3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2010; 7(6):342-353. doi:10.7150/ijms.7.342 This issue Cite
Research Paper
Refractive Status and Prevalence of Refractive Errors in Suburban School-age Children
1. Department of Ophthalmology, Children's Hospital, Chongqing Medical University, Chongqing, People's Republic of China
2. Southwest Hospital, Southwest Eye Hospital, The Third Military Medical University, Chongqing, People's Republic of China
Received 2010-9-12; Accepted 2010-10-15; Published 2010-10-18
Abstract
Objective: This study investigated the distribution pattern of refractive status and prevalence of refractive errors in school-age children in Western China to determine the possible environmental factors. Methods: A random sampling strategy in geographically defined clusters was used to identify children aged 6-15 years in Yongchuan, a socio-economically representative area in Western China. We carried out a door-to-door survey and actual eye examinations, including visual acuity measurements, stereopsis examination, anterior segment and eyeball movements, fundus examinations, and cycloplegic retinoscopy with 1% cyclopentolate. Results: A total of 3469 children living in 2552 households were selected, and 3070 were examined. The distributions of refractive status were positively-skewed for 6-8-year-olds, and negatively-skewed for 9-12 and 13-15-year-olds. The prevalence of hyperopia (≥+2.00 D spherical equivalent [SE]), myopia (≤-0.50 D SE), and astigmatism (≥1.00 diopter of cylinder [DC]) were 3.26%, 13.75%, and 3.75%, respectively. As children's ages increased, the prevalence rate of hyperopia decreased (P<0.001) and that of myopia increased significantly (P<0.001). Children in academically challenging schools had a higher risk of myopia (P<0.001) and astigmatism (≥1.00DC, P =0.04) than those in regular schools. Conclusion: The distribution of refractive status changes gradually from positively-skewed to negatively-skewed distributions as age increases, with 9-year-old being the critical age for the changes. Environmental factors and study intensity influence the occurrence and development of myopia.
Keywords: refractive error, suburban school-age children, myopia
INTRODUCTION
Childhood visual impairment due to refractive errors is one of the most common problems among school-age children and is the second leading cause for treatable blindness [1]. Vision 2020: The Right to Sight, a global initiative launched by a coalition of non-government organizations and the World Health Organization (WHO) [2], is to eliminate avoidable visual impairment and blindness on a global scale. In China, the problem of uncorrected refractive error is particularly common [3], and the refractive errors have become one of the leading causes for visual impairment and blindness, especially among children [4]. In order to reduce the occurrence of avoidable visual impairment and blindness caused by refractive errors, there is an urgent need for obtaining the epidemiological information on refractive errors and other eye diseases among school-age children.
There are several epidemiological reports on refractive errors in school-age children from the Asia-Pacific region and many other countries, such as Singapore [5], South Korea [6], Japan [7], China [8, 9, 10], Nepal [11], Malaysia [12], India [13, 14], and Chile [15]. The prevalence rates of refractive errors in these areas are different from the results of epidemiological studies from China [8, 9, 10] and the prevalence of myopia is higher in China, indicating that differences in ethnicity, regional and economical differences and development levels could affect the prevalence of refractive errors. For instance, It has been demonstrated that different ethnic groups show different prevalence rates of refractive errors [16].
Although there are some reports in this research field from China, the subjects are mainly children attending schools or patients seen in eye clinics [17], which may not be representative of all school-age children. Furthermore, the majority of the reported population-based epidemiological researches on eye diseases among school-age children [8, 9, 10] are conducted in regions near the national capital or in developed coastal metropolis, which may not be fully representative of the whole China, especially the developing regions.
Western China is very vast (6.8 million square kilometers, accounting for 71% of the area in mainland China), and includes eleven provinces and one municipality, but the population is relatively sparse (360 million, accounting for only 28% of the total China population) [18]. Compared to other regions in China, this area is relatively less developed. Because of the relatively low standard of living and low level of social economical development, there is not enough attention paid to children's vision and refractions in Western China.
In order to obtain the refractive status in school-age children in Western China, we selected Yongchuan District, Chongqing, a representative district in Western China, as the study site for our population-based research. The focus of our research was to determine the environmental factors on the prevalence of refractive errors within a single ethnicity. We also compared the prevalence rates of refractive errors in academically challenging schools with those in regular schools to determine the effects of academic demands (study load) among these children on their vision and eye health. Additionally, with a comparison with previous reports [8, 9, 10], our results may provide a basis for establishing effective strategies for the prevention and treatment of refractive errors among school-age children in China.
MATERIALS AND METHODS
Sample Selection
A cross-sectional study was conducted in Yongchuan District, one of the 40 administrative districts in Chongqing City. Chongqing city, with a registered population of 30.51 million (2000 Census), is considered an economic and cultural center of Western China [19]. Yongchuan District was chosen for this study because it had a relatively stable population (-0.97% annual average growth rate from the 2000 Census), with its socioeconomic status being ranked middle in Western China and most residents in this district being Han Chinese.
In this study, clusters were defined by geographical residential areas, called residence administrative community (RACs) and villages. Those RACs and villages with large populations were further divided and those with small populations were combined to create clusters with estimated 100 to 150 eligible children each. The calculation of sample size was based on preliminary studies carried out from September 6, 2006 to October 7, 2006, in which 324 aged 6-15 year-old children were randomly selected. The prevalence of refractive errors was 20%. The level of significance was set at 5% (two-tailed), and the tolerable error (type B error) was set at 1.5%. The sample size for this study was calculated as follows: n≈Z2(ρ)(1-ρ)/B2, where ρ=0.2, B=0.015, and Z=1.96 for a 95% confidence interval; and the error bound was 7.5%. After adjusting for an anticipated 10% nonparticipation rate, the sample size was determined to be 3,005 [20]. Among the 78 clusters that met the study criteria, 28 were randomly selected for the study, including 6 from urban areas, 13 from rural areas, and 9 from suburban areas; in the latter regions approximately 1/3 of people were registered as urban residents and the remaining 2/3 as rural residents. It was estimated that 3469 eligible children were living in the 28 clusters, exceeding the required sample size of 3005.
