to identify patients of unexplained syncope who had received ILR and had asystolic (>10 second pause) or bradycardic (< 20 beats per minute) response corresponding to syncopal event during ILR monitoring.
Inclusion criterion
We queried our data base of implanted loop recorders. We identified 150 patients who received ILR over a period of 8 years for evaluation of unexplained nature of their syncope. Out of these 150 patients only 14 had either a bradycardic (n=11) or a tachycardiac response (n=3) recorded on ILR during episodes of syncope. Patients were included in the study if they had either syncope or symptoms during monitoring which resembled the index syncope episode that lead to evaluation. Patients included in the study had undergone an extensive evaluation including head up tilt test, cardiac electrophysiology study and 24 hour holter monitor and 1 month event recorder prior to implantation of ILR. Another 8 patients who had received loop implants during the same time frame and had no arrhythmia recorded during an episode of the syncope were also include to make groups comparable. These patients were followed for a period of 9±3 months after rhythm directed therapy for recurrence of any syncope.
The information about the clinical symptoms was obtained from patient charts and physician letters. The clinical symptoms which were obtained from these sources included
- Presence of Aura: Aura included subjective nature of symptoms like lightheadedness, dizziness feeling of passing out. It was considered present or absent if the patient had aura during the episode of syncope (while being on ILR monitoring) and resembled the index episode.
- Duration of syncope: The duration of syncope was determined from the loss of consciousness to full recovery of consciousness. The duration also included the postictal confusion if it was a convulsive syncope. We defined episodes of loss of consciousness as prolonged if they were > 5 minutes. The estimate of duration of loss of consciousness was obtained from the people witnessing the event
- Convulsive Syncope. Syncopal episodes were labeled as convulsive if the patients had convulsions during the episodes. These convulsions were myoclonic in nature and were witnessed by family members or friends. None of our patients had loss of bladder or bowel controls during these episodes.
- Palpitations: Patient histories were reviewed for presence or absence of palpitation immediately prior to syncope. Due to the specific nature of palpitations this symptom was not included in the aura.
Statistics
All statistical analyses were done using SPSS. The continuous data was presented as mean ±SD and categorical data as percentages. T-test for comparison of means and chi-square test for categorical data was used. Significance was achieved with P value < 0.05.
Results
Total of 22 patients of refractory syncope were included in this study. These patients had suffered from recurrent episodes of syncope (> 2 in 6 months). All of these patients had a negative work-up including head up tilt test (HUTT), 24 hour holter, 30 day event monitor and cardiac electrophysiology studies. Some of these patients had undergone stress and coronary angiography as well as electroencephalography and CT scan. All the evaluations turned out to be inconclusive. In view of negative initial inconclusive work-up patients received implantable loop recorders. The average duration of monitoring with an ILR was 6 months.
The baseline clinical characteristics of patients with asystolic or bradycardic responses during ILR monitoring (Group 1) are compared with those without asystolic or bradycardic responses (Group 2) in Table 1. Eleven patients (4 males and 7 females; age 39 ±11) had asystole or bradycardia on ILR monitoring. Eight patients had bradycardia (HR < 20) for > 10 seconds and 3 patients had asystole >10 seconds in group 1.
Eleven patients in group 2 (2 males and 9 females; age 46±23) had either tachycardia (n=3) or a sinus rhythm (n-8) recorded during an episode syncope.
One patent with tachycardia in Group 2 had Ventricular Tachycardia (HR > 140) and episodes of atrial fibrillation (HR 180). Two patients had atrioventricular re-entrant tachycardia with HR (200).
These episodes of arrhythmias either tachycardia or bradycardia were associated either with syncope during ILR monitoring.
Baseline clinical characteristics in two groups of patients
| Clinical Characteristics | Group1 (N=11) | Group 2 (N=11) | P |
|---|---|---|---|
| Age | 39±11 | 46±23 | NS |
| Race (Caucasian)% | 90 | 94 | NS |
| Male: Female | 4:7 | 2:9 | NS |
| Symptoms | |||
| Palpitations % | 37 | 74 | 0.125 |
| Convulsive syncope % | 62 | 0 | 0.002 |
| Episode > 5 min. % | 87 | 0 | 0.001 |
| Prodrome % | 13 | 73 | 0.009 |
Group 1= Patients with asystolic or bradycardic response on ILR monitoring.
Group 2= Patients without asystolic or bradycardic response on ILR monitoring.
Symptoms (Table 1 and Figure 1)
- Aura or prodrome: Only thirteen percent of patients in group1 had aura or warning signs before syncope compared to 73% in group 2 (p=0.01).
- Duration: Eighty seven percent of patients in group 1 had prolonged episode compared to none in group 2 (p=0.0001).
- Palpitations: Thirty seven percent of patients in group 1 had palpitations compared to 74% in group 2 (p=0.12).
- Convulsive Syncope. Convulsive syncope was seen in 62% of patients in group1 and none in group 2 (p=0.002).