The inclusion criteria were the following: 1) actual age was 6-15-years old on the examination day; 2) parents or legal guardians signed an informed consent; and 3) there was no history of systematic cardiovascular or nervous diseases, such as congenital heart diseases, hypoxic-ischemic encephalopathy, and learning difficulties. The exclusion criteria were the following: 1) Children who had eye injuries or eye diseases (e.g., corneal opacities, cataracts, fundus pathology, etc) that affected visual functions; 2) children who had a history of untreated closed-angle glaucoma or untreated anatomically narrow angles - information obtained from anterior segment examination and medical history; 3) children who were allergic to any ingredient in 1% cyclopentolate solution; 4) children who refused to continue the examinations due to eye discomfort during cyclopentolate administration (e.g., burning, photophobia, irritation); and 5) children who moved eyeballs excessively during examination.
Field Survey
According to the 2000 Census, households with eligible children were chosen based on resident address. Children aged 6-15 years having lived in census-identified households for at least six months were selected. Those who were selected but temporarily absent from the area at the time of selection were also included. During door-to-door selection interviews, a parent or legal guardian of the child was informed of the study details, including the side effects of pupillary dilation and cycloplegia and the assigned time for eye examination. Parents who had expressed hesitancy or reluctance to participate in this study were invited to a seminar for further information on the study. The study only included children whose parents or legal guardians signed the consent form. The selection process was completed in one month, from August 8, 2006 to September 5, 2006. Human subject research approval for the study protocol was obtained from WHO's Secretariat Committee on Research Involving Human Subjects. The study protocol was also approved by the local ethics committee. The protocol adhered to the provisions of the Declaration of Helsinki for research. The Bureau of Education and Bureau of Health in Yongchuan District approved the implementation of this study.
Eye Examination
Eye examinations were performed by a medical team consisting of three ophthalmic nurses, two ophthalmologists, and one optometrist, between October 8, 2006 and January 1, 2007. Examination included an assessment of visual acuity, stereopsis, and ocular motility. A slit lamp assessment of the anterior segment and a dilated fundus examination was also performed.
The examination process began with testing visual acuity at 4 m using ETDRS LogMAR visual acuity chart (Precision Vision, La Salle, IL) [21]. After testing stereopsis with digital stereograms, the ophthalmologist evaluated the anterior segment with a slit lamp and ocular motility was assessed using a pen torch. Both pupils were then dilated with two drops of 1% cyclopentolate at five minute intervals, and the pupillary light reflex was checked 20 min later. If the pupillary light reflex was still present, a third drop was administered. Light reflex and pupil dilation were evaluated an additional 15 min. Cycloplegia was considered complete if the pupil was dilated to 6 mm or more and the light reflex was absent. After the fundus examination was performed with a direct ophthalmoscope (YZ6E; Six Six Vision Corp., Suzhou, China), refraction was performed with a streak retinoscope (YZ24; Six Six Vision Corp., Suzhou, China). Because the examination was carried out in the winter, photophobia after mydriasis was not obvious. All the examined children did not have assigned homework on the examination day, avoiding the difficulties in reading and writing caused by ciliary muscle paralysis. Children with refractive errors without correction were referred to a local eye hospital for further diagnosis and treatment.
Data Management and Analysis
Household selection and clinical examination data were reviewed for accuracy and completeness before the computer-aided data entry. Refraction of astigmatism was expressed by SE (SE = sphere + 0.5 × cylinder). The refraction distributions of all age groups were expressed as mean ± standard deviation (SD) and median values of diopter for both eyes. Since the refraction distributions of left eyes and right eyes were similar (Pearson coefficient = 0.90) and the data from left eyes had fewer outliers, only the data from left eyes were presented in this report. The distributions of refractive status were further analyzed by dividing the children into three age groups: 6-8-year-old (Grades 1-3), 9-12-year-old (Grades 4-6), and 13-15-year-old (Grades 7-9). The division was based on different learning stages. One-way analysis of variance (ANOVA) and least significant difference (LSD) multiple comparisons were carried out to test significance of the differences between diopter means of different age groups. P<0.05 was considered statistically significant. Furthermore, Kolmogoroy-Smirnov (KS) tests were utilized to perform the normal distribution tests for the refractive distributions of every age as well as every age group.
Children were considered hyperopic (defined as ≥+1.50 D SE or ≥+2.00 D SE) if one or both eyes were hyperopic; myopic (defined as ≤-0.50 D SE) if one or both eyes were myopic; astigmatism (defined as cylinder powers ≥0.50 DC or ≥1.00 DC) if one or both eyes were astigmatism. Astigmatism was further analyzed by dividing the subjects into three types: hyperopic astigmatism (simple hyperopic astigmatism and compound hyperopic astigmatism), myopic astigmatism (simple myopic astigmatism and compound myopic astigmatism), and mixed astigmatism. Confidence intervals for the prevalence estimates were calculated. All data were statistically analyzed with a SPSS software program (SPSS for Windows, Rel.13.0.0.2004; SPSS, Chicago, IL). Chi-square tests were applied to compare the prevalence of hyperopia, myopia, and astigmatism among different groups. When outcome variables (had refractive error or not) were used in logistic regression, we analyzed the factors such as age, gender and school type affecting the prevalence of refractive errors.
Quality Assurance
All investigators and staff involved in this research participated in an intensive two-day training. Demographic data were collected by qualified nurses. During a complete examination, the tested children went through six separate stations: visual acuity assessment, stereopsis, anterior segment and eye movement examinations, eye drop instillation, cycloplegic retinoscopy, and fundus examination. The quality of examination for each station was controlled by the leading investigators. Because a senior investigator was assigned for the quality control for each of the six stations and every station's record was produced independently, this research procedure minimized possible systematic biases that could be present when only one person performed multiple tests or multiple people performed one test.
RESULTS
Characteristics of the Study Population
The randomly selected 28 clusters included 3611 households, of which 2552 households (70.67%) had a total of 3469 children aged 6-15 years. Among the 2552 households, 1713 (67.12%) had one child and 839 (32.88%) had two or more children. Among the 3469 children, 399 children were excluded from the study for various reasons: 197 refused to participate in the eye examinations, nine had potential risks for cycloplegia, 36 had eye discomforts, 86 had other pathological conditions (systematic diseases such as congenital brain diseases and cardiovascular diseases), 63 were unable to continue the examination due to non-cooperation, and eight had unclear fundus reflexes in eyes with corneal or media opacities. Finally, 3070 children (88.50%) met the study criteria, including 1611 boys (52.48%) and 1459 girls (47.52%), with the gender ratio (M:F) being 1.1:1.0. Girls had a better response rate (90.56%) than boys (86.71%). The average age was 10.41 ± 2.73 years old. Table 1 shows the demographic makeup of the study population. The 324 children from the pilot study were also included in the 3070 children.
Refraction distribution
Refractions of both eyes for all the 3070 children were examined with cycloplegic dilation. The mean refraction was 0.47±1.20 D SE in left eyes. Table 2 shows the detailed information of SE values in left eyes. From 6-year-old to 15-year-old, the SE means displayed a decreasing trend from +1.36 D to -0.14 D SE, but the rate of decrease was not constant. The refraction medians also displayed a decreasing trend as age increased; refractions for 6-year-old children had a median of +1.25 D SE, and refractions for 15-year-old children had a median of +0.25 D SE. These results indicated that as age increases, more children have negative SE values.
Age and sex distribution of the selected and examined population
| Age | NO.(%) of All | NO. (%) of Boys | NO. (%) of Girls | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Selected | Examined | %Exam | Selected | Examined | %Exam | Selected | Examined | %Exam | |
| 6 | 300(8.65) | 239(7.79) | 79.67 | 177(9.53) | 139(8.63) | 78.53 | 123(7.64) | 100(6.85) | 81.30 |
| 7 | 362(10.44) | 313(10.20) | 86.46 | 195(10.50) | 169(10.49) | 86.67 | 167(10.37) | 144(9.87) | 86.23 |
| 8 | 369(10.64) | 339(11.04) | 91.87 | 170(9.15) | 156(9.68) | 91.76 | 199(12.35) | 183(12.54) | 91.96 |
| 9 | 378(10.90) | 350(11.40) | 92.59 | 196(10.55) | 180(11.17) | 91.84 | 182(11.30) | 170(11.65) | 93.41 |
| 10 | 373(10.75) | 341(11.12) | 91.42 | 166(8.93) | 154(9.56) | 92.77 | 207(12.85) | 187(12.82) | 90.34 |
| 11 | 349(10.06) | 319(10.39) | 91.40 | 200(10.76) | 180(11.17) | 90.00 | 149(9.25) | 139(9.53) | 93.29 |
| 12 | 358(10.32) | 305(9.93) | 85.20 | 197(10.60) | 167(10.37) | 84.77 | 161(10.00) | 138(9.46) | 85.71 |
| 13 | 325(9.37) | 285(9.28) | 87.69 | 181(9.74) | 156(9.68) | 86.19 | 144(8.94) | 129(8.84) | 89.58 |
| 14 | 379(10.93) | 354(11.53) | 93.40 | 207(11.14) | 187(11.61) | 90.34 | 172(10.68) | 167(11.45) | 97.09 |
| 15 | 276(7.96) | 225(7.33) | 81.52 | 169(9.10) | 123(7.64) | 72.78 | 107(6.64) | 102(6.99) | 95.33 |
| All | 3469(100.0) | 3070(100.0) | 88.50 | 1858(100.0) | 1611(100.0) | 86.71 | 1611(100.0) | 1459(100.0) | 90.56 |
Descriptive statistics (Mean, Median, SD, Range, Kurtosis and Skewness) of SE diopter in left eyes
| Age(yrs) | Mean* | Median | SD | Range | Kolmogorov-Smirnov test | Kurtosis | Skewness | ||
|---|---|---|---|---|---|---|---|---|---|
| z-statistic | P-value | ||||||||
| Total | 0.47 | 0.75 | 1.20 | -10.00~8.13 | 11.116 | <0.001 | 10.68 | -1.80 | |
| 6 | 1.36a | 1.25 | 0.58 | -0.50~4.38 | 3.011 | <0.001 | 9.29 | 1.92 | |
| 7 | 1.22b | 1.25 | 0.77 | -3.25~8.13 | 3.808 | <0.001 | 27.48 | 1.52 | |
| 8 | 0.94c | 1.00 | 0.95 | -4.00~6.25 | 3.898 | <0.001 | 12.91 | -0.43 | |
| 9 | 0.66d | 0.75 | 0.87 | -4.38 ~3.25 | 3.785 | <0.001 | 10.06 | -2.34 | |
| 10 | 0.56d | 0.75 | 1.04 | -10.00~5.00 | 4.391 | <0.001 | 34.37 | -3.84 | |
| 11 | 0.21e | 0.50 | 1.11 | -8.50~2.50 | 4.299 | <0.001 | 17.58 | -3.26 | |
| 12 | 0.13ef | 0.37 | 1.06 | -5.38~5.50 | 3.793 | <0.001 | 6.46 | -1.43 | |
| 13 | -0.00f | 0.37 | 1.30 | -7.50~6.00 | 4.524 | <0.001 | 11.15 | -2.32 | |
| 14 | -0.23g | 0.25 | 1.52 | -8.00~8.00 | 4.843 | <0.001 | 6.40 | -1.36 | |
| 15 | -0.14g | 0.25 | 1.21 | -5.13~3.50 | 3.641 | <0.001 | 2.90 | -1.36 | |
| 6-8 | 1.15 | 1.25 | 0.82 | -4.00~8.13 | 5.639 | <0.001 | 17.65 | 0.15 | |
| 9-12 | 0.41 | 0.62 | 1.05 | -10.00~5.50 | 7.238 | <0.001 | 16.81 | -2.67 | |
| 13-15 | -0.13 | 0.25 | 1.38 | -8.00~8.00 | 7.717 | <0.001 | 7.21 | -1.64 | |
* Means in the same column with different letters (a, b, c, d, e, f, g) were significantly different (P<0.05, ANOVA, LSD).