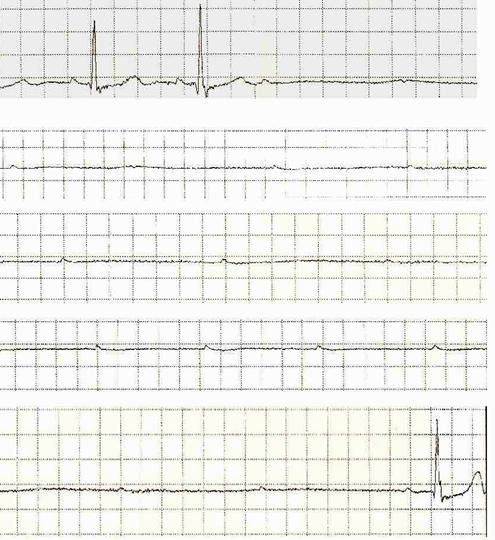
Age, gender, and race were similar in the two groups. In this study, fourteen patients had positive testing on ILR monitoring. In group 1, eight patients had bradycardia (HR < 20) for > 10 seconds and three patients had asystole >10 seconds. One of the patients had a 44-second sinus pause on ILR monitoring (Fig 2). Dual chamber pacemaker was placed in all eleven patients in group 1 in view of either asystole or complete AV block recorded on ILR during a syncopal episode. Two patients in group 2 who were noted to have supraventricular tachycardia underwent radiofrequency ablation therapy. The patient with ventricular tachycardia and atrial fibrillation received an implantable cardioverter defibrillator as well as medical management for paroxysmal atrial fibrillation. Following rhythm directed therapy, none of these patients had any further episodes of syncope over 6±3 months.
Clinical presentation of patients in different groups.
Recording downloaded from loop recorder showing prolonged Ventricular asystole and profound AV block. (44 second).
Discussion
Unexplained syncope can pose a unique diagnostic challenge for physicians especially when the initial workup such as HUTT, electrophysiology studies, 24 hour holter monitor or 30 day event recorder is inconclusive. Implantable loop recorders have been shown to improve diagnosis and, thus facilitate rhythm directed therapy in this subgroup of patients [3-16]. In our study of 22 patients, 14 had an arrhythmic etiology. Eleven patients had bradyarrhythmia on ILR monitoring.
Our study is unique as the clinical symptoms of the syncope in patients with bradyarrhythmic responses (the most common arrhythmia that has been reported during prolonged monitoring with ILR) have not been studied to date. It is interesting that abrupt onset (lack of prodrome), convulsive activity, and prolonged episodes of loss of consciousness were significantly associated with bradycardic responses during ILR monitoring. Interestingly, some of the patients in our study were labeled as having psychogenic syncope for years before the ILR monitoring revealed the diagnosis. The result of the recurrent and unpredictable nature of these syncopal episodes can result in a marked reduction in the quality of life in many of these patients [17].
Syncope can sometimes be confused with seizures. Some studies have reported that 30-42% of patients who were initially diagnosed with epilepsy had syncope with convulsive activity due cardiovascular etiology [20, 21, 22]. The pathophysiology of syncope provoked convulsive activity is complex. Asystole and sinus pauses in our patients were long enough to result in severe hypotension and cerebral hypoxia, which in turn could have lead to convulsive activity. Engel et al [23] reported seizure-like activity following periods of cerebral hypoxia. It has also been reported that in episodes of syncope associated with convulsive activity, the duration of loss of consciousness tends to be longer, as is the time to full recovery. In our study, these episodes lasted more than 5 min from onset to full return of consciousness (including postictal confusion period). In addition, all our patients who had a bradycardic/asystolic response on ILR monitoring had abrupt onset of syncope with no prodrome or aura, which predisposed them to suffer trauma from an episode. Sud et al [24] in their recent report of predicting cause of syncope from clinical histories found that syncope occurring without aura or prodrome is associated with spontaneous arrhythmic etiology predominantly bradycardia.
Given a small number of patients in our study population and retrospective nature of the study an adequately powered prospective study is needed to validate these results, nevertheless the results of our study are consistent with those of other studies [13-15,23,24].
In our study, ILR monitoring by guiding rhythm directed therapy in all patients who tested positive helped prevent further syncope. None of the patients has yet had recurrence of their syncope following definitive treatment.
Limitation
This study was retrospective in nature and followed a small number of patients. The information about the clinical symptoms was obtained from patient charts and physician letters. There was no questionnaire used to assess the symptoms. Another limitation of the study was a recall bias on the part of family members or friends witnessing these episodes. The study included only patients with unexplained syncope and thus the results can not be generalized.