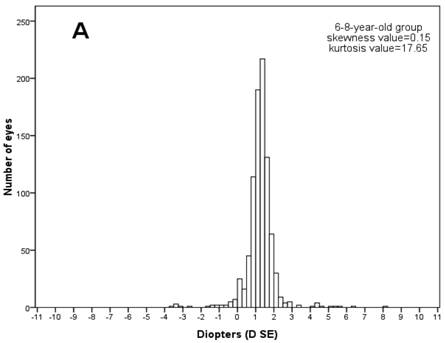
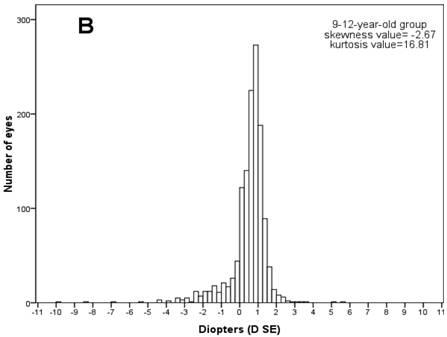
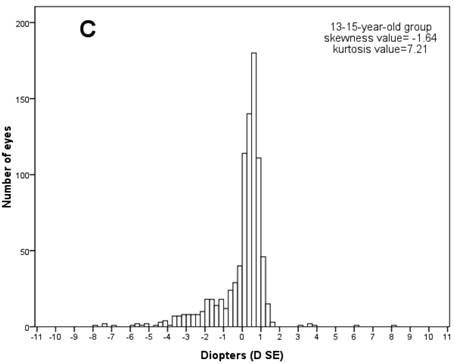
Then the frequency distributions of the refractive status for children at various ages were studied. The normal distribution tests showed that every age's refractive distribution was abnormal (Kolmogorov-Smirnov test, P<0.001). Figure 1 shows the frequency distribution of SE refraction in the three age groups. Every age group's frequency distribution clearly showed a SE peak. In the 6-8-year-old group, the SE varied from -4.00 to +8.13 D and peaked between +1.25 D and +1.50 D (24.50 % of the children in the group). In the 9-12-year-old group, the SE varied from -10.00 to +5.50 and peaked between +0.75 D and +1.00 (20.80%). In the 13-15-year-old group, the SE varied from -8.00 to +8.00 D and peaked between +0.50 D and +0.75 D (20.80%). The refractive frequency distributions for ages 6-8 were positively-skewed (skewness=0.15), but the frequency distributions for ages 9-12 (skewness= -2.67) and 13-15 (skewness=-1.64) showed negatively skewed due to increased myopia in the two groups.
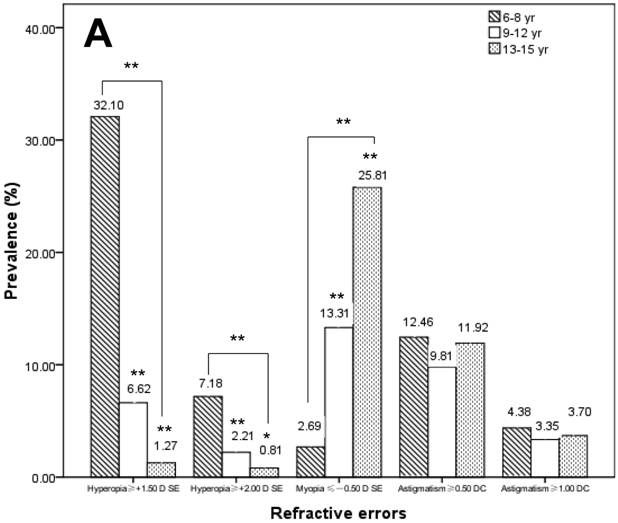
Prevalence of refractive errors
Table 3 shows the prevalence of hyperopia, myopia, and astigmatism at different ages. Among the 3070 children, 384 (12.51%) had hyperopia if the ≥ +1.50 D SE standard was used or 100 (3.26%) had hyperopia if the ≥ +2.00 D SE standard was used; 422 (13.75%) had myopia (≤ -0.5 D SE); 343 (11.17%) had astigmatism if the ≥ 0.50 DC standard was used or 115 (3.75%) had astigmatism if the ≥1.00 DC standard was used. These results demonstrated that age had a significant influence on the prevalence of hyperopia and myopia: as age increased, the prevalence of hyperopia markedly decreased, and that of myopia significantly increased. The prevalence of hyperopia was 48.12% (≥ +1.50 D SE) and 9.21% (≥ +2.00 D SE) among 6-year-olds. The prevalence of hyperopia was significantly decreased to 1.33% (≥ +1.50 D SE, χ2=133.762, P<0.001) and 0.89% (≥ +2.00 D SE, χ2=16.341, P<0.001) among 15-year-olds. Furthermore, the prevalence of myopia significantly increased from 0.42% to 27.11% from 6 to 15-year-olds (χ2=71.329, P<0.001). Figure 2A shows the prevalence of refractive errors in different groups.
Age did not significantly affect the prevalence of astigmatism (≥ 0.50 DC, χ2=11.548, P=0.24; ≥ 1.00 DC, χ2=8.806, P=0.46). The prevalence of astigmatism was 11.30% (≥ 0.50 DC) and 4.18% (≥ 1.00 DC) in 6-year-olds, and 14.22% (≥ 0.50 DC) and 4.89% (≥ 1.00 DC) in 15-year-olds.
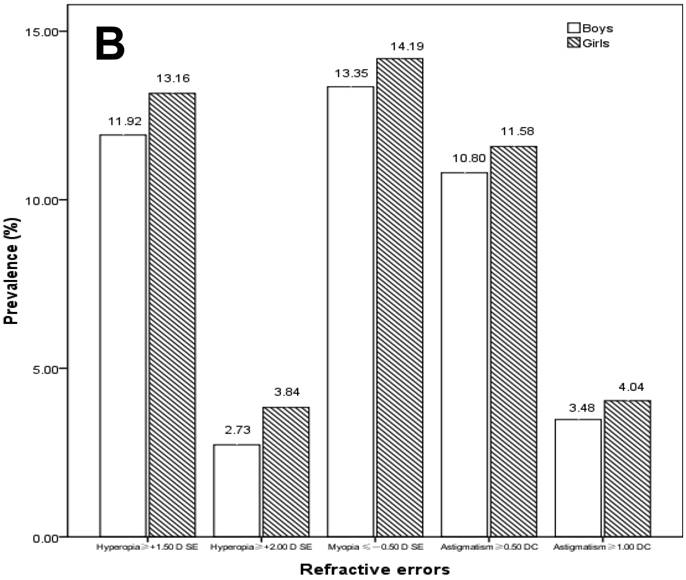
Gender did not significantly affect the prevalence rates of hyperopia (≥ +1.50 D SE, χ2=1.079, P=0.30; ≥ +2.00 D SE, χ2=2.977, P=0.08), myopia (χ2=0.458, P=0.50), and astigmatism (≥ 0.50 DC, χ2=0.472, P=0.49; ≥ 1.00 DC, χ2=0.684, P=0.41), although girls had slightly higher prevalence of refractive errors than boys (Figure 2B).
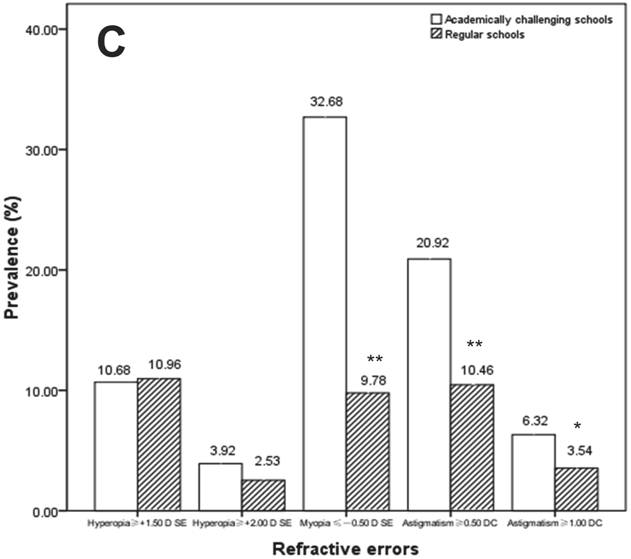
The prevalence of hyperopia (≥ +1.50 D SE, χ2=0.02, P=0.88; ≥ +2.00 D SE, χ2=1.65, p=0.20) did not differ between children in academically challenging schools and those in regular schools. The prevalence of myopia and astigmatism among children in academically challenging schools, however, were significantly higher than that in regular schools. The prevalence of myopia in academically challenging schools and regular schools were 32.68% and 9.78% (χ2=85.53, P<0.001), respectively. The prevalence of astigmatism (≥ 1.00 DC) in academically challenging schools and regular schools were 6.32% and 3.54% (χ2=4.41, P=0.04), respectively (Figure 2C).
Frequency histograms of spherical equivalent diopter data for (A) children in 6-8-year-old group (n=891), (B) 9-12-year-old group (n=1315), and (C) 13-15-year-old group (n=864). Values on the x-axis represent spherical equivalent diopter. The interval of each column is 0.25 D. Data were from the left eyes of 3070 school-age children.
X-axis represents different definition criteria for hyperopia, myopia, and astigmatism. (A) Prevalence of refractive errors by age groups (6-8, 9-12, and 13-15 years old). For the prevalence with the 6-8, 9-12 and 13-15 years old, means with ** were significantly different (P<0.001, chi-square test); and means with * were significantly different (P<0.05, chi-square test). (B) Prevalence of refractive errors by gender. (C) Prevalence of refractive errors by school type (academically challenging schools and regular schools). For the prevalence with the academically challenging schools and regular schools, means with ** were significantly different (P<0.001, chi-square test); and means with * were significantly different (P<0.05, chi-square test).
Prevalence of refractive errors versus age
| Age (yrs) | Hyperopia* (%) | Myopia† (%) | Astigmatism‡ (%) | ||
|---|---|---|---|---|---|
| ≥ +1.50 D SE | ≥ +2.00 D SE | ≤ -0.50 D SE | ≥ 0.50 DC | ≥ 1.00 DC | |
| 6 | 48.12(41.79-54.45)§ | 9.21(5.54-12.88) | 0.42(0-1.24) | 11.30(7.29-15.31) | 4.18(1.64-6.72) |
| 7 | 36.42(31.09-41.75) | 7.67(4.72-10.62) | 1.92(0.40-3.44) | 11.56(8.02-15.10) | 3.19(1.24-5.14) |
| 8 | 16.81(12.83-20.79) | 5.31(2.92-7.70) | 5.01(2.69-7.33) | 14.16(10.45-17.87) | 5.60(3.15-8.05) |
| 9 | 11.71(8.34-15.08) | 3.14(1.31-4.97) | 8.57(5.64-11.50) | 12.00(8.60-15.40) | 4.00(1.95-6.05) |
| 10 | 7.92(5.05-10.79) | 3.52(1.56-5.48) | 9.38(6.29-12.47) | 8.80(5.79-11.81) | 2.64(0.94-4.34) |
| 11 | 3.45(1.45-5.45) | 1.25(0.03-2.47) | 16.93(12.81-21.05) | 7.84(4.89-10.79) | 2.19(0.58-3.80) |
| 12 | 2.62(0.83-4.41) | 0.66(0-1.57) | 19.34(14.91-23.77) | 10.49(7.05-13.93) | 4.59(2.24-6.94) |
| 13 | 0.70(0-1.67) | 0.35(0-1.04) | 21.05(16.32-25.78) | 10.18(6.67-13.69) | 3.16(1.13-5.19) |
| 14 | 1.69(0.35-3.03) | 1.13(0.03-2.23) | 28.81(24.09-33.53) | 11.86(8.49-15.23) | 3.39(1.50-5.28) |
| 15 | 1.33(0-2.83) | 0.89(0-2.12) | 27.11(21.30-32.92) | 14.22(9.66-18.78) | 4.89(2.07-7.71) |
| All | 12.51(11.34-13.68) | 3.26(2.63-3.89) | 13.75(12.53-14.97) | 11.17(10.06-12.28) | 3.75(3.08-4.42) |
* Children were considered hyperopic (defined as ≥+1.50 D SE or ≥+2.00 D SE) if one or both eyes were hyperopic;
† myopic (defined as ≤-0.50 D SE) if one or both eyes were myopic;
‡ astigmatism (defined as cylinder powers ≥0.50 DC or ≥1.00 DC) if one or both eyes were astigmatism.