Conclusion
In the group of patients with recurrent unexplained syncope, severe bradycardia/asystole was the most common positive finding recorded during ILR monitoring. The clinical symptoms that were found to have the consistent association with severe bradycardia and asystole include lack of prodrome, convulsive activity and prolonged loss of consciousness.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Kapoor WN. Evaluation and outcome of patients with syncope. JAMA. 1990;69:160-175
2. Soteriades ES, Evans JC, Larson MG. et al. Incidence and prognosis of syncope. N Engl J Med. 2002;347:878-885
3. Sarasin FP, Louis-Simonet M, Carlballo D. et al. Prospective evaluation of patients with syncope: a population based study. Am J Med. 2001;111:177-184
4. Linzer M, Yang EH, Estes NA. Diagnosing syncope. Part 2: Unexplained syncope. Clinical efficacy assessment project of the American college of physicians. Ann Intern Med. 1990;150:1073-1078
5. Gibson TC, Heitzman MR. Diagnostic efficacy of 24 hour electrocardiographic monitoring for syncope. Am J cardiol. 1984;53:1013-1017
6. Linzer M, Pritchet EL, Pontinen M. Incremental diagnostic yield of loop electrocardiographic recorders in unexplained syncope. Am J of Cardiol. 1990;66:214-219
7. Cumbee SR, Pryor RE, Linzer M. Cardiac loop ECG recording: a new non-invasive diagnostic test in recurrent syncope. South Med J. 1990;83:39-43
8. Brown AP, Dawkins KD, Davies JG. Detection of arrhythmia. Use of patient activated ambulatory electrocardiogram device with a solid state memory loop. Br Heart J. 1987;58:251-253
9. Zimetbaum P, Kime KY, Ho KK. Utility of patient activated cardiac event recorders in general clinical practice. Am J Cardiol. 1997;79:1-372
10. Krahn AD, Klein GJ, Yee R, Hoch JS, Skanes AC. Cost Implication of Testing strategy in patients with syncope. Randomized Assessment of Syncope Trial. J Am Coll Cardiol. 2003;42:495-501
11. Schuchert A, Maas R, Kretzschmar C, Behrens G, Kratzman I, Meinertz T. Diagnostic yield of external electrocardiographic loop recorders in patients with recurrent syncope and negative Tilt table test. PACE. 2003;26:1837-1840
12. Farwell DJ, Freemantle N, Sulke AN. Use of implantable loop recorders in the diagnosis and management of Syncope. European Heart Journal. 2004;25:1257-1263
13. Moya A, Brignole M, Mennozi C. et al. Mechanism of syncope in patients with isolated syncope and in patients with tilt positive syncope. Circulation. 2001;104:1261-1267
14. Brignole M, Mennozi C, Moya A. et al. Mechanism of syncope in patients with bundle branch block and negative electrophysiological tests. Circulation. 2001;104:2045-2050
15. Inamdar V, Mehta S, Juang G, Cohen T. The utility of implantable loop recorders for diagnosing unexplained syncope in 100 consecutive patients - Five year, Single Center Experience. J invasive cardiol. 2006;18(7):313-315
16. Menozzi C, Bringole M, Garcia -Civera R. Mechanism of syncope in patients with heart disease and negative electrophysiologic test. Circulation. 2002;105:2741-2745
17. Grubb BP. The impact of syncope and transient loss of consciousness on quality of life. Benditt D, Bringole M, Raviele A, Wieling W, eds. Malden MA: Blackwell- futura Publishing. 2007:148-152
18. Frangini PA, Cecchin F, Jordao L, Martuscello M, Alexander ME, Triedman JK, Walsh EP. et al. How Revealing Are Insertable Loop Recorders in Pediatrics? PACE. 2008;31(3):338-343
19. Giada F, Gulizia M, Francese M, Croci F, Santangelo L, Santomauro M, Occhetta E, Mennozi C, Raviele A. Recurrent unexplained palpitations (RUP) study. J Am Coll Cardiol. 2007;49(19):1951-6
20. Gastaut H, Gastaut Y. Electroencephalographic and clinical study of anoxic convulsions in children: their location within the group of infantile convulsions and their differentiation from epilepsy. Electroencephalogr clin Neurophysiol. 1958;10:815-835
21. Zaidi A, Clough P, Cooper P. Misdiagnosis of epilepsy: Many seizures like episodes have cardiovascular cause. J Am Coll Cardiol. 2000;36:181-184
22. Zaidi A, Clough P, Marwer G. et al. Accurate diagnosis of convulsive syncope: Role of implantable subcutaneous ECG monitoring. Seizure. 1999;8:184-186
23. Engel J. Differential diagnosis of seizures. In: (ed.) Engel JJr. Seizures and epilepsy. Philadelphia: FA Davis Co. 1998:340-1
24. Sud S, Klein GJ, Skanes AC, Gula LJ, Yee R, Krahn AD. Predicting the cause of syncope from clinical history in patients undergoing prolonged monitoring. Heart Rhythm. 2009;6(2):238-43
Author contact
![]() Correspondence to: Blair P Grubb, MD, Director Electrophysiology Services, Division of Cardiology, Department of Medicine, Health Sciences Campus, University of Toledo Medical Center, Mail Stop 1118, 3000 Arlington Ave, Toledo OH 43614, USA
Correspondence to: Blair P Grubb, MD, Director Electrophysiology Services, Division of Cardiology, Department of Medicine, Health Sciences Campus, University of Toledo Medical Center, Mail Stop 1118, 3000 Arlington Ave, Toledo OH 43614, USA

 Global reach, higher impact
Global reach, higher impact