§ 95% CI of the prevalence of refractive errors in the bracket
In order to analyze the possible factors influencing myopia, hyperopia, and/or astigmatism, multiple logistic regression analyses were performed with children's gender, age, and school type as covariates (Table 4). It was found that myopia was correlated with school type (odds ratio [OR]=5.88, P<0.001) and age (OR= 1.50, P<0.001). Gender did not significantly affect the prevalence of myopia (P=0.82). For hyperopia, only age was a statistically significant factor (OR=0.60, P<0.001). Gender (hyperopia ≥ 1.50D SE, P=0.22; hyperopia ≥ 2.00D SE, P=0.77) and school type (hyperopia ≥ 1.50D SE, P=0.67; hyperopia ≥ 2.00D SE, P=0.22) did not correlate with hyperopia prevalence. For astigmatism, only school type was a statistically significant factor (astigmatism ≥ 0.50DC, OR=2.26, P<0.001; astigmatism ≥ 1.00DC, OR=1.84, P=0.04). Table 5 shows the comparisons of different types of astigmatism between the children in academically challenging schools and those in regular school. Gender (astigmatism ≥ 0.50DC, p=0.52; astigmatism ≥ 1.00DC, P=0.66) and age (astigmatism ≥ 0.50DC, P=0.46; astigmatism ≥ 1.00DC, P=0.53) were not statistically significant factors.
Odds Ratios for hyperopia, myopia and astigmatism by Age, Gender, and School type with Cycloplegic Retinscopy
| Hyperopia | Myopia | Astigmatism | |||
|---|---|---|---|---|---|
| ≥ +1.50 D SE | ≥ +2.00 D SE | ≤ -0.50 D SE | ≥ 0.50 DC | ≥ 1.00 DC | |
| Age(yrs) | 0.063***(0.545-0.667) | 0.831**(0.728-0.948) | 1.5***(1.389-1.62) | 0.977(0.918-1.04) | 1.035(0.932-1.149) |
| Boy/girl | 1.3(0.852-1.986) | 1.112(0.553-2.239) | 0.96(0.679-1.357) | 1.121(0.795-1.581) | 1.139(0.642-2.022) |
| Academically challenging /regular school | 0.911(0.595-1.394) | 1.547(0.769-3.113) | 5.889***(4.08-8.499) | 2.257***(1.596-3.191) | 1.838*(1.033-3.269) |
Data are given as adjusted odds ratios (95% confidence interval).
*P<0.05.
**P<0.01.
***P<0.001.
Prevalence of astigmatism by different types (%)
| School type | Hyperopic astigmatism | Myopic astigmatism | Mixed astigmatism | ||
|---|---|---|---|---|---|
| ≥ +0.50 DC | ≥ +1.00 DC | ≤ -0.50 DC | ≤ -1.00 DC | ||
| Academically challenging | 13.51(10.37-16.63) | 4.79(2.84-6.76) | 8.71(6.12-11.28) | 4.79(2.84-6.76) | 1.96(0.69-3.23) |
| Regular | 6.91(4.86-8.94) | 1.69(0.65-2.73) | 2.76(1.55-4.25) | 1.69(0.65-2.73) | 1.01(0.2-1.8) |
| p | < 0.001 | 0.004 | < 0.001 | 0.004 | 0.198 |
Data are given as the prevalence of refractive errors (95% confidence interval).
DISCUSSION
In the present study, Yongchuan District was chosen for this study because its population, location, and socio-economic development level were representative of Western China. Among 3469 children selected, we examined 3070 (88.50%), a high participating rate that ensured the data quality of this study. Several reasons contributed to the success of our study. Historically, as there are few optometrists and ophthalmologists in Yongchuan District, our efforts were well accepted by parents and children. Local governments, the Health Bureau and Education Commission in Yongchuan District, and school authorities widely supported this study. Additionally, the medical team set up a checkpoint in every sampled village at convenient locations to facilitate the study. Most subjects actively participated in the study and eye examinations, and we only compensated a few subjects who initially hesitated to participate in examinations for their time.
In the study, the numbers of the subjects of 6-year-olds and 15-year-olds were relatively smaller than other age groups. The reasons may be that 6-year-olds were less likely to cooperate with an eye exam and many 15-year-olds were unwilling to delay their school work (cycloplegia could cause difficulties in reading and writing for up to two days).
The refractive distribution in the 6-8-year-old group was close to a normal distribution situated toward emmetropia and hyperopia diopter ranges. Although most children had emmetropia and hyperopia in the 9-12 years and 13-15 years age groups, increased myopia in those age groups led to negatively skewed distributions. This observation was similar to Elvis's study in Australian children [22]. The distributions of refractive frequency for various ages displayed a clear change in shape. The pattern of refractive distribution at every age, indicated that, from age 8, the distribution became negatively skewed: age 8's distribution was only slightly skewed negatively (-0.43), and this skewness became more prominent from age 9 (-2.34). Therefore, we speculate that the distribution shift from positive-skewed to negative-skewed happens around age 8-9 and that, since this shift could be explained by an increased in myopia, ages 8 and 9 are the critical ages for occurrence of myopia. Similarly, we found that age had a significant influence on the prevalence of hyperopia and myopia. As age increased, the prevalence of hyperopia significantly decreased and the prevalence of myopia increased. Based on the definitions of hyperopia (≥+2.00 DS) [23, 24] and myopia (≤-0.50 D SE) [22, 23, 24], the occurrences of hyperopia was greater than myopia in ages 6, 7, and 8 while the occurrences of myopia became greater than hyperopia in age 9 and onward. This shift in myopia occurrence further demonstrate that ages 8 and 9 are critical ages for the refractive distribution. Therefore, more attention should be paid to 8-9-year-olds, in order to delay the occurrence and progression of myopia.
The overall prevalence of myopia was 13.75%, lower than the 16.2% reported in Shunyi County, Beijing [8] and 35.1% reported in Liwan District, Guangzhou [10]. Even though ethnicity was similar in the three regions, geographic locations and economic developments were different. Therefore, we infer that environmental factors may influence the occurrence and development of myopia. Several reasons may contribute to the lower prevalence of myopia in the Yongchuan District. Compared with Beijing and Guangzhou, Yongchuan District is located in Western China, where children's learning intensity was generally lower and video-contacting time was shorter. Furthermore, Western China has more green plants, so the school-age children in this region were closer to nature.
To further prove the effects of environmental factors on refractive errors' prevalence, we compared the prevalence in children from academically challenging schools to regular schools in the same administrative area. We discovered that academically challenging schools had more myopic children (32.68%) than the regular schools (9.78%). To explain this finding, we added up school students' average reading and writing times based on course schedule, counseling after class, and homework time (Table 6). Our investigation showed that children in academically challenging schools spent more time reading and writing than those in regular schools. In Grades 1-3, the study time differences could be up to 107 minutes per day, and in Grades 4-6 and Grades 7-9, the study time differences could be up to 160 and 224 minutes per day. The result reflected a close relationship between study intensity and myopia. Near-work activity may contribute to the development of myopia. Similar results were obtained from researches in Singapore [25], Israel [26], rural area in Northern China [27], HongKong [28], and Orinda [29]. The myopia prevalence's comparison between academically challenging schools and regular schools demonstrated how environmental factors may alter refractive distribution.
Comparison of near-work activity between academically challenging school and regular school
| Grades 1-3 | Grades 4-6 | Grades 7-9 | ||||
|---|---|---|---|---|---|---|
| Academically challenging | Regular | Academically challenging | Regular | Academically challenging | Regular | |
| Study time in class (minutes /day) | 200 | 160 | 240 | 200 | 280 | 280 |
| Self-study time at school (minutes /day) | 0 | 0 | 0 | 0 | 120 | 60 |
| Time for homework after class (minutes /day) | 105 | 50 | 135 | 75 | 260 | 120 |
| Time for computer classes (minutes /week) | 60 | 0 | 60 | 0 | 120 | 0 |
| Total time (minutes /day) | 317 | 210 | 435 | 275 | 684 | 460 |
Study time in class: times when the teachers were actually lecturing in class.
Self-study time at school: sometimes teachers gave additional lectures while other times the students studied themselves.
Homework time outside class: times that the students spent outside school to finish up homework.
One of our most significant findings was the relationship between school type and the astigmatism prevalence. A challenging school refers to the one with skilled teachers, good infrastructure, much more investment from local government than non-challenging schools, and high university enrolment rates. Compared to a general school, a challenging school has a more competitive learning environment. This may encourage the enrollment of more talented students and may appeal to teachers with additional qualifications. Moreover, both teachers and students live stressful lives in the challenging school. There are more demands placed on teachers to produce students with good academic qualifications while there is more homework for students. Comparing astigmatism prevalence between academically challenging and regular schools, we discovered that the prevalence rates of myopic astigmatism and hyperopic astigmatism in academically challenging schools were significantly higher than those in regular schools. Furthermore, mild astigmatisms (≥ 0.50DC, P<0.001) between schools varied more significantly than moderate astigmatism (≥ 1.00DC, P=0.004). As mentioned above, students from academically challenging schools spend much more time reading and writing than those from regular school. We speculate that prolonged lowering of the upper eyelid during reading and writing can cause pressures on eyeballs, specifically corneas. These pressures may result in mild morphological changes on corneas which result in hyperopic and myopic astigmatism, especially mild astigmatism. Several research studies proved that eyelid's pressures such as granuloma, chalazia [30, 31], and congenital ptosis [32, 33] can contribute to astigmatism [34]. These findings support our inference. We therefore conclude that near-work activity may be one of the factors contributing to astigmatism.
There was no difference in the mixed astigmatic prevalence between academically challenging schools (n1) and regular schools (n2) (χ2=1.658, P=0.198). This observation could be due to the extremely small number of students with mixed astigmatism (n1=9, n2=6). Therefore more data is needed to support these findings.
In this study, gender did not correlate with the prevalence of refractive errors, even in academically challenging schools and regular schools. Research in Nepal [11], Chile [15] and Japan [7] produced similar results.
Several limitations of this study are noted. This study was limited by using only retinoscopy during refraction examination, which could lead to observer bias. The lack of supporting data on autorefraction [35], axial length, and keratometry, due to the inconvenience in transporting auxiliary equipment on rugged mountain roads in the study regions, should be considered a weakness of this study.
In summary, our results indicate that an increase in studying intensities could lead to increases in myopia and astigmatism occurrences, but it is not clear whether the occurrence increases were caused by prolonged near-work activities or reduced outdoor activities because of increased studying intensity, and further studies are needed to ascertain the most significant contributors. A recent report [36](Rose et al., 2008) suggests that outdoor time is protective against the development of myopia, rather than near-work causing myopia. We emphasize the importance of reducing near-work activity and preserving outdoor time in the setting of academically demanding schedules to reduce the prevalence of myopia.
Acknowledgements
We thank Prof. Jia-Liang Zhao for valuable discussions and the following individuals for excellent assistance in the planning and execution of this study: Ming-Gang Wang, Chongqing Municipal Government; Chang-Yu Liu, Commerce Department; Fu-Rong Zhang and Da-Bin Yuan, Teaching Committee of Chongqing Yongchuan District; Guo-Hua Zhao, Food College of Southwest University; Tao Yu, Southwest Hospital, Southwest Eye Hospital, Third Military Medical University; and Zi-Yue Wang, University of Texas, Austin, USA. The authors indicate no financial conflict of interest.
This study supported in part by a grant (2007CE9070) from the Chongqing Science and Technology Commission.
Competing Interests
None.
References
1. Prevalence of refractive error in school children of Karachi. Prevalence of refractive error in school children of Karachi. J Pak Med Assoc. 2008;58:322-325
2. Pizzarello L, Abiose A, Ffytche T. et al. Vision 2020: the right to sight: a global initiative to eliminate avoidable blindness. Arch Ophthalmol. 2004;122:615-620
3. He M, Xu J, Yin Q, Ellwein LB. Need and challenges of refractive correction in urban Chinese school children. Optom Vis Sci. 2005;82:229-234
4. Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ. 2001;79:237-243
5. Zhan MZ, Saw SM, Hong RZ. et al. Refractive errors in Singapore and Xiamen, China--a comparative study in school children aged 6 to 7 years. Optom Vis Sci. 2000;77:302-308
6. Arnold RW, Ruben J, Donahue SP, AAPOS Vision Screening Committee. Korean kindergarten vision screen programme. Br J Ophthalmol. 2005;89:392- 393
7. Yamashita T, Watanabe S, Ohba N. A longitudinal study of cycloplegic refraction in a cohort of 350 Japanese schoolchildren. Anisometropia. Ophthalmic Physiol Opt. 1999;19:30-33
8. Zhao J, Pan X, Sui R. et al. Refractive error study in children: Results from Shunyi district, China. Am J Ophthalmol. 2000;129:427-435
9. Zhao J, Mao J, Luo R, Li F, Munoz SR, Ellwein LB. The progression of refractive error in school-age children: Shunyi District, China. Am J Ophthalmol. 2002;134:735-743
10. He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci. 2004;45:793-799
11. Pokharel GP, Negrel AD, Munoz SR, Ellwein LB. Refractive error study in children: results from Mechi Zone, Nepal. Am J Ophthalmol. 2000;129:436-444
12. Goh PP, Abqariyah Y, Pokharel GP, Ellwein LB. Refractive error, and visual impairment in school age children in Gombark district, Malaysia. Ophthalmol. 2005;112:678-685
13. Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Muñoz SR, Pokharel GP, Ellwein LB (). Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;4:615-622
14. Dandona R, Dandona L, Naduvilath TJ, Srinivas M, McCarty CA, Rao GN. Refractive Errors in an urban population in Southern India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci. 1999;40:2810-2818
15. Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB. Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol. 2000;129:445-454
16. Mohammad K, Mohammadreza G, Mohammadi ZI. Prevalence of Refractive Errors in Primary School Children [7-15 Years] of Qazvin City. European Journal of Scientific Research. 2009;28:174-185
17. He M, Zheng Y, Xiang F. Prevalence of myopia in urban and rural children in mainland China. Optom Vis Sci. 2009;86:40-44
18. National Bureau of Statistics of China. China statistical yearbook 2003 [in Chinese]. Beijing: China Statistics Press. 2003:100-102
19. Chongqing Municipal Bureau of Statistics. Chongqing statistical yearbook 2004 [in Chinese]. Beijing: China Statistics Press. 2004:58-59
20. Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive error study in children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 2000;129:421-426
21. Ferris FL III, Bailey I. Standardizing the measurement of visual acuity for clinical research studies: Guidelines from the Eye Care Technology Forum. Ophthalmology. 1996;103:181-182
22. Ojaimi E, Rose KA, Morgan IG. et al. Distribution of ocular biometric parameters and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci. 2005;46:2748-2754
23. Anera RG, Soler M, de la Cruz Cardona J, Salas C, Ortiz C. Prevalence of refractive errors in school-age children in Morocco. Clinical and Experimental Ophthalmology. 2009;37:191-196
24. Robaei D, Kifley A, Rose KA, Mitchell P. Refractive error and patterns of spectacle use in 12-year-old Australian children. Ophthalmology. 2006;113:1567-1573
25. Saw SM, Chua WH, Hong CY. et al. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci. 2002;43:332-339
26. Zylbermann R, Landau D, Berson D. The influence of study habits on myopia in Jewish teenagers. J Pediatr Ophthalmol Strabismus. 1993;30:319-322
27. Saw SM, Hong RZ, Zhang MZ. et al. Near-work activity and myopia in rural and urban schoolchildren in China. J Pediatr Ophthalmol Strabismus. 2001;38:149-155
28. Wong L, Coggon D, Cruddas M, Hwang CH. Education, reading, and familial tendency as risk factors for myopia in HongKong fishermen. J Epidemiol Community Health. 1993;47:50-53
29. Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633-3640
30. Nisted M, Hofstetter HW. Effect of chalazion on astigmatism. Am J Optom Physiol Opt. 1974;51:579-582
31. Bohigian GM. Chalazion: a clinical evaluation. Ann Ophthalmol. 1979;11:1397-1398
32. Cadera W, Orton RB, Hakim O. Changs in astigmatism after surgery for congenital ptosis. J Pediatr Ophthalmol Strabismus. 1992;29:85-88
33. Holck DEE, Dutton JJ, Wehrly SR. Changes in astigmatism after ptosis surgery measured by corneal topography. Ophthal Plast Reconstr Surg. 1994;10:241-246
34. Grosvenor T. Etiology of astigmatism. Am J Optom Physiol Opt. 1978;55:214-218
35. Erdurmus M, Yagci R, Karadag R, Durmus M. A comparison of photorefraction and retinoscopy in children. J AAPOS. 2007;11:606-611
36. Rose KA, Morgan IG, Ip J. et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279-1285
Author contact
![]() Corresponding author: Dr Zheng-Qin Yin, Southwest Hospital, Southwest Eye Hospital, Third Military Medical University, Gaotanyan 30, Shapingba District, Chongqing 400038, China; Tel: +86-23-68754401; Fax: +86-23-63622874; Email: happy20070801cn
Corresponding author: Dr Zheng-Qin Yin, Southwest Hospital, Southwest Eye Hospital, Third Military Medical University, Gaotanyan 30, Shapingba District, Chongqing 400038, China; Tel: +86-23-68754401; Fax: +86-23-63622874; Email: happy20070801cn

 Global reach, higher impact
Global reach, higher impact